Modified Physiological Triage Tool (MPTT)
TRIAJE
Es oficial, PHTLS y ATLS asumen este algoritmo de Triage Prehospitalario simplificado con solo dos colores, Amarillo (no grave) Rojo Grave, Negro (nada que hacer) Verde que se siente y tome agua en lo que trabajamos con los que nos necesitan... Traduccion Dr. Ramon Reyes, MD jijij TRAUMA SYSTEMS National Guidelines for the Field Triage of Injured Patients by American College of Surgeons ACS. 2021 ir al enlace para obtener el documento completo
¿Conoces el Sistema de Triaje de Trauma Estadounidense de solo dos colores?
Te damos la oportunidad de conocerlo en Español o Ingles en los Siguientes Enlaces by #DrRamonReyesMD
Español
Guía Nacional para el Triaje de Campo de Pacientes Lesionados 2021
English
TRAUMA SYSTEMS National Guidelines for the Field Triage of Injured Patients by American College of Surgeons ACS. 2021
https://emssolutionsint.blogspot.com/2022/10/trauma-systems-national-guidelines-for.html #PHTLS #ATLS #ITLS #Triage #Triaje #EMS #Trauma
leer https://emssolutionsint.blogspot.com/2022/10/trauma-systems-national-guidelines-for.html #DrRamonReyesMD
Ver video completo y compartir via Facebook https://www.facebook.com/DrRamonReyesMD/videos/226272200208371
http://eprints.whiterose.ac.uk/123313/5/Clean%20Revision_TARN%20Validation_EMJ_Submission%20.pdf
http://jramc.bmj.com/content/jramc/early/2017/10/21/jramc-2017-000819.full.pdf
https://www.semanticscholar.org/paper/A-concept-for-major-incident-triage%3A-full-scaled-Rehn-Andersen/822aceb07fe1ff7692c75d7d56b69bdf01889cf8
http://jramc.bmj.com/content/jramc/early/2017/10/21/jramc-2017-000819.full.pdf
https://www.semanticscholar.org/paper/A-concept-for-major-incident-triage%3A-full-scaled-Rehn-Andersen/822aceb07fe1ff7692c75d7d56b69bdf01889cf8
Read article
The work of a Royal Navy doctor is being implemented by the NHS and the Defence Medical Services for use in the aftermath of terrorist attacks and mass casualty incidents.
Advances in military medicine have often filtered into civilian care, such as blood transfusions in the First World War to the treatment used on casualties in Afghanistan.
Deciding the priority of treatment in mass casualty incidents is known as 'triage' and is vital not only in military situations but is also pivotal in the wake of terrorist attacks in the UK. Key to success in triage is identifying patients who need life-saving interventions.
For years medics have been using flow charts to conduct triage and to determine the priority of treatment for patients in mass casualty incidents.
But recent studies show that the existing method of UK triage (both military and civilian) has only between 28-43% chance of correctly prioritising patients in need of life-saving interventions.
The MPTT-24 is being introduced as the new method of triage within the Defence Medical Services.
Royal Navy Emergency Medicine Trainee, Surgeon Lieutenant Commander Jamie Vassallo, has been studying triage since 2010 and undertook a PhD to try and optimise the process.
His new model, the Modified Physiological Triage Tool-24 (MPTT-24) allows for a quicker assessment at the scene and in the military setting can correctly identify over 80% of patients in need of urgent intervention.
Surgeon Lieutenant Commander Vassallo said: "What we’re seeing from recent major incidents is that quite often the initial triage process is being conducted by non-medical personnel such as police firearms officers.
"What we need therefore is an effective triage process that can be utilised irrespective of the background of the provider.
"The benefit of the MPTT-24 is that it was designed in such a way that it can be reliably used by a variety of individuals, irrespective of their clinical experience.”
The MPTT-24 has been incorporated into the new 2018 NHS England Clinical Guidelines for Major Incidents and additionally is being introduced as the new method of triage within the Defence Medical Services where it has already demonstrated very good success rates on recent exercises.
