
 This blog post is the third part of a series of 3, on a recent lecture I was asked to give on Critical Care Updates: Resuscitation Sequence Intubation. This talk was mostly derived from a podcast by Scott Weingart (Twitter: @EMCrit) where he talked about the physiologic killers during preintubation and perintubation. In this podcast, Scott mentions the HOp killers: Hypotension, Hypoxemia, and Metabolic Acidosis (pH) as the physiologic causes of pre-intubation/peri-intubation morbidity and mortality. Taking care of these critically ill patients that require intubation can be a high stress situation, with little room for error. In part three of this series we will discuss some useful strategies at the bedside to help us not worsen pre-intubation/peri-intubation metabolic acidosis.
This blog post is the third part of a series of 3, on a recent lecture I was asked to give on Critical Care Updates: Resuscitation Sequence Intubation. This talk was mostly derived from a podcast by Scott Weingart (Twitter: @EMCrit) where he talked about the physiologic killers during preintubation and perintubation. In this podcast, Scott mentions the HOp killers: Hypotension, Hypoxemia, and Metabolic Acidosis (pH) as the physiologic causes of pre-intubation/peri-intubation morbidity and mortality. Taking care of these critically ill patients that require intubation can be a high stress situation, with little room for error. In part three of this series we will discuss some useful strategies at the bedside to help us not worsen pre-intubation/peri-intubation metabolic acidosis.
What was the Premise of this Talk?
- Resuscitate Before You Intubate (i.e. Resuscitation Sequence Intubation)
- Hefner AC et al [1] and Kim WY et al [2] evaluated over 2800 patients requiring emergency intubation. In both trials the rate of cardiac arrest (CA) within 10 minutes of intubation ranged from 1.7% – 2.4%. Both trials listed pre-intubation hypotension (SBP ≤90mmHg) as a risk factor for cardiac arrest. Hefner AC et al also mentioned hypoxemia as a risk factor as well.
What are the Physiologic Killers Pre-intubation/Peri-intubation?
-
HOp Killers (Credit to Scott Weingart at emcrit.org)
- Hypotension (Hypotension Kills – Part 1 of 3)
- Hypoxemia (Hypoxemia Kills – Part 2 of 3)
- Metabolic Acidosis (pH)
pH Kills
- Try and avoid intubation in these patients if at all possible. Even consider a short trial of NIPPV while you try and correct the cause of metabolic acidosis.
-
Intervention 1: Bicarbonate Therapy
- Forsythe et al wrote a review article on Bicarbonate Therapy in Lactic Acidosis [1]. In this review article he argues against the use of bicarbonate due to the fact that when giving bicarbonate it eventually gets turned into CO2. Patients in severe metabolic acidosis are already tachypneic in an effort to blow off CO2, so any further CO2 could make them more acidotic and lead to cardiac dysrhythmias. He lists a slew of studies to support this contention:
- 18 Animal Studies: Increase serum pH, but Decrease Intracellular pH
- 2 Human Studies: Increase serum pH, but no improvement in hemodynamics or catecholamine responsiveness
- Bottom Line: No controlled studies have shown improved hemodynamics or catecholamine responsiveness due to sodium bicarbonate infusion
- Forsythe et al wrote a review article on Bicarbonate Therapy in Lactic Acidosis [1]. In this review article he argues against the use of bicarbonate due to the fact that when giving bicarbonate it eventually gets turned into CO2. Patients in severe metabolic acidosis are already tachypneic in an effort to blow off CO2, so any further CO2 could make them more acidotic and lead to cardiac dysrhythmias. He lists a slew of studies to support this contention:
-
Intervention 2: Ventilator-Assisted Pre-OXygenation (VAPOX)
- If intubation does become necessary maintaining spontaneous respirations is a critical action because maintenance of acid-base homeostasis is dependent on a respiratory alkalosis (i.e. hyperventilation). Even a brief apneic period can lead to worsening metabolic acidosis leading to cardiac dysrhythmias.
- Although VAPOX is primarily used for pre-oxygenation, in this scenario, we are using the ventilator to assist with ventilation to help assist spontaneous respirations to help avoid increased CO2 and worsening metabolic acidosis.
