
 Rocky Mountain Spotted Fever (RMSF)
Rocky Mountain Spotted Fever (RMSF)
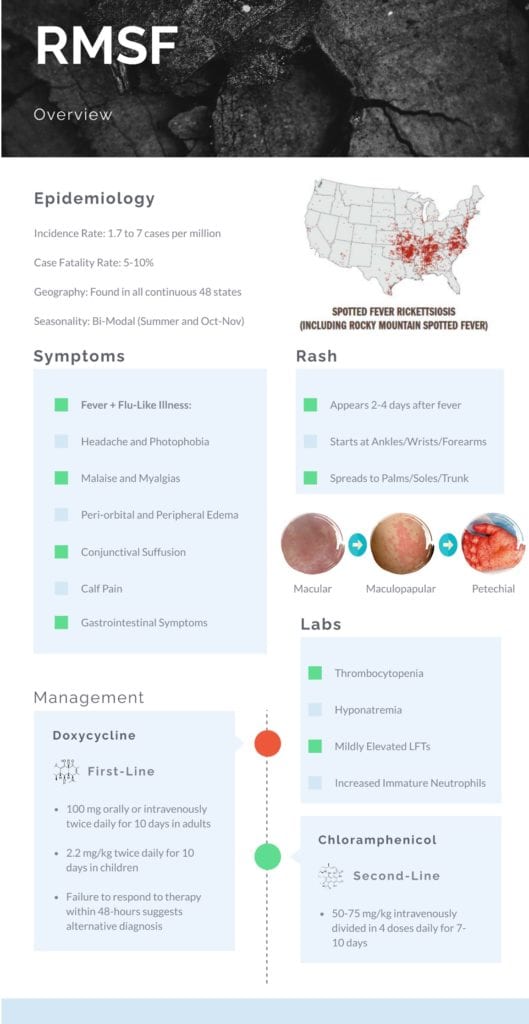
Epidemiology
Incidence:
- Overall annual incidence rose from 1.7 to 7 cases per million in the United States between 2000 and 2007 (Openshaw 2010)
- Annual incidence is highest in children aged 5-9 years of age (Amsden 2005)
Age:
- Median age is 42 years of age with greater than 87% of cases reported in Caucasian patients (Openshaw 2010)
Gender:
- Slight male to female predominance (Openshaw 2010)
Morbidity/Mortality: RMSF is the most common fatal rickettsial illness in the United States
- Overall hospitalization rates are noted be at 23.4% based on aggregated reviews of case reports (Openshaw 2010)
- Case fatality rate is estimated to be 5-10% overall (Biggs 2016)
- If treatment is delayed, case-fatality rates of 40-50% have been described for patients treated on day 8 or 9 of their illness
- Case fatality rate is highest in those over the age of 70 (Amsden 2005)
- Without treatment, the case fatality rate is over 25% (Lacz 2006)
Geography and Seasonality (Openshaw 2010): Cases have been found in all continuous 48 states
- Five States account for over 64% of all reported cases:
- North Carolina
- Oklahoma
- Arkansas
- Tennessee
- Missouri
- Seasonal distribution is concentrated in June (38 %) and July (38%).
- Second smaller peak is noted in October and November when adult ticks are active
Poor Prognostic Factors (Biggs 2016):
- Age < 10 or > 40 years of age
- Alcohol abuse
- Glucose-6-phosphate dehydrogenase deficiency
- Delays in diagnosis and treatment
- Immunocompromised states
- Use of sulfonamide antimicrobial
Pathogenesis (Lacz 2006):
- Rickettsia has tropism for endothelial cells and is able to spread centripetally via filopodia propulsion.
- Invasion of endothelial and smooth muscle cells of various organs leads to dysfunction of microcirculation, host immune response, vascular tone, angiogenesis, and normal hemostasis.
- Multiple organ systems are infected including the brain, liver, skin, lungs, kidneys, as well as the gastrointestinal system.
History and Physical:
Symptoms (Biggs 2016):
- Symptoms typically appear 3-12 days after bite of an infected tick
- Classic Triad: Tick Bite, Rash, Fever
- Present in only a minority of patients
- Rash: Absence of rash does not rule out this diagnosis
-
Timeline:
- Typically appears 2-4 days after fever onset
-
Distribution:
- Begin on the ankles, wrists, and forearms and subsequently spreads to the palms, soles, arms, legs, and trunk
- Typically spares the face
-
Morphology:
- Day 1: Initially seen as small, blanching macules
- Over next several days, the rash becomes maculopapular, sometimes exhibiting central petechiae
- Day 5 and 6: Rash becomes primarily petechial with involvement of the palms and soles
- Initial Symptoms (< 5 days):
- Fever
- Headache
- Chills
- Malaise
- Myalgia
- Photophobia
- Conjunctival Suffusion
- Periorbital and Peripheral Edema
- Calf Pain
- Acute Transient Hearting Loss
- Gastrointestinal Symptoms
- Severe Manifestations: Most cases are self-limiting, but RMSF has been associated with the following severe disease manifestations:
- Meningoencephalitis, Coma, Cerebral Edema
- Renal Failure
- ARDS
- Seizures
- Shock
- Cutaneous Necrosis and Gangrene
- Arrhythmias, Myocarditis
-
Timeline:
Diagnosis:
Labs: Characteristic laboratory findings are seen in RMSF along fever and non-specific flu-like illness:
- Thrombocytopenia
- Hyponatremia
- Mild Elevated Hepatic Transaminase
- Increased Number of Immature Neutrophils
Confirmatory Testing (Dantas-Torres 2007):
- Serological testing revealing four-fold change in IgG antibodies specific to R rickettsii using indirect immunofluorescence assay (IFA) in paired samples
- Antibodies are not detected until 7-10 days after disease onset
- RT-PCR assays are also available for diagnosis
- ELISA testing is also available for diagnosis
- Immunohistochemical staining from skin or tissue biopsies has also been used for diagnosis
Guest Post By:

Akash Ray, DO
PGY-2 Emergency Medicine Resident Inspira Medical Center
Vineland, NJ
Twitter: @_kashray
References:
- Biggs H et al. Diagnosis and Management of Tickborne Rickettsial Diseases: Rocky Mountain Spotted Fever and Other Spotted Fever Group Rickettsioses, Ehrlichioses, and Anaplasmosis – United States. MMWR Recomm Rep. 2016. PMID: 27172113
- Openshaw J et al. Rocky mountain spotted fever in the United States, 2000-2007: interpreting contemporary increases in incidence. Am J Trop Med Hyg. 2010. PMID: 20595498
- Amsden J et al. Tick-borne bacterial, rickettsial, spirochetal, and protozoal infectious diseases in the United States: a comprehensive review. Pharmacotherapy. 2005. PMID: 15767235
- Lacz N et al. Rocky Mountain spotted fever. J Eur Acad Dermatol Venereol. 2006. PMID: 16643138
- Dantas-Torres F. Rocky Mountain spotted fever. Lancet Infect Dis. 2007. PMID: 17961858
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post Emerging Tick-Borne Illnesses: Not Just Lyme Disease Part 4 RMSF appeared first on REBEL EM - Emergency Medicine Blog.
