
 Background: Post-cardiac arrest patients are among the sickest groups of patients seen in the Emergency Department. They are difficult to study, which leads to endless questions about how to best care for them. Below we address the available evidence on four of these controversies: oxygen therapy, hemodynamic management, cardiac catheterization and head CT. We recognize the limitations to the available data and attempt to offer the best recommendations we can.
Background: Post-cardiac arrest patients are among the sickest groups of patients seen in the Emergency Department. They are difficult to study, which leads to endless questions about how to best care for them. Below we address the available evidence on four of these controversies: oxygen therapy, hemodynamic management, cardiac catheterization and head CT. We recognize the limitations to the available data and attempt to offer the best recommendations we can.
 Oxygen Therapy
Oxygen Therapy
- Avoiding both hypoxia and hyperoxia is important. Hyperoxia may lead to cerebral vascoconstriction and production of free radicals.
- Hyperoxia (PaO2 >300) on first ICU blood gas was associated with increased mortality compared to normoxia and hypoxia (OR 1.8 95%CI 1.5-2.2.) (Kilgannon 2010)
- Titration of oxygen in the pre-hospital period following OHCA was found to not be feasible due to concern for hypoxia, however it is feasible to titrate oxygen safely after arrival in hospital. (Young 2014)
- A Systematic Review and Meta-analysis by Wang et. al. found that post-ROSC hyperoxia was significantly associated with in-hosiptal mortality (OR 1.4) but was not significantly associated with poor neurologic status at hospital discharge. (Wang 2014)
- Bottom line: Target a SpO2 of 92-95%. Titrate down fiO2 to the minimum amount required to achieve this goal as hyperoxia has been associated with worse outcomes
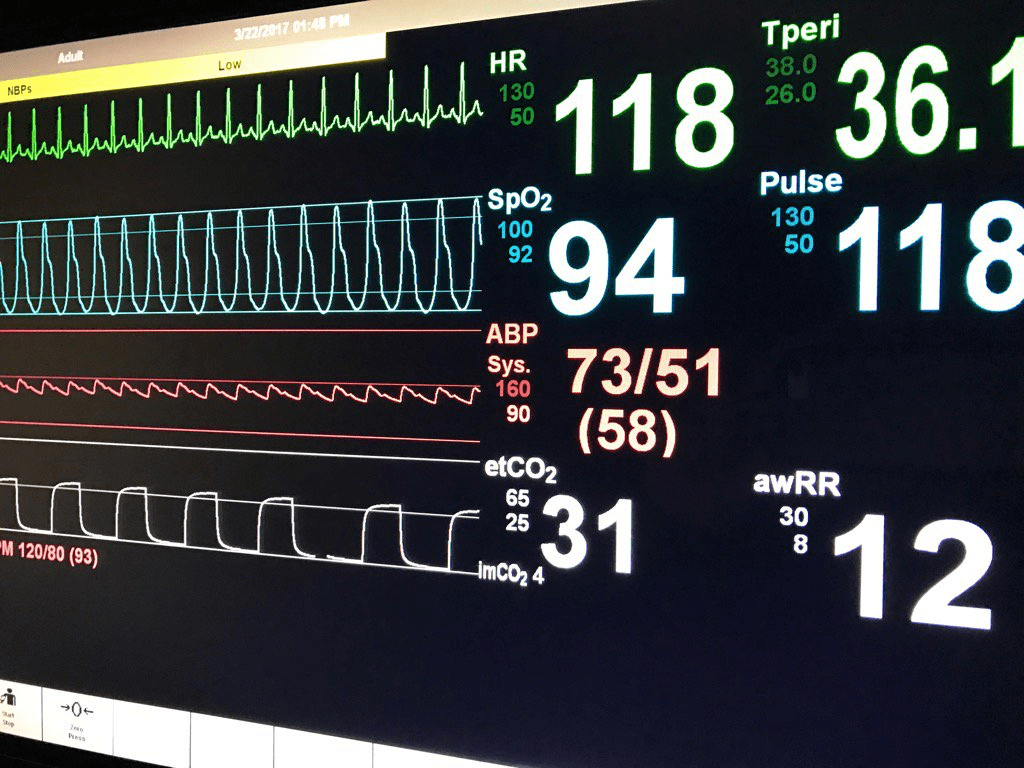 Hemodynamic Management
Hemodynamic Management
- Post-ROSC patients are often hypotensive due to the underlying etiology of cardiac arrest or secondary to ischemia-reperfusion injury
- Blood pressures are likely to drop as the effect of vasoactive substances (most commonly epinephrine) given during cardiac arrest wears off.
