
 The 2017 edition of the Social Media And Critical Care (SMACC) conference was held in Berlin, Germany this year (#dasSMACC). Over 2000 emergency physicians, intensivists, anesthetists, EMS providers, and nurses piled into the Tempodrom for three days of inspiring lectures and an all-around good time. This conference is truly a leader in innovation and continues to push the boundaries of medical education and entertainment. Here are some of the lessons learned and take home messages from the second day of the conference.
The 2017 edition of the Social Media And Critical Care (SMACC) conference was held in Berlin, Germany this year (#dasSMACC). Over 2000 emergency physicians, intensivists, anesthetists, EMS providers, and nurses piled into the Tempodrom for three days of inspiring lectures and an all-around good time. This conference is truly a leader in innovation and continues to push the boundaries of medical education and entertainment. Here are some of the lessons learned and take home messages from the second day of the conference.
dasSMACC – Day #2
A multi-disciplinary panel started the day discussing inter-professional issues in medicine (i.e. Tribes). The panel was lead by Walter Eppich and including Jesse Spurr, Liz Crowe, Carol Hodgson, Ashley Liebig, and Sandra Viggers
- There should be one tribe in medicine…the human tribe. The common mission in medicine should also be patient care which can help unite the tribes
- We all belong to multiple tribes with different sets of rules
- We generally judge others by their actions, and ourselves by our intentions, so be generous to others
- Leaders in medicine are often those that have been there the longest or those willing to raise their hands, not necessarily the most qualified. Leaders need leadership training
- You are an emotional contagion. Your attitude sets the stage for the daily culture
- Tribalism in medicine can cause worse care, due to narrow views, patients becoming body parts
- South Africa has a great intern system using wrist bands to indicate fatigue:
- Green Band = Working <24hrs
- Orange Band = Working 24 – 30hrs
- Red Band = Working >30hrs

- Culture is created by everyone. We all need to take responsibility for the culture at each of our own work places
- The good part of tribes is they help build cohesion and a team, but the bad part about tribes is it can create friction between tribes and gets in the way of patient care (Protective within teams, but destructive across specialties)
- In the real world we introduce ourselves by our names…why don’t we do this at the workplace
Chris Hicks gave a talk about making complex problems simple:
- Managing complexity is about limiting variables, reducing goals to habits, basic steps, process over outcome
- When things get complex, it is our ability to simplify that will see us through
- Simple can be harder than complex because you have to get your thing straight -Steve Jobs-
- Develop habits—habit breaks down the complex. It becomes harder not to execute, than to execute. Habit also allows you to identify outliers and variances
- Emergence—process of self-organizing in complex situation, bringing individual behavior into a group alignment; with good team setup and task allocation, team can solve much more complex tasks than any individual can
- Organize teams not by specialty but by a specific goal (i.e. chest tube team, airway team, pelvic binder team, etc…)
- Factor Down—breaking down the problem into manageable parts
- Limit Variables—you can’t constrain chaos, but you can allow only certain paths for it to take
- Take Home Points
- Lean on Habit
- Foster Emergence
- Factor Down
- Limit Variables
- Dream big but plan simple

Maaret Castren pondered the Future of Out of Hospital Cardiac Arrest. The chairwoman of the European Resuscitation Council and the International Liaison Committee on Resuscitation talked about where we are today and how to improve
- 50% of patients with sudden cardiac death had symptoms up to 4 weeks prior to their death
- No one in ventricular fibrillation should die. If they do, we need to look at what we did wrong. (For clarification, VF should not be the final rhythm at the time of death.)
