
 Background: Some of the major take home points from the sepsis trilogy of studies recently published (ProCESS, ARISE, and ProMISe) was that early identification of patients with sepsis, early intravenous fluids, and timely, appropriate broad-spectrum antibiotics is key to decreasing morbidity and mortality. In 2006 a study by Kumar et al [3] showed a 7.6% increase in mortality in patients with sepsis for every hour of delay after the onset of shock, but this finding has not been reproduced. In fact, the results of timing of antibiotic administration on outcomes have been all over the map. Regardless, the Surviving Sepsis Campaign still has very specific recommendations regarding the timing of antibiotics. And even more painful is that metrics for the quality of care of patients with severe sepsis and septic shock are now recognizing these recommendations as core measures.
Background: Some of the major take home points from the sepsis trilogy of studies recently published (ProCESS, ARISE, and ProMISe) was that early identification of patients with sepsis, early intravenous fluids, and timely, appropriate broad-spectrum antibiotics is key to decreasing morbidity and mortality. In 2006 a study by Kumar et al [3] showed a 7.6% increase in mortality in patients with sepsis for every hour of delay after the onset of shock, but this finding has not been reproduced. In fact, the results of timing of antibiotic administration on outcomes have been all over the map. Regardless, the Surviving Sepsis Campaign still has very specific recommendations regarding the timing of antibiotics. And even more painful is that metrics for the quality of care of patients with severe sepsis and septic shock are now recognizing these recommendations as core measures.
Current Surviving Sepsis Guideline Recommendations (2013) [2]:
- Administer antibiotics within 3 hours of ED triage
- Administer antibiotics within 1 hour of severe sepsis (Level 1B)/septic shock (Level 1C) recognition
What Article is Being Reviewed?
Sterling SA et al. The Impact of Timing of Antibiotics on Outcomes in Severe Sepsis and Septic Shock: A Systematic Review and Meta-Analysis. Critical Care Medicine 2015; 43(9): 1907 – 15. PMID: 26121073
What They Did:
- Meta-analysis of 11 publications (16,178 patients) looking at the association between timing of antibiotic administration and mortality in severe sepsis and septic shock
- Antibiotic timing defined as:
- ≤3 hours vs >3 hours from triage
- ≤1 hour vs > 1 hour from shock/severe sepsis recognition
- Also performed sensitivity analysis of the effect of time to antibiotics from severe sepsis/shock recognition in hourly increments
- Excluded: Neutropenic and Immunosuppressed patients
Primary Outcome:
- Mortality
Results:
- Antibiotic timing from triage (6 of 11 studies):
- ≤3 hours –> 10,208 patients –> 2,574 died
- >3 hours –> 5,970 patients –> 1,793 died
- Pooled OR 1.16 (95% CI, 0.92 – 1.46; p = 0.21)
- Antibiotic timing from shock/severe sepsis recognition (8 of 11 studies):
- ≤1 hour –> 335 patients –> 1,174 died
- > 1hour –> 7,682 patients –> 3,581 died
- Pooled OR 1.46 (95% CI, 0.89 – 2.40; p = 0.13)
- Sensitivity Analysis of the Effect of time to Antibiotics from severe sepsis/shock recognition
- <1 hour –> 2,318 patients –> 848 deaths
- 1 – 2 hours –> 1,298 patients –> 471 deaths
- 2 – 3 hours –> 853 patients –> 323 deaths
- 3 – 4 hours –> 615 patients –> 245 deaths
- 4 – 5 hours –> 453 patients –> 193 deaths
- > 5 hours –> 2,386 patients –>1,537 deaths
- No statistically significant increase in the pooled ORs for each hourly incremental delay in antibiotic administration
Strengths:
- Utilized a scoring system to determine study quality
- All studies included were considered moderate to high quality
Limitations:
- As with any meta-analysis the pooled results are only as good as the individual studies included in the analysis. Remember crap in = crap out!!
- The study did not include any randomized controlled trials (highest level of evidence) as none have ever been performed.
- Several studies were excluded, as they did not contain all the data necessary to evaluate time of antibiotic administration on mortality. The authors did attempt to contact original authors three different times, but only received responses from half the authors. Having these results, could potential alter the results of this study
- Studies included were not limited to studies of appropriate or effective antibiotic use. In other words, included patients may have received inappropriate antibiotics or had resistant organisms, which could also alter results of this study.
Discussion:
- It is obvious that failure to administer effective broad-spectrum antibiotics will be detrimental to patient outcomes, but the exact time when this occurs is still not known, most likely because sepsis has a complex pathophysiology that has a spectrum of severity as opposed to actual categories of disease.
- SIRS criteria was created in 1992 as a consensus statement from the Society of Critical Care Medicine and American College of Chest Physicians. Using SIRS criteria alone misclassifies 23.4% of patients [4] and 15% of patients will not meet definitions of severe sepsis and septic shock until after 3 hours from ED arrival [5]. If this holds true then is time to antibiotics from triage a reliable quality metric?
