
 Background Information: The presentation of a patient with syncope to the Emergency Department (ED) can pose a challenge to clinicians as the identification of a serious underlying condition is the priority. Often the original cause of the syncope is difficult to determine in the ED and ultimately results in unnecessary hospitalization. Of all syncope patients evaluated in the ED, 3-5% of them will be found to have a serious condition after ED disposition.1 Furthermore, the literature has shown that hospital admissions due to syncope were associated with low mortality or the need for procedures.2 Emergency physicians are then also posed with the task of determining which patients may be considered low, medium and high risk for a serious outcome. Several risk stratification tools have been developed to help with the identification of these patients, however many of these tools are not validated and very complex, therefore they are not used clinically. The Canadian Syncope Risk Score (CSRS) is among these decision tools, however it has yet to be validated. The authors of this paper sought to conduct a multicenter ED based prospective study to validate this tool and advocate its superior use over some of the other risk stratification tools that currently exist.
Background Information: The presentation of a patient with syncope to the Emergency Department (ED) can pose a challenge to clinicians as the identification of a serious underlying condition is the priority. Often the original cause of the syncope is difficult to determine in the ED and ultimately results in unnecessary hospitalization. Of all syncope patients evaluated in the ED, 3-5% of them will be found to have a serious condition after ED disposition.1 Furthermore, the literature has shown that hospital admissions due to syncope were associated with low mortality or the need for procedures.2 Emergency physicians are then also posed with the task of determining which patients may be considered low, medium and high risk for a serious outcome. Several risk stratification tools have been developed to help with the identification of these patients, however many of these tools are not validated and very complex, therefore they are not used clinically. The Canadian Syncope Risk Score (CSRS) is among these decision tools, however it has yet to be validated. The authors of this paper sought to conduct a multicenter ED based prospective study to validate this tool and advocate its superior use over some of the other risk stratification tools that currently exist.
Clinical Question:
- Is the CSRS a valid clinical tool in predicting 30-day serious outcomes not evident during the index ED evaluation of syncope patients?
What They Did:
- Prospective cohort validation study at 9 large Canadian EDs from March 2014 to April 2018
- Screened all consecutive ED patients for enrollment in the study both before and after the publication of the CSRS.
- After the publication of the CSRS, ED attendings and residents were trained on the study protocol with a 1-hour didactic session to enroll patients with true syncope and record the CSRS predictors
- Research assistants trained in the study protocol reviewed all ED visits during the study period to identify eligible patients who may have not been enrolled
- The following multi-step approach to ascertain 30-day outcomes was implemented:
- First a structured review of all available medical records related to the index and subsequent ED visits
- Second, a scripted telephone follow-up immediately after 30 days
- Third, they reviewed administrative health records for return visits, outpatient investigations, or hospitalizations at all local adult hospitals across four provinces
- Finally, patients without 30-day follow-up information were searched in provincial coroner’s database for matching records
- Two blinded emergency physicians adjudicated each serious outcome including time and when in the care the outcome occurred. A third physician resolved any disagreements between the two.
Inclusion Criteria:
- Emergency department patients ≥16 years of age
- Presented to the ED within 24 hours of their syncopal episode regardless of whether they were discharged or hospitalized
Exclusion Criteria:
- Prolonged LOC (> 5 minutes)
- Obvious witnessed seizure
- Mental status changes from baseline
- Head trauma causing LOC
- Major trauma
- Unable to obtain history (i.e. language barrier, alcohol or drug intoxication)
- Serious underlying condition identified during the index ED evaluation
Outcomes:
Primary:
- 30-day serious outcomes which was classified into two sub-groups:
- Arrhythmic Serious Conditions:
- Any serious arrhythmias
- Intervention to treat arrhythmias such as pacemaker/defibrillator insertion, or cardioversion
- Any death due to an unknown cause.
