
 Background: There are several classes of medications available to treat pediatric migraines and because of this many providers have different combinations that they like to use. Typically, NSAIDs, anticholinergics, and dopamine antagonists are used with varying degrees of success. There is little evidence to guide providers if these agents fail in terms of which medications would be helpful for further abortive therapy. There have been several trials published in the adult population regarding the use of low dose propofol (LDP) for acute migraines. Propofol is great in the ED setting due to its short acting duration of action, as well as its anti-emetic properties. Many things done in pediatrics are extrapolated from adult literature, however the authors of this paper wanted to see if LDP was any better than standard therapy (ST) in the treatment of acute pediatric migraines.
Background: There are several classes of medications available to treat pediatric migraines and because of this many providers have different combinations that they like to use. Typically, NSAIDs, anticholinergics, and dopamine antagonists are used with varying degrees of success. There is little evidence to guide providers if these agents fail in terms of which medications would be helpful for further abortive therapy. There have been several trials published in the adult population regarding the use of low dose propofol (LDP) for acute migraines. Propofol is great in the ED setting due to its short acting duration of action, as well as its anti-emetic properties. Many things done in pediatrics are extrapolated from adult literature, however the authors of this paper wanted to see if LDP was any better than standard therapy (ST) in the treatment of acute pediatric migraines.
Protocol:
-
All patients received:
- 20mL/kg (max 1L) of NS over 30 min
-
ST:
- Ketorolac 0.5mg/kg (max 30mg IV)
- Diphenhydramine 1mg/kg (max 50mg IV)
- Metoclopramide 0.1 mg/kg (max 10mg IV) – 5 patients received prochlorperazine 0.1mg/kg instead (max 10mg IV)
-
LDP:
- Low-dose propofol 0.25 mg/kg (max 30mg IV) q5min until resolution of headache (i.e. VAS ≤4) with a maximum of 5 doses
What They Did:
- Multicenter, prospective, pragmatic randomized controlled clinical trial of pediatric migraine treatment
- Low-dose propofol (LDP) vs standard therapy (ST)
Outcomes:
- Primary: Percent pain reduction after initial treatment
-
Secondary:
- ED LOS
- Treatment LOS
- 24hr rebound headache
- Return visits to the ED
- Adverse reactions (i.e. extrapyramidal reactions, hypotension, hypoxia, or respiratory depression)
Inclusion:
- Age 7 – 19 years
- Had a diagnosis of migraine or diagnosed with migraine by ED physician
- Visual analog Scale (VAS) Score of 6 – 10
Exclusion:
- Known allergy to any study medications
- Signs of a secondary headache
- Acute head injury
- Major surgery within the last 7 days
- Intracranial shunt
- History of tumor or malignancy
- Chronic lung disease
- Congenital or acquired heart disease with poor cardiac function or single ventricle
- Known renal failure
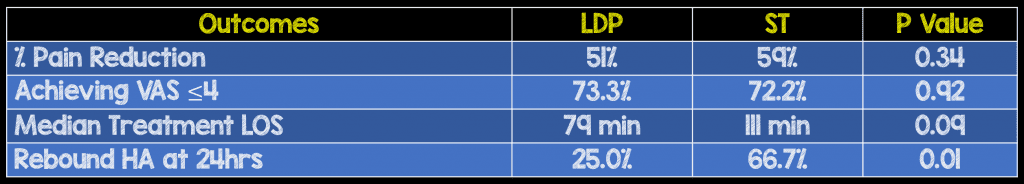
Results:
- 66 patients included in the analysis
-
Adverse Events:
- LDP: 1/30 patients (3.3%) had transient oxygen desat to 89% that self-resolved without further intervention
- ST: 3/36 patients (8.3%) had extrapyramidal symptoms
Strengths:
- Multicenter randomized clinical trial
- Analysis of rebound headache was limited to patients who had experienced successful treatment of their index headache to avoid confounding with rescue medications
- No baseline differences of patients in either arm of the trial with the exception of personal history of migraine and use of daily prophylaxis for migraine medication
Limitations:
- Due to the national shortage of prochlorperazine the study protocol did have to be modified during the middle of the study
- The authors chose an interesting primary endpoint in the fact that it was percent pain reduction (i.e. Is it the same to go from 10 to 8 as it is to go from 5 to 3?)
- Although given at a low dose, patients in the propofol arm still required continuous cardiorespiratory and pulse oximetery monitoring with BP checks q5min requiring a nurse to be continually at the bedside
- Patients failing the initial arm of therapy were given rescue therapy at the discretion of the treating physician and not crossed over to the other arm of the study
- Patients and providers were not blinded to study medication
- Unable to track screened patients at one of the EDs due to limited research infrastructure. It is possible that some eligible patients were missed at this facility
- Strict international headache criteria for the diagnosis of migraine was not used, which may have led to the inclusion of some non-migraine primary headaches, therefore underestimating the usefulness of LDP in migraines
- Pain scores were assessed at different frequencies of time, with LDP being assessed every 5 minutes and ST being assessed every 15min
- Study underpowered as it did not enroll the 74 patients required to reach statistical significance
Discussion:
- In this particular trial the mean number of propofol boluses was 3.3 and a median of 4
Author Conclusion: “LDP did not achieve better pain reduction than ST, however, LDP was associated with significantly fewer rebound headaches and a nonsignificant trend toward shorter median LOS from drug administration to disposition.”
Clinical Take Home Point: In this study LDP was not better than ST for pain reduction in pediatric migraine, but did result in fewer rebound headaches. This study will not change my practice of using ST first to help abort pediatric migraines, but for those patients that are refractory to primary treatment, LDP is a nice opioid-sparing option.
References:
- Sheridan DC et al. Low-Dose Propofol for Pediatric Migraine: A Prospective, Randomized Controlled Trial. JEM 2018. PMID: 29456086
For More Thoughts on This Topic Checkout:
- Rick Pescatore at REBEL EM: Alternative Headache Therapies
Post Peer Reviewed By: Anand Swaminathan (Twitter: @EMSwami)
The post Milk of Amnesia (Propofol) for Pediatric Migraines? appeared first on REBEL EM - Emergency Medicine Blog.