- It is also important to state that, this study is not saying early antibiotic administration is not important in severe sepsis and septic shock, but instead that this arbitrary, non-evidence based time to antibiotic administration time of 3 hours (triage) or 1 hour (severe sepsis/shock) should not be a metric for quality of care.
Comments from Twitter:
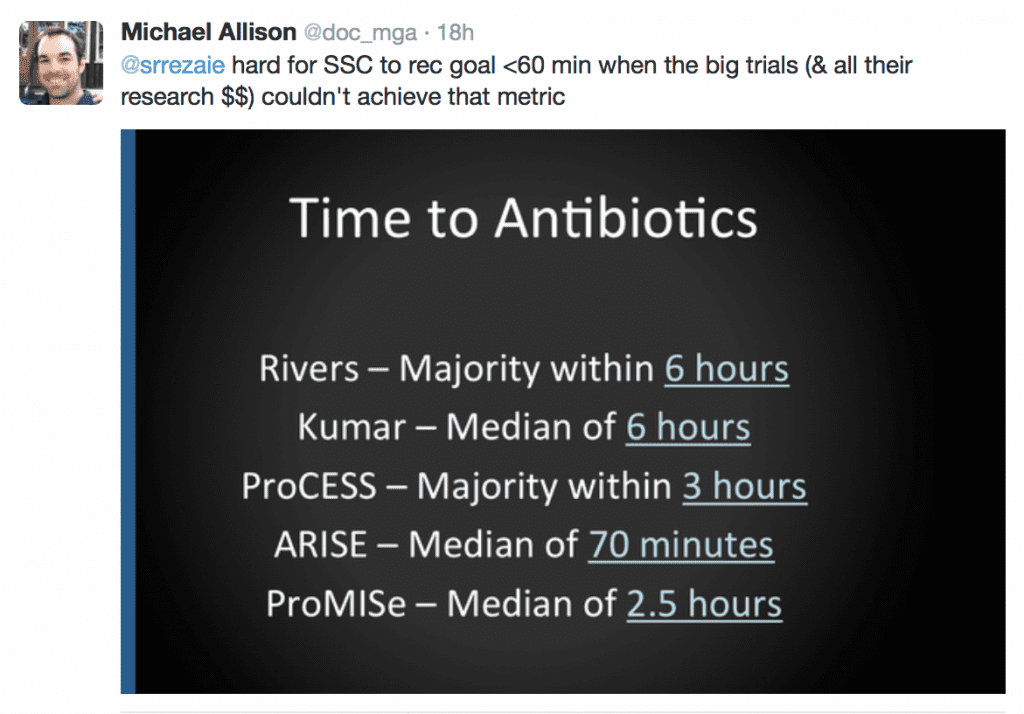
Tweet and image from Michael Allison (@doc_mga)
Clinical Take Home Point: There is no data driven or evidence based research that demonstrates time to antibiotic administration in severe sepsis/septic shock as a reliable quality metric. Sepsis is a heterogeneous spectrum of illness and as such, one size does not fit all.
References:
- Sterling SA et al. The Impact of Timing of Antibiotics on Outcomes in Severe Sepsis and Septic Shock: A Systematic Review and Meta-Analysis. Critical Care Medicine 2015; 43(9): 1907 – 15. PMID: 26121073
- Dellinger RP et al. Surviving Sepsis Campaign: International Guidelines for Management of Severe Sepsis and Septic Shock: 2012. Crit care Med 2013; 41(2): 580 – 637. PMID: 23353941
- Kumar A et al. Duration of Hypotension Before Initiation of Effective Antimicrobial Therapy is the Critical Determinant of Survival in Human Septic Shock. Crit Care Med 2006; 34: 1589 – 96. PMID: 16625125
- Venkatesh et al. Time to Antibiotics for Septic Shock: Evaluating a Proposed Performance Measure. Am J Emerg Med 2013; 31: 680 – 683. PMID: 23380106
- Villar et al. Many Emergency Department Patients with Severe Sepsis and Septic Shock do not Meet Diagnostic Crteria Within 3 Hours of Arrival. Ann Emerg Med 2014; 64: 48 -54. PMID: 24680548
For More Thoughts on This Checkout:
- John Greenwood at Critical Care Project: Personalized Resuscitation Metrics – Sepsis, Early Antibiotics, and the Dilemma of Speed vs. Accuracy
- Josh Farkas at PulmCrit: The Fallacy of Time-to-Intervention Studies
Post Peer Reviewed By: Anand Swaminathan (Twitter: @EMSwami)
The post Time to Antibiotics in Sepsis: A Metric Not Supported by “High Quality” Evidence appeared first on REBEL EM - Emergency Medicine Blog.