- The American Heart Association (AHA) recommends avoiding and immediately correcting hypotension (systolic blood pressure <90 mmHg, MAP <65 mmHg) during postresuscitation care (Class IIb) (Callaway 2015)
- A retrospective study showed that survivors of cardiac arrest had higher MAPs at all time points compared to non-survivors (this is also the case among patients requiring vasoactive agents), suggesting that patients may benefit from a higher goal MAP (>80 mm Hg.) (Beylin 2013)
- There is an ongoing RCT in Belgium (Ameloot 2017) to determine if a target MAP of 85-100 mm Hg in comatose survivors of cardiac arrest has improved outcomes compared to those with a target MAP > 65 mm Hg.
- Bottom line: Avoiding hypotension is important in post-cardiac arrest patients. Although limited, available evidence suggests that a higher goal MAP may improve survival.
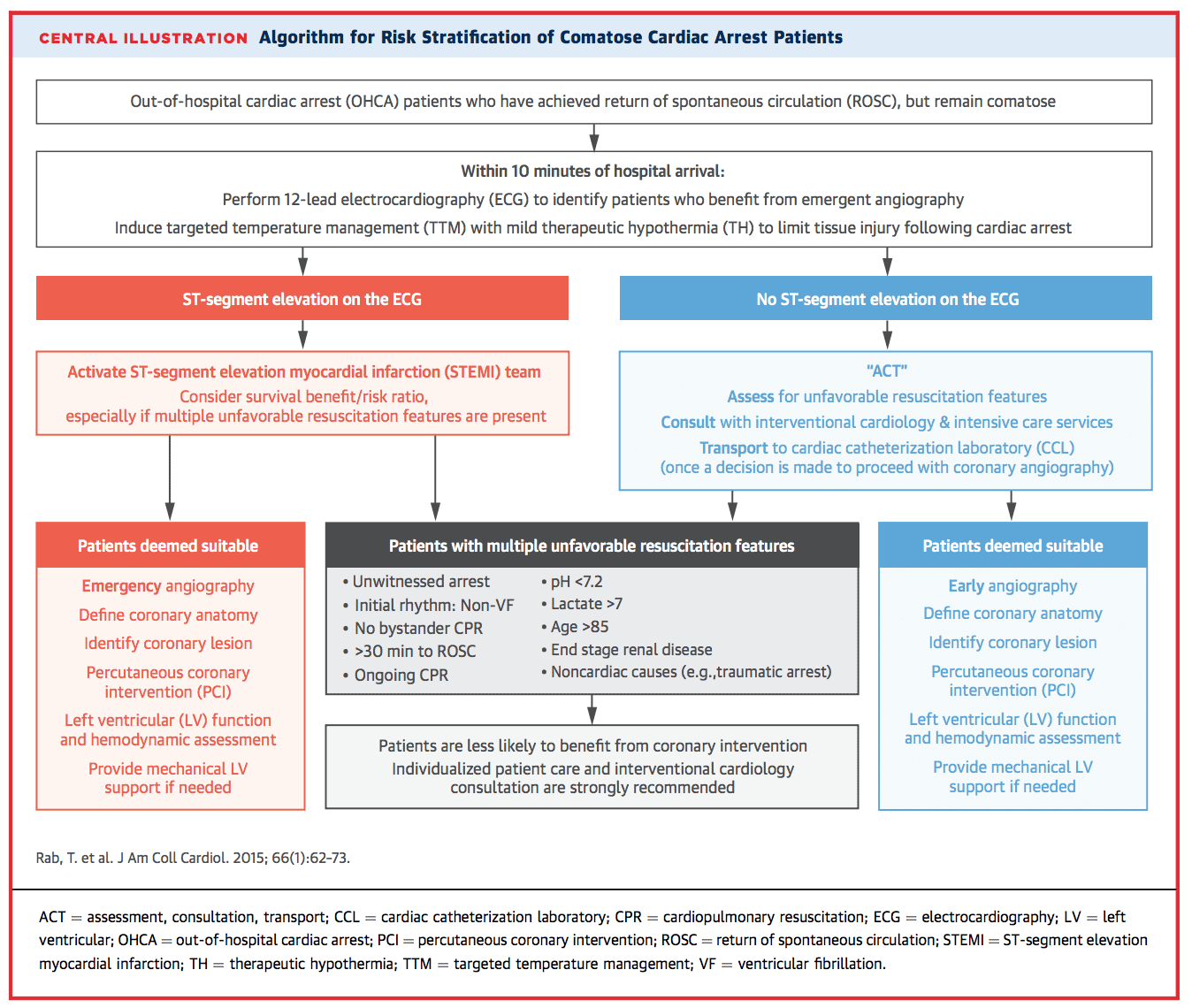
Cardiac Catheterization
- Coronary artery disease is the most common cause of cardiac arrest. However, it remains difficult to predict which patients will benefit from cardiac catheterization after ROSC.