- Non-arrhythmic Serious Conditions:
- Myocardial infarction
- Serious structural heart disease
- Aortic Dissection
- Pulmonary Embolism
- Severe pulmonary hypertension
- Subarachnoid hemorrhage
- Any serious condition causing syncope
Results:
- 4131 patients with syncope were enrolled. After 160 (3.9%) with serious conditions were excluded and 152 (3.7%) were lost to follow-up, a total of 3819 patients were included in the final analysis
- 139 patients (3.6%) experienced serious 30-day outcomes
- 107 (2.8%) experienced arrhythmic outcomes, including 9 who died due to an unknown cause
- 32 (0.3%) experienced non-arrhythmic outcomes
- A total of 13 (0.3%) patients died within 30 days and the following causes of death were identified for the following four patients:
- Cardiogenic shock: 1 patient
- Septic shock: 1 patient
- Ventricular arrhythmia: 2 patients
- Of the 4030 patients:
- 114 (3.0%) were missing ECGs
- 1566 (41.0%) did not have troponin measured
Critical Results:
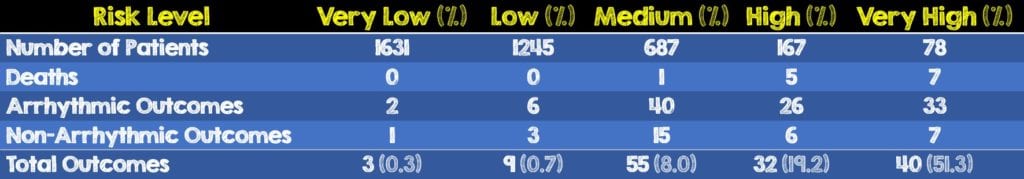
- In this validation study, 3 (0.3%) out of 1631 patients at very low risk and 9 (0.7%) at low risk experienced serious 30-day outcomes
- Approximately 20% and 50% of high risk and very-high risk patients experienced serious 30-day outcomes, respectively
- Of the 99 patients in the medium, high and very-high risk groups who experienced arrhythmic serious outcomes, 89 (89.9%) of them were identified within 15 days of the index ED visit
- The 13 patients with ventricular arrhythmia had them identified within 9 days of the index ED visit
- None of the 12 patients in the very low and low risk groups died
- At a threshold score of -1, including the 2145 of 3819 patients, the CSRS performed with a sensitivity of 97.8% (95% CI, 93.8 – 99.6%) and a specificity of 44.3% (95% CI, 42.7 – 45.9%).
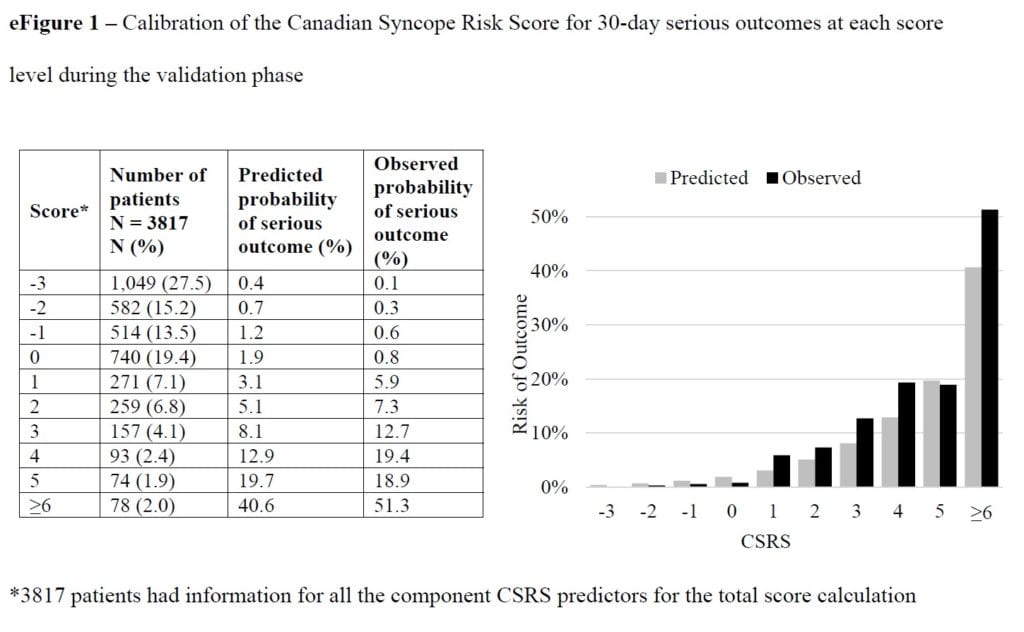
Table and Graph from [1]
Strengths:
- Large number of study patients involving multiple sites across several different provinces
- Consecutive sampling analyzing all visits from the entire ED population to prevent patient selection bias
- Had a third physician to resolve disagreements between the two blinded emergency physicians designated to adjudicate each serious outcome
- Utilized a well thought out multi-step approach to ascertain 30-day outcomes
- Only 152 (3.7%) of 4131 patients were lost to follow-up. This small amount was likely due to their thorough approach to follow-up as described above.
- The authors assumed that deaths from an unknown cause were due to arrhythmia which most likely overestimates the risk of the CSRS
- Attempted to reduce bias and prevent physicians from making disposition decisions based on the risk score by not including the estimated risk of serious outcomes associated with each score level from the derivation study on the data collection form
- Conducted sensitivity analysis for missing troponin values given large number
- The sample size of the study met the recommendations for validation studies of prediction tools (ie. Minimum of 100 events and a minimum of 100 non-events)
- Lastly, this validation study adhered to reporting requirements of several organizations and the CSRS’s ability to risk stratify patients follows the recommendations of several national professional medical societies.