- There is a paper by Grant S et al, which is a case series discussing use of VAPOX in 8 patients requiring intubation [2], but the best protocol I have seen is done by Scott Weingart on EMCrit. The podcast can be found HERE and will be described below:
- Make sure there is someone who can use a ventilator and adjust settings before attempting this
- 1st place the patient on NC 15LPM of O2
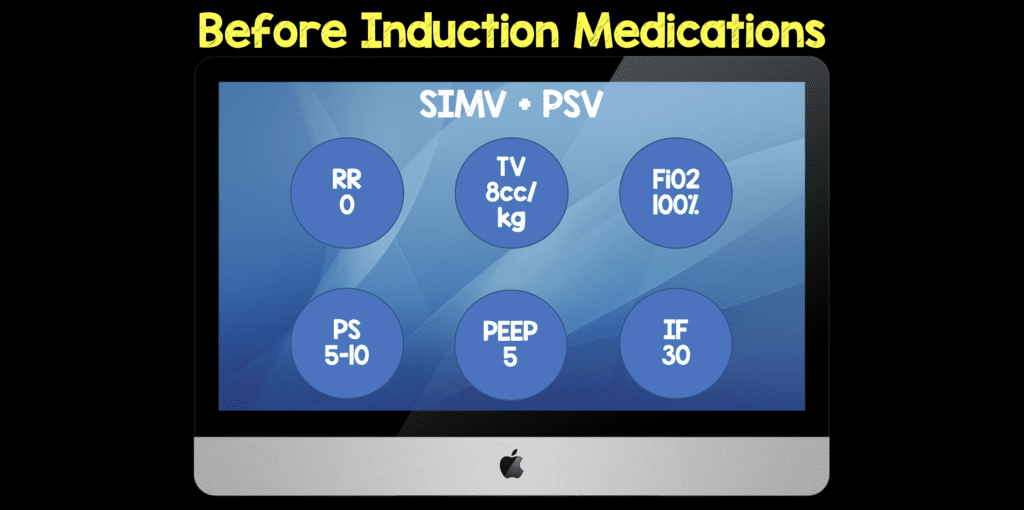
- Setup a Ventilator to Synchronized Intermittent Mandatory Ventilation (SIMV) + Pressure Support Ventilation (PSV)
- The reason this mode is used instead of Assist Control (AC) – Continuous Mandatory Ventilation (CMV) is that in this mode all breaths whether they are patient initiated or are ventilator initiated the patient will get full tidal volumes for every breath which can lead to barotrauma in a patient who is tachypneic.
- SIMV will give you three types of breaths:
1. Controlled: These breaths come at a set time. (i.e. If you set RR at 10 then every 6 seconds you get a breath. Controlled breaths will only be given if the patient is sedated/apneic/paralyzed or if you set RR higher than patients rate)2. Assisted Breaths: Triggered by the patient but only when the patient triggers or initiates the breath they will get full tidal volume set by the doc or therapist (i.e. VC SIMV + PS). If the rate is set at 10 then patient will get a breath every 6 seconds. If they trigger a breath at second 6 the breath given will be an assisted breath. If they fail to trigger or initiate a breath then the breath is a controlled breath.3. Spontaneous Breaths: SIMV mode allows you to take spontaneous breaths and you can add PS to these breaths. Again if rate set to 10 then every 6 sec the patient can take an assisted breath (if patient initiated) or controlled (time dependent if patient not breathing). So in between breaths the patient can take spontaneous breaths that will be pressure supported.
-
If you put a patient in VC SIMV mode w/ PS and set RR=O then they are essentially on PS only. No assisted breaths or controlled breaths will be delivered. Only PS. The RR set is the number of controlled or assisted breaths (if patient triggered).
-
- There are 6 settings that you need to setup (Before Induction Medications):
- Respiratory Rate = 0 (This lets the patient breath at their own rate)
- Tidal Volume = 550mL (8cc/kg of Ideal Body Weight)
- Fraction of Inspired O2 = 100%
- Pressure Support = 5 – 10cmH20 (Its hard to breath through a straw)
- PEEP = 5cmH20 (This can be titrated up to 15cmH20 if O2 sats ≥95%)
