In Emergency Medicine, we are like Goldilocks when it comes to many things: We don’t like a patient’s PaO2 to be too high or too low. We don’t like the bed too high or too low when we intubate. We get concerned when we see a potassium that is too high or too low. The Goldilocks principle is also true of opening pressures on a lumbar puncture (LP). This post will discuss what the opening pressure means, and a differential diagnosis for when it is too high or too low and even when it is in the normal range.
Consider a case in which you are doing an LP for a patient with an abrupt onset headache who had a negative head CT. You nail the LP, but forget to measure the opening pressure. What do you do when the cerebrospinal fluid (CSF) lab studies come back with a champagne tap? You may consider further imaging with an MRI, or symptomatic management and observation. However, in some cases measuring the opening pressure could mean the difference between diagnosing or missing entities like CSF leaks, cerebral venous thrombosis, and idiopathic intracranial hypertension (IIH).

What Determines the Opening Pressure?
The opening pressure (OP) in a healthy individual is determined by the rates of production and drainage of CSF. It is produced from choroid plexus in the ventricles. It flows from the lateral ventricles through the foramina of Monro into the 3rd ventricle, and from there to the 4th ventricle and out the foramina of Luschka and Magendie into the subarachnoid space around the brain and spinal canal. It is reabsorbed by the arachnoid villi in the superior sagittal sinus into the venous system where it drains into the jugular veins. Disorders that dysregulate production, absorption, or flow of the CSF can cause an elevated or decreased OP. In addition, infection, inflammation, and hemorrhage can also increase the OP. Adults have about 150 cc of CSF, and it is continuously produced and reabsorbed at a rate of about 20 cc/hr. The fast rate of production and accumulation explains why patients with IIH typically only get a few hours of relief after a ‘therapeutic’ large volume tap.
What is a Normal Opening Pressure?
The normal range for CSF is reported differently in various sources, with most reporting a normal range of 7-18 cmH2O in adults,1 though some consider the normal range 5-25 cmH2O.2 However, a pressure >25 cmH2O or <5 cmH2O should certainly prompt you to look for a source.
When the OP is Too High
There are a number of causes for an elevated OP that range from the acute, life threatening, to the more indolent:
- Meningitis: OP can be high particularly in bacterial meningitis, but also can be high in viral and fungal meningitis or neurosyphilis.
- Idiopathic Intracranial Hypertension (IIH): Formerly called pseudotumor cerebri, it causes an elevated OP without any mass lesions.
- Subarachnoid hemorrhage: Can cause an elevated OP, but it may depend on the timing and severity
- Brain abscesses
- Intracranial vasculitis
- Encephalitis
- Meningeal carcinomatosis: OP can be very high, even as far as overflowing the pressure manometer despite the top extension piece
- Guillain-Barre syndrome
- Intracranial masses
- Venous sinus thrombosis causing decreased CSF reabsorption
- Jugular vein compression from a neck mass or post-surgical scarring
- Cerebral edema: Could be post-traumatic, from hypoxia, or from a stroke
- Choroid plexus papilloma causing increased CSF production is a rare cause of increased OP
When the OP is Too Low
- There may be a mass or abscess blocking outflow of the CSF into the spinal canal
- CSF leak which could be post-LP, post-traumatic, post-surgical or spontaneous, the latter occurring rarely, but more commonly in older adults)
When the OP is Normal
A normal OP can be a good sign, but of course has to be taken within the full clinical context of the history, physical exam, and other results as it can be normal in a number of CNS disease states. All of the following conditions may have a normal CSF OP:
- Aseptic meningitis
- Cerebral epidural abscess
- Normal pressure hydrocephalus
- Intracranial masses not involving or affecting CSF flow or causing significant edema
- Multiple sclerosis
False Positives
Several things can make the OP falsely high. If the patient is straining or performing a Valsalva, or pulling their knees up tightly, it could falsely increase the OP. Also, the opening pressure should be measured in the left lateral decubitus position. It will measure falsely high if measured in the sitting position. There is some controversy about whether body mass index (BMI) contributes to a higher OP. There does seem to be a trend for higher OPs in obese patients but the difference is small and not statistically significant.3
False Negatives
If patients hyperventilate, this can cause the OP to be lower.4 Patients who are dehydrated or hypotensive may also have a decreased OP. This is not actually a false negative, because it is a true low OP. However, it is low because of another systemic problem, and not a specific CNS disorder.
When do you need a head CT before an LP?
The LP is useful for diagnosing meningitis, subarachnoid hemorrhage, and other auto-immune or inflammatory disorders. However, the LP will obviously not be appropriate for diagnosing a brain mass, a stroke, or a skull fracture. In general, when you are suspecting any of these based on the history and physical, the patient should have appropriate imaging first. Here is a quick mnemonic for patients in whom you should consider a CT before an LP, with the acronym “TAP AS IF”.
- Trauma
- Age > 60
- Papilledema (or other sign of increased ICP)
- Altered mental status
- Seizure
- Immunocompromised (HIV/AIDS)
- Focal neurologic deficits such as hemiparesis or new anisocoria, which can be a sign of impending herniation, typically accompanied by severe altered mental status.
If the patient has an obvious source of their symptoms on CT, such as a mass, hematoma, fracture, or abscess, then the LP can be deferred if the findings explain the clinical history. If they have signs of midline shift, obstructive hydrocephalus, or cerebral edema, then an LP should be avoided.
Summary and Recommendations
- Always measure an opening pressure when doing an LP. Failing to do so could mean missing a clue to the diagnosis.
- Include the opening pressure value in your data set to help determine the cause of a patient’s symptoms.
- Remember the TAP AS IF mnemonic to help remember whether a head CT may be helpful before the LP.
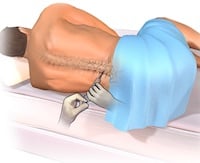
Top image 5
-
References
1.Reichman E F, Polglaze K, Euerle B. Neurological and Neurosurgical Procedures: Lumbar Puncture. In: Emergency Medicine Procedures. McGraw Hill; 2013:747-761. -
2.Lee S, Lueck C. Cerebrospinal fluid pressure in adults. J Neuroophthalmol. 2014;34(3):278-283. [PubMed]
-
3.Whiteley W, Al-Shahi R, Warlow C, Zeidler M, Lueck C. CSF opening pressure: reference interval and the effect of body mass index. Neurology. 2006;67(9):1690-1691. [PubMed]
-
4.Seehusen D, Reeves M, Fomin D. Cerebrospinal fluid analysis. Am Fam Physician. 2003;68(6):1103-1108. [PubMed]
-
5.Blausen.com staff. Medical gallery of Blausen Medical 2014. . WikiJournal of Medicine. https://commons.wikimedia.org/wiki/File:Blausen_0617_LumbarPuncture.png. Published 2014. Accessed February 11, 2017.
Author information
The post Tips for Interpreting the CSF Opening Pressure appeared first on ALiEM.

