
 Background: Currently the Advanced Trauma Life Support (ATLS) guidelines recommend initial treatment of decompression of a tension pneumothorax, as needle thoracostomy (NT) using a 5cm angiocatheter at the 2nd intercostal space (ICS2) in the mid clavicular line (MCL). With the growth of size in our population worldwide, there has been increasing evidence about two things:
Background: Currently the Advanced Trauma Life Support (ATLS) guidelines recommend initial treatment of decompression of a tension pneumothorax, as needle thoracostomy (NT) using a 5cm angiocatheter at the 2nd intercostal space (ICS2) in the mid clavicular line (MCL). With the growth of size in our population worldwide, there has been increasing evidence about two things:
- A 5cm angiocatheter may not be long enough to reach the pleural space
- The 2nd intercostal space at the mid clavicular line (ICS2-MCL) may not be the ideal location for needle decompression
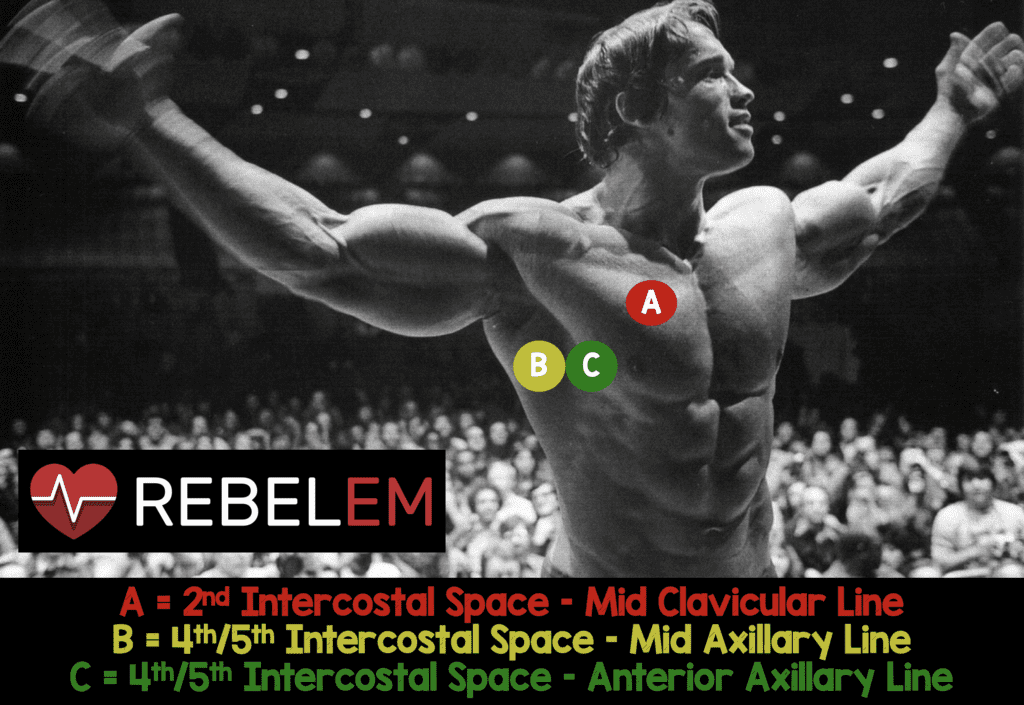
What other Alternative Locations are Possible for Needle Decompression:
- 4th/5th Intercostal Space at the Mid Axillary Line (4th/5th ICS-MAL)
- 4th/5th Intercostal Space at the Anterior Axillary Line (4th/5th ICS-AAL)
What Article are we Reviewing Today?
