
 Definition: A life-threatening adverse reaction resulting from local anesthetic reaching significant systemic circulating levels. Local Anesthetic Systemic Toxicity (LAST) is rare and almost always occurs within minutes of injection of the local anesthetic.
Definition: A life-threatening adverse reaction resulting from local anesthetic reaching significant systemic circulating levels. Local Anesthetic Systemic Toxicity (LAST) is rare and almost always occurs within minutes of injection of the local anesthetic.
Causes:
- Injection of local anesthetic into the systemic circulation (either errantly as part of a regional block i.e. Bier block)
- Rapid absorption of local anesthetic injected into a highly vascular area
- Use of local anesthetic doses in excess of the maximum dose (typically occurs with multiple subcutaneous injections)
- Common implicated procedures: bronchoscopy, circumcision, tumescent liposuction. Consider diagnosis in any patient coming from outpatient surgical center with cardiac arrest
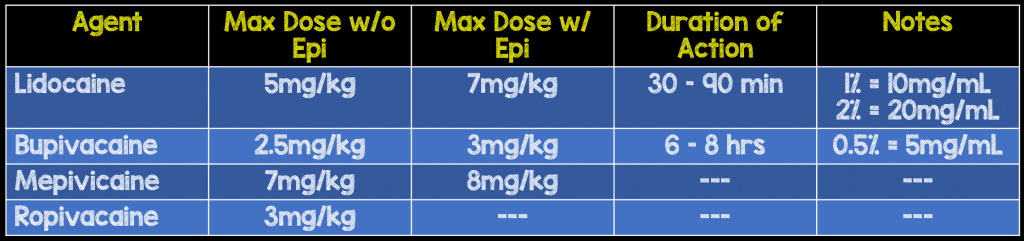
Commonly Used Local Anesthetics
Mechanism of Action
- All of the local anesthetic agents are sodium channel blockers
-
Lidocaine
- Class IB antidysrhythmic
- Gains rapid entry to the brain thus producing CNS symptoms early on
Signs + Symptoms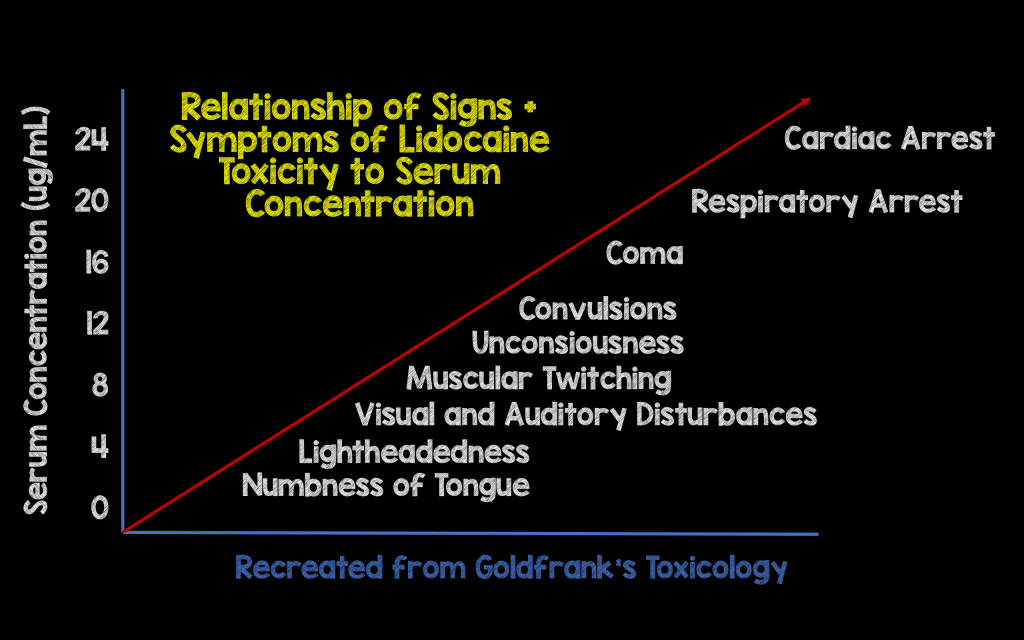
-
CNS Symptoms
-
Minor Signs/Symptoms
- Tongue and perioral numbness
- Parasthesias
- Restlessness
- Tinnitus
- Muscle fasciculations + tremors
-
Major Signs/Symptoms
- Tonic-clonic seizures
- Global CNS depression
- Decreased level of consciousness
- Apnea
- Neurologic symptoms typically precede cardiovascular symptoms in lidocaine toxicity
-
Minor Signs/Symptoms
-
Cardiovascular Symptoms
- Early Signs: Hypertension and tachycardia
-
Late Signs
- Peripheral vasodilation + profound hypotension
- Sinus bradycardia, AV blocs
- Conduction defects (Prolonged PR, Prolonged QRS)
- Ventricular dysrhythmias
- Cardiac arrest
- Cardiovascular symptoms typically present first in bupivacaine toxicity
Differential Diagnosis
- Anaphylaxis (rare with amide anesthetics)
- Effect of other sodium channel blockers (i.e. antihistamines, TCAs, cocaine, antimalarials)
- Anxiety
Management
-
Prevention of toxicity
- Know + calculate maximum doses of local anesthetic agent prior to use
- Always aspirate prior to injection to ensure drug is not delivered intra-arterial or intravenous
- Ask patient about symptoms after injection
- Consider serial repairs of large or multiple wounds to minimize chance for toxicity
-
Basic Management
- Institute basic management if ANY sign/symptom is present after local anesthetic use (i.e. new perioral numbness; don’t wait for CV findings!)
