
Welcome to another ultrasound-based case, part of the “Ultrasound For The Win!” (#US4TW) Case Series. In this case series, we focus on a real clinical case where bedside ultrasound changed the management or aided in the diagnosis. In this case, an 18-year-old man presents with a sore throat.
Learning Objectives:
- Review the differential for a patient presenting to the ED with throat pain/voice change
- Value of POCUS in evaluating patients with possible peritonsillar abscess (PTA)
- Review advantages and anatomy of ‘telescopic’ view as a potential approach to ultrasound-guided PTA drainage
Case Presentation:
An 18-year-old male with no significant past medical history presents to the emergency department with throat pain for two weeks. He was seen by his primary doctor one week ago with negative strep and monospot testing. He was diagnosed with viral pharyngitis and sent home with instructions for symptomatic care. His symptoms became worse over the last few days with difficulty swallowing, decreased oral intake and fever. He noted the pain was worse on the left side of his throat and that his voice ‘sounded different.’ He denied any drooling, neck stiffness or shortness of breath.
Vitals:
BP: 127/69
HR: 90
RR: 16
O2 sat: 98% RA
Temp: 100.1°F
Differential Diagnosis
- Peritonsillar abscess (PTA)
- Peritonsillar cellulitis (Quinsy)
- Retropharyngeal abscess
- Epiglottitis
- Uvulitis
- Ludwig’s angina
- Tonsillitis/pharyngitis
- Strep, Coxsackie, Adenovirus, EBV, CMV, gonococcal, Candida, primary HIV
Physical Examination:
Physical examination revealed a non-toxic appearing man with no signs of respiratory distress. He had no appreciable facial swelling. His neck was supple with no meningeal signs.
You take a look in his oropharynx and see this –

Inspection of his oropharynx revealed left greater than right tonsillar enlargement with erythema and mild uvular deviation to the right concerning for a peritonsillar abscess. The ED team performed a point-of-care ultrasound to evaluate for a drainable collection.

Ultrasound Image Quality Assurance (QA):
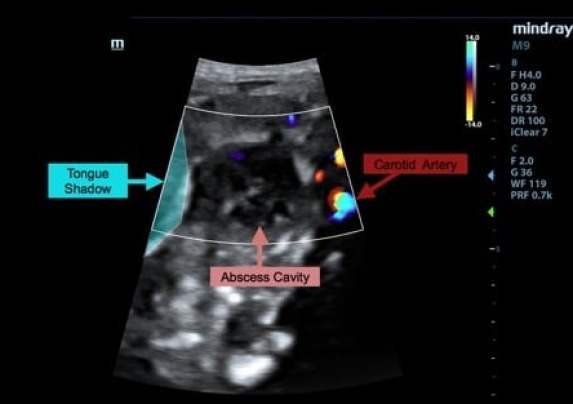
The role of ultrasound in identification and drainage of PTA has been previously established in EM literature.1,2 Ultrasound can differentiate true abscess from cellulitis/phlegmon and help guide your bedside drainage procedure – whether just to identify anatomical landmarks and gauge a safe target for needle insertion or with dynamic guidance through the procedure.3,4 This is generally described using the endocavitary probe. The probe is placed into the mouth against the affected tonsil to visualize any adjacent collection. However, not all EM providers have access to an endocavitary probe. The patient may also have trismus or difficulty opening their mouth wide enough to accommodate the endocavitary probe. Some patients simply cannot tolerate the oral ultrasound. A ‘telescopic’ submandibular ultrasound approach has been described as an alternative to endocavitary views in these patients. The curvilinear probe is positioned medial to the angle of the mandible on the side of the affected tonsil and the probe fanned to localize any collection as well as visualizing the internal carotid artery. This method is dubbed a telescopic approach as the tonsil is being visualized remotely. See figures 3A,B below.

Ultrasound-Guided Needle Aspiration of Peritonsillar Abscess:
A point-of-care ultrasound was performed to look for a drainable peritonsillar collection. No endocavitary probe was available in the ED at the time and we decided to try the telescopic submandibular approach.
Let’s break down the steps:
- The curvilinear probe was placed under the patient’s mandible and the probe fanned to locate the tonsil.
- A hypoechoic collection was visualized adjacent to the left palatine tonsil with positive squish sign consistent with a peritonsillar abscess. Color doppler was utilized to isolate the carotid vessels on the screen and exclude a vascular component to the collection.
- The estimated distance of the drainable collection to the carotid was measured on the screen as well as the estimated size of the abscess cavity. An 18G spinal needle was obtained and the cap cut to act as a needle guard (see Figure 4).
- The area was anesthetized, and needle cap was first used to indent to tonsil in the projected site/plane of needle entry to make adjustments via ultrasound prior to sticking the patient. A partner held the probe in place while the patient held a laryngoscope to comfortably depress the tongue and light the field, leaving the performing physician free to perform the needle aspiration with two hands. Figures 5&6 detail needle insertion/abscess drainage in real time.

Disposition and Case Conclusion:
A needle aspiration procedure yielded 4 cc of purulent material. The patient tolerated the procedure well with no complications. He felt some immediate improvement in his throat pain and dysphagia post-procedure and noted his voice “already sounded more normal.”
Using this submandibular approach we were able to capture real time images of the procedure (Fig. 5, 6). This approach allows constant visualization of the needle tip, the abscess cavity and the carotid throughout the procedure adding an extra layer of patient safety, as well as reassurance for the performing provider.


Take Home Points:
- Point-of-care ultrasound can improve your success in identifying and draining peritonsillar abscess
- The telescopic submandibular approach with the curvilinear probe can be a useful alternative to the endocavitary probe
- As with any procedure, set-up is key – optimizing patient positioning, pain control, equipment/personnel before you start improves your chances of a fast, successful drainage procedure
Read more on ALiEM about how to drain a peritonsillar abscess.
References:
-
1.Costantino T, Satz W, Dehnkamp W, Goett H. Randomized trial comparing intraoral ultrasound to landmark-based needle aspiration in patients with suspected peritonsillar abscess. Acad Emerg Med. 2012;19(6):626-631. https://www.ncbi.nlm.nih.gov/pubmed/22687177.
-
2.Rehrer M, Mantuani D, Nagdev A. Identification of peritonsillar abscess by transcutaneous cervical ultrasound. Am J Emerg Med. 2013;31(1):267.e1-3. https://www.ncbi.nlm.nih.gov/pubmed/22795424.
-
3.Blaivas M, Theodoro D, Duggal S. Ultrasound-guided drainage of peritonsillar abscess by the emergency physician. Am J Emerg Med. 2003;21(2):155-158. https://www.ncbi.nlm.nih.gov/pubmed/12671820.
-
4.Lyon M, Blaivas M. Intraoral ultrasound in the diagnosis and treatment of suspected peritonsillar abscess in the emergency department. Acad Emerg Med. 2005;12(1):85-88. https://www.ncbi.nlm.nih.gov/pubmed/15635144.
Author information
The post Ultrasound for the Win! 18M with dysphagia #US4TW appeared first on ALiEM.