He added: "It's been a number of years of hard work - which was the basis of doing the PhD in Major Incident triage.
"It's not often that you see outputs from PhDs being implemented into practice - certainly not as soon as this has been done, so it really is a proud moment of mine."
The nature of the MPTT-24 means that it is transferable to be able to be reliably used by first responders, firearms officers, and non-medical service personnel.
The work of a Royal Navy doctor is being implemented by the NHS and the Defence Medical Services for use in the aftermath of terrorist attacks and mass casualty incidents.
Advances in military medicine have often filtered into civilian care, such as blood transfusions in the First World War to the treatment used on casualties in Afghanistan.
Deciding the priority of treatment in mass casualty incidents is known as 'triage' and is vital not only in military situations but is also pivotal in the wake of terrorist attacks in the UK. Key to success in triage is identifying patients who need life-saving interventions.
For years medics have been using flow charts to conduct triage and to determine the priority of treatment for patients in mass casualty incidents.
But recent studies show that the existing method of UK triage (both military and civilian) has only between 28-43% chance of correctly prioritising patients in need of life-saving interventions. https://www.forces.net/news/royal-navy-doctor-changing-way-medics-respond-major-incidents-0
Major incident triage and the implementation of a new triage tool, the MPTT-24
James Vassallo1,2, J E Smith3,4 and L A Wallis1
Author affiliations
Abstract
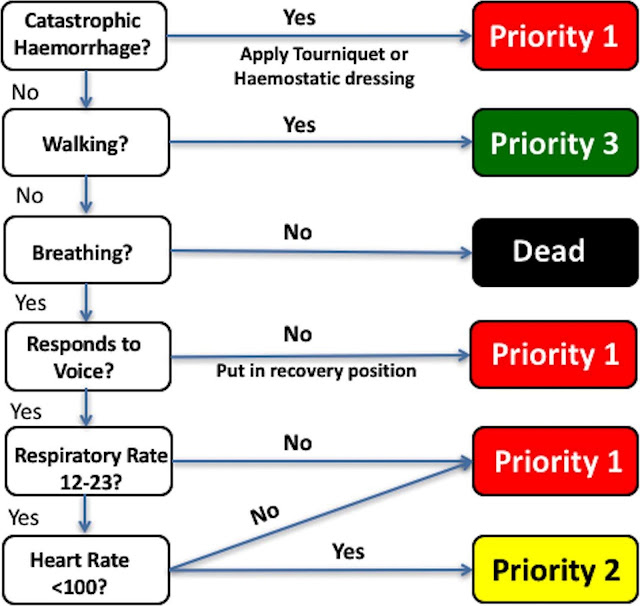
Introduction The Modified Physiological Triage Tool (MPTT) is a recently developed primary triage tool and in comparison with existing tools demonstrates the greatest sensitivity at predicting need for life-saving intervention (LSI) within both military and civilian populations. To improve its applicability, we proposed to increase the upper respiratory rate (RR) threshold to 24 breaths per minute (bpm) to produce the MPTT-24. Our aim was to conduct a feasibility analysis of the proposed MPTT-24, comparing its performance with the existing UK Military Sieve.
Method A retrospective review of the Joint Theatre Trauma Registry (JTTR) and Trauma Audit Research Network (TARN) databases was performed for all adult (>18 years) patients presenting between 2006–2013 (JTTR) and 2014 (TARN). Patients were defined as priority one (P1) if they received one or more LSIs. Using first recorded hospital RR in isolation, sensitivity and specificity of the ≥24 bpm threshold was compared with the existing threshold (≥22 bpm) at predicting P1 status. Patients were then categorised as P1 or not-P1 by the MPTT, MPTT-24 and the UK Military Sieve.