- The AHA recommends emergent coronary angiogram of out of hospital cardiac arrest (OHCA) patients with suspected cardiac etiology of arrest and ST elevation on ECG (Class I). Emergency coronary angiography is reasonable for select (eg, electrically or hemodynamically unstable) adult patients who are comatose after OHCA of suspected cardiac origin but without ST elevation on ECG (Class IIa.) (Callaway 2015)
- >25% of patients without STEMI on their ECG have a coronary occlusion requiring PCI (Hollenbeck 2014)
- Patients who underwent PCI after VF arrest have decreased mortality (OR 0.30.). However more of a benefit was seen in younger patients (Cronier 2011)
- A combination of ECG criteria (ST-elevation and/or depression and/or LBBB and/or non-specific QRS) in post-cardiac arrest patients was 100% sensitive and 45% specific for an ultimate diagnosis of MI (Sideris 2011)
-
A Systematic Review and Meta-analysis of non-randomized controlled studies found that cardiac catheterization was associated with increased survival (OR 2.77) and increase survival with good neurologic outcome (OR 2.20) (Camuglia 2014)
- This review did not control for ECG pattern
- A potential confounder is that patients who had coronary angiogram may have received more attentive care
- Post-VF arrest patients with non-ST elevation in ECG have been found to have better outcomes if coronary angiogram was performed (survival 65.6% vs 28.6% also with better neurologic outcomes among survivors in cath group) (Hollenbeck 2014)
- A recent algorithm advocates for taking into account “Unfavorable Factors” that indicate patient is less likely to benefit from cath when deciding whether to obtain coronary angiogram (Rab 2015)
- Bottom Line: Almost all STEMIs should go to the cath lab immediately. Strongly consider cath in non-STEMI post-ROSC patients if patients had an initial shockable rhythm, there is a high suspicion of coronary etiology or no other etiology of arrest is found. Patients who undergo coronary angiogram seem to do better than those who do not but this may be a result of more attentive/aggressive care.
Non-Contrast Head CT (NCHCT)
- Neurologic emergencies are a common cause of OHCA (2.3-16%) (Reynolds 2017)
-
Up to 79% of head CTs done in post-ROSC patient had abnormalities (Naples 2009)
- CT scans prompted diagnostic and therapeutic changes in 39% of patients in whom it was performed
- Percentages are likely biased as it is unclear what prompted clinicians to perform a NCHCT or to not perform one
-
NCHCT led to changes in management in up to 34% of patients in whom it was performed (Reynolds 2017)
- Changes in management: Triaged to NICU, neurosurgery consult, hyperosmolar therapy, reversal of coagulopathy, prophylactic anti-epileptic therapy, stopping targeted temperature management, placing DNR orders
- However, only 1 out of 20 patients in whom CT changed management survived to discharge (non-neurologically intact patient)
- Bottom Line: NCHCT may change management in post-cardiac arrest patients but it is unclear which patients should have a NCHCT performed.