- Stop injection or infusion of agent
- Establish IV access if not already present
- Continuous cardiac monitor
-
Aggressive Supportive Care
-
Airway/Breathing
- Toxicity worsened by hypercapnea, hypoxia and acidosis
- Use 100% FiO2
- Hyperventilate
-
Cardiovascular Collapse
- Consider epinephrine to augment cardiac output and improve peripheral vascular tone
- Consider bicarbonate infusion for severe acidosis
- Initiate high-quality CPR in arrest
- Manage seizures with benzodiazepines over propofol as propofol is a cardiac depressant (Goldfrank’s 2015)
-
Airway/Breathing
-
Lipid Emulsion Therapy (20% Intralipid)
- Mechanism of action: unclear. May act as lipid sink, may facilitate redistribution of local anesthetic from target organs
-
Utility in lidocaine vs. bupivacaine
- Due to lidocaine short 1/2 life, may be unnecessary. CPR alone typically adequate
- Bupivacaine has longer 1/2 life making intralipid more useful in this form of LAST
-
Dosing (Neal 2012, Cao 2015)
-
Bolus: 1 – 1.5 ml/kg over 1 min
- Can repeat bolus every 3 minutes up to a total dose of 3 ml/kg
-
Infusion: 0.25 ml/kg/min
- Continue infusion until hemodynamically stable for at least 10 minutes
- Can increase infusion to 0.5 ml/kg/min if BP worsens
-
Bolus: 1 – 1.5 ml/kg over 1 min
- Continue CPR during infusion to circulate drug
Take Home Points
- The key in managing LAST is prevention. Know your dose, know your maximum dose, always aspirate prior to injection and ask patient about symptoms
- Lidocaine toxicity CV complications are typically preceded by neurological signs/symptoms. If these develop, stop administration, place patient on monitor and ready your antidote
- Bupivacaine toxicity can be sudden and catastrophic. If you are using the drug, undershoot your max dose and know where your antidote is
- Intralipid has been shown to be effective in LAST. Administer the drug anytime there are signs of hemodynamic compromise
For More on This Topic Checkout:
- LITFL: Local Anesthetic Toxicity
- Wiki EM: Local Anesthetic Systemic Toxicity
References:
- Schwartz DR, Kaufman B. Local Anesthetics. In: Hoffman RS, Howland M, Lewin NA, Nelson LS, Goldfrank LR. eds. Goldfrank’s Toxicologic Emergencies, 10e New York, NY: McGraw-Hill; 2015. Link
- Neal JM et al, American Society of Regional Anesthesia and Pain Medicine. American Society of Regional Anesthesia and Pain Medicine checklist for managing local anesthetic systemic toxicity: 2012 version. Reg Anesth Pain Med 2012;37:16–8. PMID: 22189574
- Cao D et al. Intravenous lipid emulsion in the emergency department: a systematic review. J Emerg Med 2015; 48(3): 387-97. PMID: 25534900
Post Peer Reviewed By: Salim Rezaie (Twitter: @srrezaie)
The post Local Anesthetic Systemic Toxicity (LAST) appeared first on REBEL EM - Emergency Medicine Blog.