Limitations:
- 20% of potentially eligible patients were not enrolled. The authors speculate it is because they were very low risk and discharged quickly before screening or the ED physician was too busy to complete the data collection form.
- The number of patients in the higher scores were smaller making CSRS results less reliable in these score ranges
- Although not on the data collection form, the CSRS score led to increased hospitalizations and patients getting loop monitoring. The authors did not find similar increases in the outpatient workup of these patients.
- The authors speculate that the large number of patients missing ECGs and the more than 50% of patients who never had troponins ordered were lower risk and unlikely to have influenced the study’s results by underestimating the actual short-term risk. Without the data, there’s no way to know for sure.
- All the centers in this study were academic EDs, therefore the accuracy of the CSRS in non-academic settings is unknown.
- Of the 5133 potentially eligible patients with syncope, 1002 were excluded because they were missed
- This external validity and generalizability may be limited as this validation study was limited to Canadian sites with a universal health care system that reliably captures all hospital-based healthcare facilities. Furthermore, some of these sites were also part of the derivation phase.
Discussion:
- In this prospective multicenter study, the short-term serious mortality for ED syncope was very low and similar to previously reported findings.3,4
- The authors recognize that three-quarters of the patients in this validation study were designated as being very low or low risk, again with less than 1% experiencing a serious outcome. Therefore, assuming these patients are given very clear instructions on specific symptoms and return precautions, discharge with outpatient follow-up to their primary care physician may be a reasonable treatment plan.
- Unlike other syncope risk stratification scores such as the San Francisco Syncope Rule (SFSR) and the Risk Stratification of Syncope in the ED (ROSE), the CSRS did not include patients with serious outcomes clear on ED presentation. The authors rightfully acknowledge its use may be more applicable to the lower risk patients who may be safe for discharge.
- The medicolegal considerations may be downplayed by the authors and a significant source of bias. Canadian physicians are sued significantly less than American physicians. With a more robust and established outpatient system they may be more likely to discharge patients compared to their American counterparts who are practicing more defensive medicine.5,6
- As an important reminder when using any kind of risk score, the management and disposition of each patient should be tailored to their individual clinical picture. Clinical decision tools should not supersede one’s physical exam skills and clinical gestalt.
Author’s Conclusions:
- The CSRS was successfully validated and its use is recommended to guide ED management of patients when serious causes are not identified during index ED evaluation. Very-low-risk and low-risk patients can generally be discharged, while brief hospitalization can be considered for high-risk patients. We believe CSRS implementation has the potential to improve patient safety and health care efficiency.
Our Conclusion:
- In patient’s presenting to the ED with syncope, the CSRS appears to be a validated and reliable tool in determining the risk of serious outcomes in lower risk patients. Patients who are very low and low risk should still have close outpatient follow-up and given strict return precautions. A lower threshold for admission is warranted when determining the need for hospitalization of high and very high-risk patients. As well any other risk stratification score or clinical decision tool, clinical judgement, patient presentation and shared decision making should be incorporated prior to determining dispositions
Clinical Bottom Line:
- Risk stratifying syncope patients remains a difficult diagnostic dilemma in the ED. The CSRS is a validated and reliable tool in helping to determine very low and low risk patients’ risk of serious outcomes who present to the ED with syncope. These patients can safely be discharged home with close outpatient follow up. Patients in the middle risk group will require physician judgment and shared decision making, while the high risk and very high risk patients will most likely require further investigation for cardiac etiologies and maybe hospital admission.
References:
- Thiruganasambandamoorthy V, et al. Multicenter Emergency Department Validation of the Canadian Syncope Risk Score. JAMA Intern Med. March 2020. PMID: 32202605
- Savani GT et al. Mortality Rates and Cost of Hospital Admissions for Syncope in the United States. J Am Coll Cardiol. 2017. Link Here
- Brignole M, et al. 2018 ESC Guidelines for the diagnosis and management of syncope. Eur Heart J. 2018; PMID: 29562304
- Sun BC, et al. Consortium to Standardize ED Syncope Risk Stratification Reporting. Standardized reporting guidelines for emergency department syncope risk-stratification research. Acad Emerg Med. 2012; PMID: 22687184
- Coyte PC, et al. Medical Malpractice — The Canadian Experience. N Engl J Med. 1991; PMID: 1984189
- Anderson GF, et al. Health Spending In The United States And The Rest Of The Industrialized World. Health Aff (Millwood). 2005; PMID: 16136632
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post Validation of the Canadian Syncope Risk Score appeared first on REBEL EM - Emergency Medicine Blog.