Laan DV et al. Chest Wall Thickness and Decompression Failure: A systematic Review and Meta-Analysis Coparing Anatomic Locations in Needle Thoracostomy. Injury 2015 [Epub Ahead of Print]. PMID: 26724173
What They Did:
- Systematic review and meta-analysis of trials assessing chest wall thickness and needle thoracostomy effectiveness
Outcomes:
- Chest Wall Thickness
- Effectiveness of Needle Thoracostomy with 5cm needle
Results:
-
34,652 studies evaluated
- 15 studies included for chest wall thickness
- 13 studies included for effectiveness of needle thoracostomy with 5cm needle
-
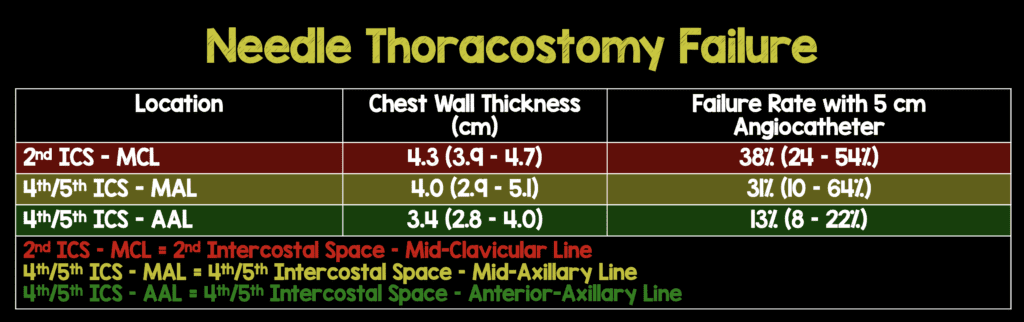
Chest Wall Thickness (Overall)
- ICS2-MCL: 4.3cm (95% CI 3.9 – 4.7cm)
- ICS4/5-MAL: 4.0cm (95% CI 2.9 – 5.1cm)
- ICS4/5-AAL: 3.4cm (95% CI 2.8 – 4.0cm)
-
Chest Wall Thickness (Men vs Women)
- ICS2-MCL: 3.6 vs 4.3cm
- ICS4/5-MAL: 3.3 vs 3.8cm
- ICS4/5-AAL: No studies reported
-
Needle Thoracostomy Failure Rate with 5cm Angiocatheter
- ICS2-MCL: 38% (95% CI 24 – 54%)
- ICS4/5-MAL: 31% (95% CI 10 – 64%)
- ICS4/5-AAL: 13% (95% CI 8 – 22%)
Strengths:
- Adhered to the Preferred Reporting Items for Systematic Reviews and meta-analyses (PRISMA)
- Adhered to the Meta-Analysis of Observational Studies in Epidemiology (MOOSE)
Limitations:
- Excluded ultrasound studies due to variable compression
- Most studies used were studies that used computed tomographic imaging, but this methodology cannot account for the degree of chest wall compression that providers may generate to access the pleural space. This may underestimate decompression rates with the use of a 5cm catheter
- Only evaluated 5cm angiocatheter and excluded other lengths
- Various study populations and methodologic factors caused a high level of heterogeneity between studies
- Due to the paucity of studies without significant results, this study was unable to conclude statistically significant differences in chest wall thickness
- Independent measurements of studies could not be verified and have to be taken at face value
Discussion:
- Regional variability in chest wall thickness may be partially explained by differences in BMI, thus in the USA and other western countries where BMI is higher, a change may be necessary in needle thoracostomy location or catheter length, but in other parts of the world, ICS2-MCL decompression may still be appropriate
- In austere environments equipment is limited and it may be difficult to find needles longer than 5cm and finding the anatomic site with the shortest distance to access the pleural space
- Clemency et al [4] found that a 5cm needle is not sufficient at ICS2-MCL and to achieve a 95% decompression rate you would need a 6.4cm catheter, but did not assess alternative anatomic sites
- Chang et al [5] did an observational, retrospective radiographic analysis of 100 consecutive adult trauma patients
- Using a 5cm needle at ICS2-MCL caused 0 injuries to underlying structures
- Using a 5cm needle at ICS4-AAL aimed perpendicular to chest wall caused 0 injuries to underlying structures
- Using a 5cm needle at ICS4-AAL at a shallow angle of entry caused a 1% rate of injury
- Using a 8cm needle at both ICS2-MCL and ICS4-AAL aimed perpendicularly to the chest wall, an injury rate as high as 9% was seen
- Using a 8cm needle at ICS4-AAL aimed at a shallow angle of entry caused an injury rate of 32%
Author Conclusion: “Evidence from observational studies suggests that the 4th/5th ICS-AAL has the lowest predicted failure rate of needle decompression in multiple populations.”
Clinical Take Home Points:
- Best evidence suggests that the 4th/5th ICS-AAL has the lowest predicted failure rate of needle decompression with a 5cm angiocatheter
- Given the increasing BMI of the population, a 5cm angiocatheter may not be long enough to reach the pleural space, but must be balanced with a risk of causing injury to vital structures with longer needles
References:
- Laan DV et al. Chest Wall Thickness and Decompression Failure: A systematic Review and Meta-Analysis Coparing Anatomic Locations in Needle Thoracostomy. Injury 2015 [Epub Ahead of Print]. PMID: 26724173
- Wax DB. Radiologic Assessment of Potential Sites of Needle Decompression of a Tension Pneumothorax at the Front? Mil Med 2014; 179: 783 – 6. PMID: 17959970
- Schroeder E et al. Average Chest Wall Thickness at Two Anatomic Locations in Trauma Patients. Injury 2013; 44: 1183 – 5. PMID: 23618786
- Clemency BM et al. Sufficient Catheter Length for Pneumothorax Needle Decompression: A Meta-Analysis. Prehosp Disaster Med 2015; 30: 249 – 53. PMID: 25857267
- Chang SJ et al. Evaluation of 8.0-cm Needle at the Fourth Anterior Axillary Line for Needle Chest Decompression of Tension Pneumothorax. J Trauma Acute Care Surg 2014; 76: 1029 – 34. PMID: 24662868
For More Thoughts on This Topic Checkout:
- Simon Laing & Zaf Qasim at HEFTEMCast: Needle Thoracostomy
- Lauren Westafer & Jeremy Faust on FOAMCast: Episode 36 – Pneumothorax
Post Peer Reviewed By: Anand Swaminathan (Twitter: @EMSwami)
The post What is the Best Anatomic Location for Needle Thoracostomy? appeared first on REBEL EM - Emergency Medicine Blog.