- The best systems in the world only have about 20% survival for out of hospital cardiac arrest
- The European Resuscitation Academy has published an article on 10 steps to improve cardiac arrest survival
- Most medical treatments have been designed for the average patient. One size does not fit all in cardiac arrest
Nikki Stamp, cardiac surgeon, offered a guide to the resuscitation of the post cardiac surgery patient. This includes pacemakers/ICDs, valve replacements, and CABG:
- Causes of the need for resuscitation in these patients include ischemia, mechanical issues, arrhythmias, and unknown causes
- Loss of pacing capture can mean the heart is distending, which is a bad thing
- If this patient arrests, get on the rhythm early because they have a propensity for VT/VF. Deliver 3 sequential shocks (not part of ACLS) and pace early
- Manual CPR can be done on a patient with a left ventricular assist device, but not mechanical CPR
- Bottom Lines:
- Shock early, pace early
- Most should not die with a closed chest
- ECMO/CPB is there to be used
- LVAD = CPR and expert advice
- Manage the at risk patient as a team
Ashley Liebig was tasked to argue that doctors don’t rule the resus room. She relayed the story of how she challenged this. She also noted that doing something different opens the door to criticism. She offered 5 ways that doctors don’t rule the resus room.
- Ergonomics—it is not just for the carts and cabinets. Placing people in the optimum place makes things easier
- Nurse-led codes—Nurses do ACLS before the doctor arrives. Let them run the code. This provides a cognitive offload for the doctor to gather more history and determine the cause that can be treated.
- Assigned roles—Having a single role frees people up to perform that role to the best of their ability without having to worry about what else they need to do
- Communication—what more needs to be said. Free dialogue and closed loop communication insures completion of tasks
- Briefing—breaking down what went well and what can be improved following the resuscitation offers continual opportunities for improvement.
Two New York docs in the resus room pitted Reuben Strayer and Scott Weingart in a point/counter-point battle. Natalie May moderated this session while collecting money in a jar for charity for any curse words uttered. A decent amount of money was collected.
- Sympathetic Crashing Acute Pulmonary Edema (SCAPE) is the Nursemaid’s elbow of the resus room.
- Non-Invasive Ventilation (NIV) should be started on every patient in respiratory distress. This is an intubation-saving procedure
- SCAPE should be treated with a 1-2 mg bolus of IV Nitroglycerin (mg, not mcg) followed by a drip starting at 100-200 mcg/min. Alternatively; the drip can be started at 400-500 mcg/min
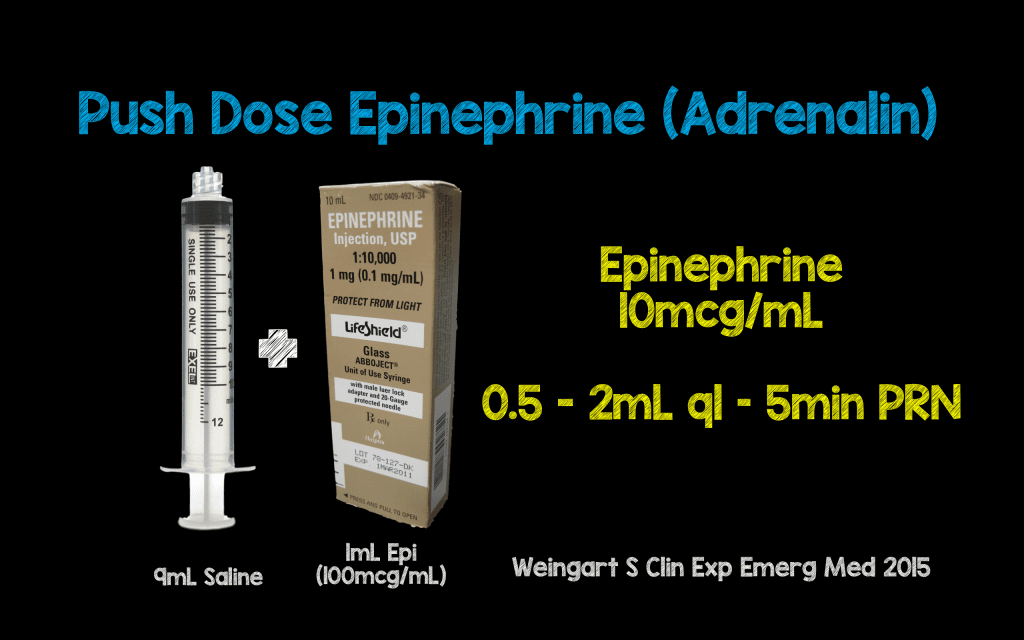
- Perintubation hypotension is associated with cardiac arrest. Strayer recommended the dirty epinephrine drip, while Weingart touted push dose epinephrine

Daniel Lichtenstein discussed whole body ultrasound centered on the lung. Lichtenstein is a giant in the world of point of care ultrasound, performing initial research in the late 1980s and early 1990s. He lamented on not coming up with a flashy acronym for his scan identifying abdominal blood in trauma patients (i.e. FAST).
