
 Background: Epistaxis is a common Emergency Department (ED) complaint with over 450,000 visits per year and a lifetime incidence of 60% (Gifford 2008, Pallin 2005). Standard anterior epistaxis treatment consists of holding pressure, use of local vasoconstrictors, topical application of silver nitrate and placement of an anterior nasal pack. ED patients with epistaxis often fail conservative management and end up with anterior nasal packs which are uncomfortable. This is even more common in the group of patients who are taking antiplatelet agents like aspirin or clopidogrel. Recently, the use of topical tranexamic acid (TXA) has been described in patients with anterior epistaxis with shorter time to epistaxis control and shorter ED length of stay (Zahed 2013). However, prior studies have not focused specifically on patients taking antiplatelet agents.
Background: Epistaxis is a common Emergency Department (ED) complaint with over 450,000 visits per year and a lifetime incidence of 60% (Gifford 2008, Pallin 2005). Standard anterior epistaxis treatment consists of holding pressure, use of local vasoconstrictors, topical application of silver nitrate and placement of an anterior nasal pack. ED patients with epistaxis often fail conservative management and end up with anterior nasal packs which are uncomfortable. This is even more common in the group of patients who are taking antiplatelet agents like aspirin or clopidogrel. Recently, the use of topical tranexamic acid (TXA) has been described in patients with anterior epistaxis with shorter time to epistaxis control and shorter ED length of stay (Zahed 2013). However, prior studies have not focused specifically on patients taking antiplatelet agents.
Article:
Zahed R et al. Topical Tranexamic Acid Compared With Anterior Nasal Packing for Treatment of Epistaxis in Patients Taking Antiplatelet Drugs: Randomized Controlled Trial. Acad Emerg Med 2017. PMID: 29125679
Clinical Question: Does application of topical TXA result in a higher proportion of patients with anterior epistaxis control at 10 minutes in comparison to anterior nasal packing.
Population: Patients (did not specify adults, pediatrics or both but assumed adults based on text) presenting to the ED of a single academic teaching hospital in Tehran, Iran with acute, new or recurrent ongoing anterior epistaxis who were currently taking antiplatelet drugs (aspirin, clopidogrel or both). Patients were included if they had continued epistaxis after 20 minutes of continued pressure.
Intervention: Tranexamic acid (TXA) soaked cotton pledget (500 mg TXA in 5 ml)
Control: Anterior nasal packing with cotton pledget soaked in epinephrine (1: 100,000) and lidocaine (2%)
Outcomes:
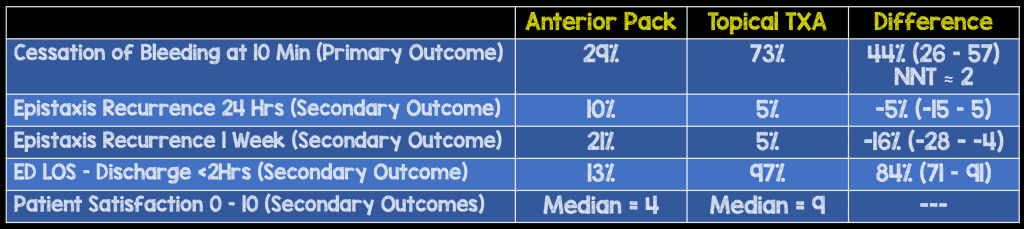
- (Primary): Proportion of patients in each group with stopped bleeding at 10 minutes
- (Secondary): Re-bleeding rate at 24 hours and one-week, ED length of stay (LOS), patient satisfaction
Design: Prospective, randomized, non-blinded, parallel group trial
Excluded: Patients with traumatic epistaxis, current anticoagulant drug use, inherited bleeding disorders, inherited platelet disorders, INR > 1.5, shock, a visible bleeding vessel, a history of renal disease and lack of consent.
Primary Results:
-
Patients enrolled
- n = 384 patients assessed for eligibility
- n = 124 patients who were included and randomized
- No patients lost to follow up for the primary or secondary outcomes
Critical Findings:
Strengths:
- Study asks a clinically relevant question regarding cessation of bleeding in epistaxis
- Data analysts were blinded to allocation
- Surpassed target sample size (57 patients needed in each arm to achieve 80% power to detect 25% difference in primary outcome)
- Follow up was complete (no patients lost)
Limitations:
- Unclear whether cessation at 10 minutes clinically more important than cessation at another interval. Additionally, nasal packing may take longer to achieve hemostasis based on mechanism making this particular comparison (primary outcome) unfair
- Physicians and patients non-blinded to intervention. Researchers indicate that the study wasn’t blinded because pharmacy prepared kits had differing numbers of cotton pledgets and the consistency, color and smell of the medications used for soaking could unblind groups
- Bleeding at 24 hours and one-week assessed in person or by phone. Authors do not specify how many assessed by each method. May introduce recall bias
- Majority of patients on aspirin only (> 80%). Though patients on clopidogrel included, results may not apply as well to this group
Authors Conclusions:
“In our study population, epistaxis treatment with topical application of TXA resulted in faster bleeding cessation, less re-bleeding at 1week, shorter ED LOS, and higher patient satisfaction as compared with ANP. “
Our Conclusions: Topical TXA resulted in a significantly higher rate of cessation of bleeding of anterior epistaxis within 10 minutes of application in comparison to anterior nasal packing in patients on antiplatelet agents (primarily aspirin). ED LOS and patient satisfaction were considerably better in the TXA group as well but these were secondary outcomes. Though this study is too small to comment on safety, there have not been any documented serious adverse effects of this approach in the published literature.
Potential to Impact Current Practice: The use of topical TXA is painless, non-invasive and relatively inexpensive. Providers should consider the use of this approach in patients with anterior epistaxis who fail direct pressure prior to placement of an anterior pack.
Bottom Line: The application of topical TXA appears to be a rapid and affective approach to achieving hemostasis in anterior epistaxis. Future studies should look at longer term outcomes and use in patients on anticoagulants or other antiplatelet agents.
References:
- Gifford TO, Orlandi RR. Epistaxis. Otolaryngol Clin North Am. 2008;41:525-536. PMID: 18435996
- Pallin DJ et al. Epidemiology of epistaxis in US emergency departments, 1992 to 2001. Ann Emerg Med. 2005;46:77-81. PMID: 15988431
- Zahed R et al. A new and rapid method for epistaxis treatment using injectable form of tranexamic acid topically: a randomized controlled trial. Am J Emerg Med 2013; 31: 1389-92. PMID: 23911102
Post Peer Reviewed By: Salim R. Rezaie (Twitter: @srrezaie)
The post Topical TXA in Epistaxis appeared first on REBEL EM - Emergency Medicine Blog.