Take Home Points
- Hyperoxia is associated with worse outcomes, aim for SpO2 92-95% and titrate down fiO2 as soon as possible
- Avoid and correct hypotension. Consider a higher goal MAP such as 80 mm Hg
- Activate the cath lab for STEMIs, patients with an initial shockable rhythm or if you suspect a cardiac etiology of arrest.
- NCHCT may change management in post-cardiac arrest patients but it is unclear which patients should get a NCHCT
Guest Post By
 Alexandra Ortego
Alexandra Ortego
Bellevue/NYU Emergency Department
Read More:
- REBEL EM: Beyond ACLS: From CPR to Cath – The New ACC/AHA Cardiac Arrest Algorithm
- REBEL EM: Cardiac Arrest, Return of Spontaneous Circulation (ROSC) With No ST-Segment Elevation on ECG. Now What?
- EMCrit: Podcast 113 – Post-Arrest Care in 2013 with Stephen Bernard Part I
- EMCrit: Podcast 114 – Post-Arrest Care in 2013 with Stephen Bernard Part II
References:
- Ameloot K et al. Mean arterial pressure of 65 mm Hg versus 85-100 mm Hg in comatose survivors after cardiac arrest: Rational and study design of the Neuroprotect post-cardiac arrest trial. Am Heart J 2017; 191: 91-98. PMID: 28888275
- Beylin ME et al. Higher mean arterial pressure with or without vasoactive agents is associated with increased survival and better neurological outcomes in comatose survivors of cardiac arrest. Intensive Care Med 2013; 39(11): 1981-8. PMID: 23995983
- Callaway CW et al. Part 8: Post-Cardiac Arrest Care. 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015; 132: S465-S482. PMID: 26472996
- Camuglia AC et al. Cardiac catheterization is associated with superior outcomes for survivors of out of hospital cardiac arrest: review and met-analysis. Resuscitation 2014; 85(11): 1533-40. PMID: 25195073
- Cronier P et al. Impact of Routine Percutaneous Coronary Intervention After Out-Of-Hospital Cardiac Arrest Due to Ventricular Fibrillation. Crit Care 2011; 15(3): R122. PMID: 21569361
- Hollenbeck RD et al. Early cardiac catheterization is associated with improved survival in comatose survivors of cardiac arrest without STEMI. Resuscitation 2014; 85(1): 88-95. PMID: 23927955
- Kilgannon JH et al. Association between arterial hyperoxia following resuscitation from cardiac arrest and in-hospital mortality. JAMA 2010; 303(21): 2165-71. PMID: 20516417
- Milne,K. Time to Talk a Littler Nerdy: Managing ROSC part 1. EM:RAP EMA 2017 November. http://www.emrap.org/episode/ema2017november/timetotalka
- Naples, R et al. Cranial computed tomography in the resuscitated patient with cardiac arrest. Am J Emerg Med 2009; 27(1): 63-7. PMID: 19041535
- Rab T et al. Cardiac Arrest: A Treatment Algorithm for Emergent Invasive Cardiac Procedures in the Resuscitated Comatose Patient. JACC 2015; 66 (1): 62 – 73. PMID: 26139060
- Reynolds A et al. Use of early head CT following out-of-hospital cardiopulmonary arrest. Resuscitation 2017; 113: 124-127. PMID: 28057527
- Sideris G et al. Value of post-resuscitation electrocardiogram in the diagnosis of acute myocardial infarction in out-of-hospital cardiac arrest patients. Resuscitation 2011; 82(9): 1148-53. PMID: 21632166
- Wang CH et al. The effect of hyperoxia on survival following adult cardiac arrest: a systematic review and met-analysis of observational studies. Resuscitation 2014; 85(9): 1142-8. PMID: 24892265
- Young P et al. Hyperoxic therapy or normoxic therapy after out-of-hospital cardiac arrest (HOT OR NOT): a randomized controlled feasibility trial. Resuscitation 2014; 85(12): 1686-91. PMID: 25261605
Post Peer Reviewed By: Anand Swaminathan (Twitter: @EMSwami) and Salim Rezaie (Twitter: @srrezaie)
The post Topics in Post-ROSC Care appeared first on REBEL EM - Emergency Medicine Blog.