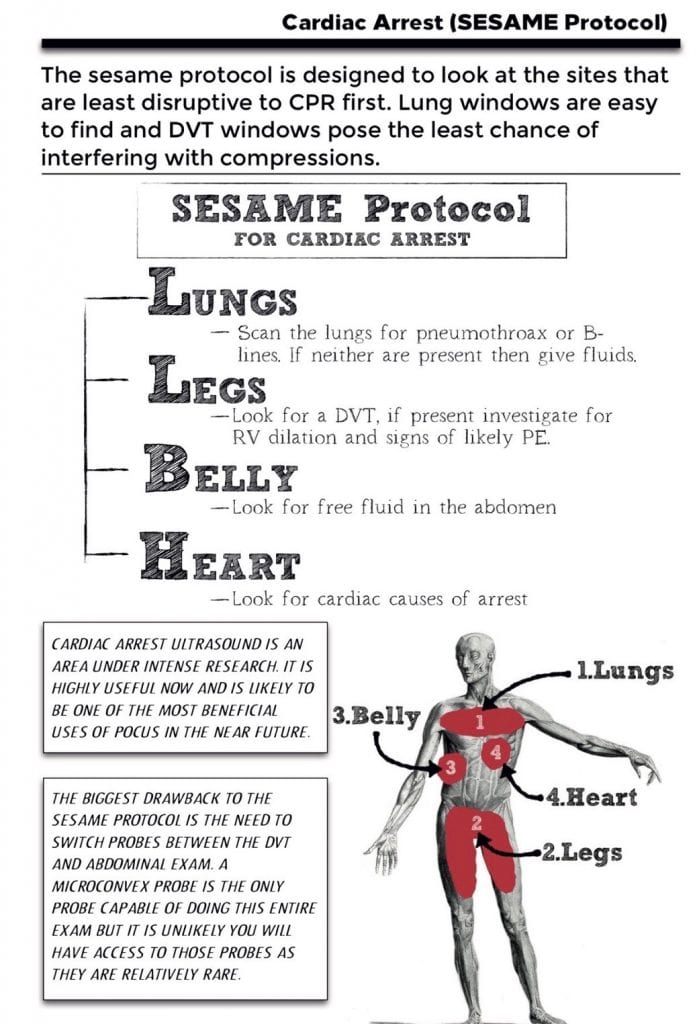
- For cardiac arrest, use the Sesame protocol. This is a fast process that can be done while compressions are being performed
- The Blue protocol is a step-by-step approach for lung ultrasound
Michele Domico dropped some pearls on pediatric cardiac disease
- If you don’t think about it, you will never see it
- A child with fatigue is not normal
- Don’t get locked into a single diagnosis. Anchoring on only one diagnosis can be disastrous.
- If you think something is abnormal, it probably is, regardless of what the parents say.
- Beware of “quiet tachypnea.” Increased respiratory rate without increased work of breathing can be a sign of decreased systemic perfusion.
- Beware of cognitive bias. You provide a new set of eyes when you see the patient. The previous diagnosis may be wrong
- If a patient has multiple visits to the doctor, but is not getting better, think cardiac causes
- BNP measures myocardial stress. Troponin measures myocardial death
MJ Slabbert offered some insights of decision-making:
- Decisions you make determine the actions you take
- “Without data you’re just another person with an opinion.” -W. Edwards Deming
- “Not everything that counts can be counted, and not everything that can be counted counts.”-Albert Einstein
- Protocols are the safety net for the novice, but can be shackles in difficult situations. Experience allows you to go outside the algorithm to direct care of the patient. This is a process call naturalistic decision-making.