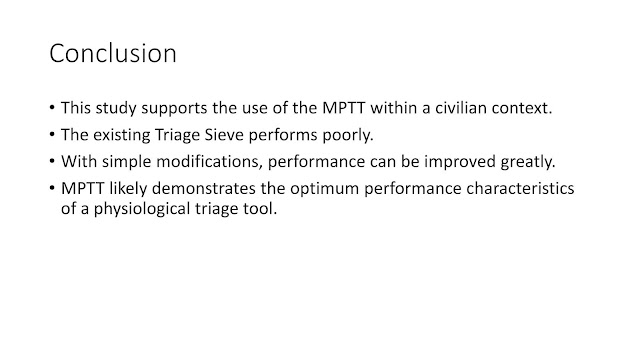
Results The MPTT and MPTT-24 outperformed existing UK methods of triage with a statistically significant (p<0 .001="" 25.5="" 29.5="" a="" absolute="" an="" and="" as="" between="" both="" cases="" categorised="" compared="" demonstrated="" difference="" in="" increase="" jttr="" mptt-24="" mptt.="" mptt="" observed="" of="" p1="" p="" populations="" reduction="" sensitivity="" significant="" span="" specificity="" statistically="" tarn="" the="" they="" was="" way="" when="" with="">0>
Conclusions When compared with the existing MPTT, the MPTT-24 allows for a more rapid triage assessment. Both continue to outperform existing methods of primary major incident triage and within the military setting, the slight increase in undertriage is offset by a reduction in overtriage. We recommend that the MPTT-24 be considered as a replacement to the existing UK Military Sieve.
This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/
http://dx.doi.org/10.1136/jramc-2017-000819
The Modified Physiological Triage Tool (MPTT) was derived on a military cohort using logistic regression and outperforms all existing triage tools at predicting the need for life-saving intervention in both military and civilian populations.
Increasing the upper respiratory rate threshold to 24 (MPTT-24) allows for a reduction in the time required to use the triage tool.
Using the Alert; responds to Verbal stimulus; responds to Painful stimulus; Unresponsive (AVPU) scale as supposed to the GCS to measure conscious level will enable the MPTT-24 to be used by a greater number of personnel, increasing its applicability.
Performance of the MPTT-24 is largely unchanged from the MPTT, and it clinically and statistically outperforms the existing UK Military Sieve at predicting the need for life-saving intervention.
We recommend that the MPTT-24 be considered as an alternative to the existing UK Military Sieve for the purposes of primary major incident triage in the military setting.
Introduction
Triage is the process of prioritising patients on the basis of their clinical acuity and is a key principle of effective major incident management.1 Within the UK, existing military and civilian doctrine utilises a two-stage approach to triage with primary and secondary triage being performed. Primary triage is a quick assessment of the patient, conducted at the scene and is frequently performed in difficult settings. For it to be effective, it must be rapid, reliable and reproducible, irrespective of the provider using it.1
The UK Military Sieve and National Ambulance Resilience Unit Sieve are the algorithms used by the Defence Medical Services and Ambulance Services, respectively, for primary major incident triage.2 3 Utilising simple physiological assessments, patients are categorised into one of three categories with priority one the most urgent. Secondary triage takes place in a more permissive environment, such as at a casualty clearing station or at the hospital entrance. Unlike primary triage, it is a more thorough assessment of the patient, frequently performed by more experienced and senior clinicians. If needed, it allows for the refinement of the triage category allocated during the primary triage process prior to treatment or admission to hospital.1
A number of studies have shown that existing methods of triage have limited accuracy at predicting the need for life-saving intervention in both the military and civilian environments.4 Derived specifically for this purpose, the Modified Physiological Triage Tool (MPTT) has shown the greatest sensitivity for predicting the need for life-saving intervention, with the lowest rates of undertriage and acceptable levels of overtriage in both military and civilian populations.5–7
Respiratory Rate (RR) and Glasgow Coma Scale (GCS) form key components of the MPTT and can both be time consuming to accurately measure, with significant inter-rater reliability being described previously.8 We propose to modify the MPTT by increasing the upper respiratory rate threshold to 24 breaths per minute (MPTT-24), allowing providers to more easily do a 15 second RR count and multiply by four (or 10 seconds and multiply by six), thereby potentially halving the time currently required to use the MPTT. In addition, we have adopted the Alert; responds to Verbal stimulus; responds to Painful stimulus; Unresponsive (AVPU) scale for the purposes of the conscious level assessment, replacing the existing GCS<14 10="" assessment.9="" span="">14>
Accepting a more pragmatic approach—with a threshold RR which is easily calculated within a shorter time frame—may change the test characteristics of the MPTT. The aim of this study was to conduct a feasibility analysis of the proposed MPTT-24 and compare its test characteristics with both the original MPTT and the existing UK Military Sieve.