- Inspiratory Flow Rate = 30LPM (Normal ventilator set at 60LPM; We want a slow breath so we don’t insufflate the stomach)
- Place a BiPAP mask on your patient, connected to the ventilator
- Use End-Tidal Capnography to see what CO2 your patient is at (You want to shoot for this number or lower to ensure your patient is still blowing off CO2)
-
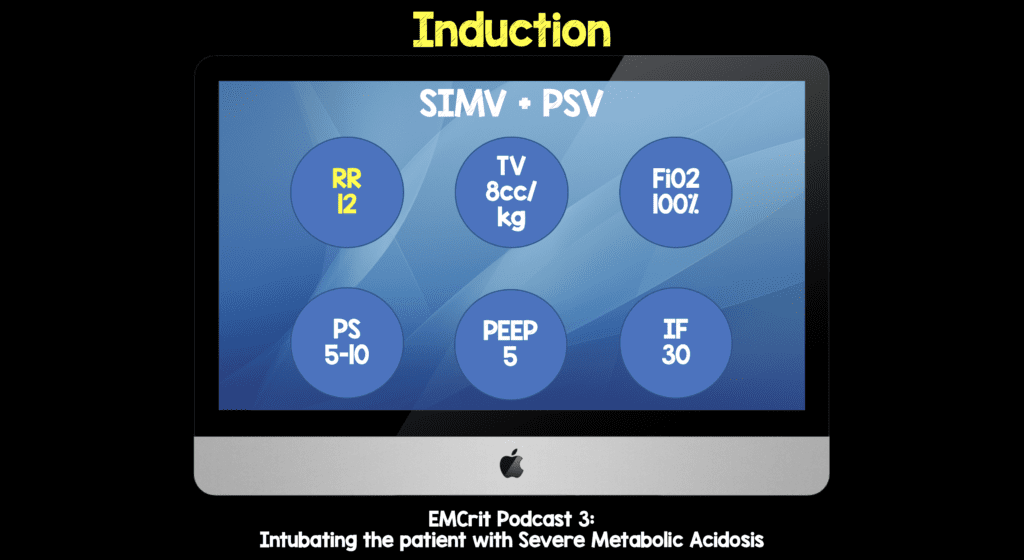
Induction of Patient with RSI Meds
- Give a good jaw thrust to ensure the airway is open
- Turn the respiratory rate up to 12 BPM (This ensures the patient is still blowing off CO2)
-
Intubation of Patient
- The most experienced person in the room should do the intubation (We want to ensure our best chance at 1st pass intubation)
- Attach the ventilator
- Turn the respiratory rate up to 30 (If you want to know why, listen to Scott Weingart’s podcast on this HERE)
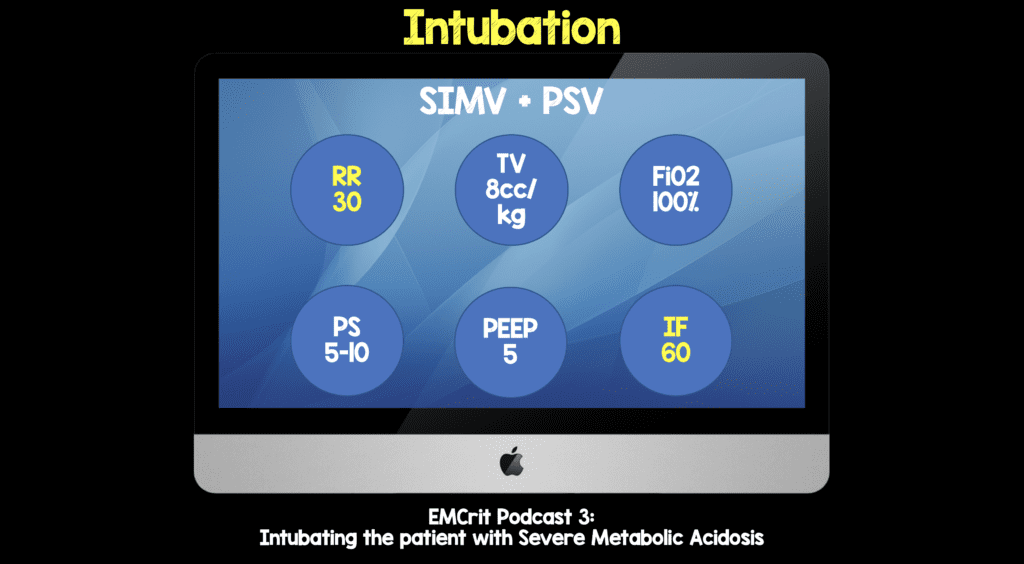
- Bottom Line: In a severely acidotic patient who needs to be intubated, VAPOX may be a nice way to ensure CO2 is being blown off to prevent further metabolic acidosis and cardiac dysrhythmias
Clinical Bottom Line:
- Severe Metabolic Acidosis in patients requiring intubation, if done incorrectly can lead to severe cardiac dysrhythmias
- The possibilities to ensure this doesn’t happen include:
- Intervention 1: Bicarbonate Therapy – This is a very controversial topic, but no controlled studies to date have shown hemodynamic improvements or improved catecholamine responsiveness
- Intervention 2: Ventilator-Assisted Pre-OXygenation (VAPOX) – This should only be performed if there is someone who can use a ventilator and change settings
Credit to Scott Weingart (Twitter: @EMCrit) for creating the HOp Killers mnemonic.
For More On This Topic Checkout:
- Scott Weingart at EMCrit: Podcast 3 – Laryngoscope as a Murder Weapon (LAMW) Series – Ventilatory Kills – Intubating the Patient with Severe Metabolic Acidosis
- Scott Weingart at EMCrit: Podcast 172c – Vent as a Bag & VAPOX
References:
- Forsythe SM et al. Sodium Bicarbonate for the Treatment of Lactic Acidosis. Chest 2000; 117(1): 260 – 7. PMID: 10631227
- Grant S et al. Ventilator-Assisted Preoxygenation: Protocol for Combining Non-Invasive Ventilation and Apnoeic Oxygenation Using a Portable Ventilator. EMA 2016; 28: 67 – 72. PMID: 26764895
- Mosier JM et al. The Physiologically Difficult Airway. WJEM 2015; 16(7): 1109 – 17. PMID: 26759664
Post Peer Reviewed By: Anand Swaminathan (Twitter: @EMSwami)
The post Critical Care Updates: Resuscitation Sequence Intubation – pH Kills (Part 3 of 3) appeared first on REBEL EM - Emergency Medicine Blog.