- Medicine is a science of uncertainty and an art of probability – William Osler
Daniel Cabrera gave a nod to classic 16-bit video games (think original Nintendo) in his talk on anaphylaxis
- Only 50% of anaphylaxis patients receive epinephrine
- Only 40% of patients are discharged with an Epipen
- Only 20% of patients receive appropriate follow up
- They will survive your 1st misdiagnosis of their anaphylaxis, but they may not make it back to you the 2nd time
- Death in anaphylaxis comes from cardiovascular collapse, but also from lack of education and access
- Don’t wait for hypotension or respiratory failure to give epinephrine
- 50% of patients will require a 2nd dose of epinephrine. This dose should also be given IM
- Options for refractory anaphylaxis include: epinephrine drip, glucagon, norepinephrine, vasopressin, methylene blue, and ECMO
The final session of the day was a panel discussion entitled Resuscitation for the Resuscitationist. Scott Weingart was the chair for the panel, which included Steve Bernard, Jim Manning, Sara Gray, Maaret Castren, MJ Slabbert, and Lionel Lamhaut:
- Vasoplegia is defined as refractory low diastolic blood pressure. Treat the etiology. A new aortic catheter is being studied. There are also come case reports on using methylene blue
- When the protocol provides no solution, do what you can, whether there is evidence or not
- For refractory VF, consider dual sequential defibrillation. If you don’t have two machines and multiple shocks have not worked, consider moving the pads to a different location
- Patients in refractory VF can be taken to the cath lab with mechanical CPR in progress
- Cardiologists need to get over patients dying on the cath table. The panel felt this is an ethical question and concern over their mortality stats should not be the concern of the cardiologist
- Esmolol is another option for refractory VF
- ECMO in refractory VF is about preserving the brain
- If the cath lab won’t take the patient in refractory VF, the panel felt that thrombolysis was indicated
- Monitoring during cardiac arrest in the prehospital should include the basic monitoring as on all patients, plus end tidal CO2 monitoring if available. In the ED, EtCO2 and the placement of a femoral arterial line were recommended
- Personalized epinephrine doses were discussed. Some people need more than 1 mg, while others need less the 1 mg. To make this decision, an arterial line needs to be in place
- There is some evidence for the use of ketamine, and perhaps fentanyl, during CPR induced consciousness. At the very least, talk to the patient to let them know what is happening and you have a plan
- The use of mechanical CPR brings calm to the scene and allows cognitive off loading as well as an overall more controlled code
- It is extremely rare to survive out of hospital cardiac arrest after 40 minutes of high quality CPR. Use ultrasound to assist in making the decision to stop resuscitation
- The question of “Stay and Play” vs. “Load and Go” for EMS was addressed. The panel mostly agreed that “Stay and Play” is the way to go, unless there is a reason to move (i.e. cath lab)
- There is some preliminary data on the Heads Up Resuscitation. This is mechanical CPR being performed with the head of the bed elevated to 45 degrees. The optimal angle has yet to be defined
- The thought behind this method is that if provides increased venous drainage from the brain
- Most of the panel is still using 32-34°C for cooling post arrest. 1/3 of patients cooled to 36°C developed fever, which is the outcome to be avoided. There is also a lot of shivering at 36°C. These patients will require paralysis
- Should EMS bypass small hospitals to take arrest patients to cardiac arrest centers? ILCOR says yes, but the panel states that it depends on the location
For More on This Topic Checkout:
- Lauren Westafer & Jeremy Faust at FOAMCast: #dasSMACC – Pulmonary Embolism, Pulmonary Edema, TEE, & Pediatric Cardiology
- Simon Carley at St. Emlyn’s: #dasSMACC Day 2
Post Peer Reviewed By: Salim Rezaie (Twitter: @srrezaie)
The post Lessons Learned and Take Home Messages From dasSMACC – Day 2 appeared first on REBEL EM - Emergency Medicine Blog.