Materials and methods
A retrospective review of the Joint Theatre Trauma Registry (JTTR) and Trauma Audit Research Network (TARN) databases was performed for all adult (>18 years) patients presenting between 2006–2013 (JTTR) and 2014 (TARN).
The JTTR holds data on all seriously injured patients treated by UK Defence Medical Services in the deployed setting with continuous data available from 2003. The default entry criterion was a patient who triggered trauma team activation, but this was expanded in 2007 to include all patients with trauma who were returned to the Royal Centre for Defence Medicine for definitive treatment.5 11 Established in 1988, TARN is the largest trauma database in Europe, collecting data from all trauma receiving hospitals in England and Wales on patients with moderate to severe injuries and contains data from point of injury through to discharge. TARN inclusion criteria include hospital admission >3 days, admission to critical care or death in hospital.12 13 Patients declared dead at scene and not conveyed to hospital are not included in the database. Patients were assumed to be non-ambulant due to the nature of the TARN database and its inclusion criteria.6
Patients were defined as priority one (P1) if they had received one or more life-saving interventions from a previously defined list, derived through international consensus of experts involved in major incident management (Figure 1).14 Using first recorded hospital RR in isolation, the sensitivity and specificity of the ≥24 breaths per minute threshold were compared with the existing threshold (≥22 breaths per minute) at predicting P1 status. Patients were then categorised as P1 or not-P1 by the MPTT, the MPTT-24 (Figure 2) and the UK Military Sieve. A McNemar test was used to determine statistical significance between the triage tools.
Life-saving interventions defining the priority one patient. ACLS, advanced cardiovascular life support.
Modified Physiological Triage Tool (MPTT)-24 algorithm with increased respiratory rate upper threshold (≥24), conscious level assessment using Alert; responds to Verbal stimulus; responds to Painful stimulus; Unresponsive (AVPU scale) and the additional assessment for external catastrophic haemorrhage. Vassallo 2017. CC BY 4.0
Ethics statement
The use of the JTTR was approved by the Medical Directorate, Royal Centre for Defence Medicine. Additionally, as part of a larger programme of work, this study received ethical approval from the Human Research Ethics Committee of the University of Cape Town, the primary academic institution of the lead author (reference 285/2013).
Results
Basic study characteristics are shown in table 1. In both populations, the increased threshold in RR in isolation was associated with an absolute reduction in sensitivity (TARN 11.4%, JTTR 13.5%) and an increase in specificity (TARN 8.9%, JTTR 13.8%). An increase in OR and positive predictive value was observed when using a higher RR for both TARN and JTTR (table 2).
Performance analysis of test characteristics for RR (≥22 and 24 thresholds), MPTT, MPTT-24 and the existing UK Military Sieve
When incorporated into the MPTT-24, an absolute reduction in sensitivity was observed (TARN 8.9%, JTTR 3.2%) with an increase in specificity. There was a statistically significant difference between the MPTT and MPTT-24 in the way they categorised TARN and JTTR cases as P1 (p<0 .001="" span="">0>
The MPTT-24 demonstrated a statistically significant (p<0 .001="" 23.5="" 25.5="" a="" ability="" existing="" identify="" in="" increase="" intervention.="" its="" jttr="" life-saving="" military="" need="" of="" over="" sensitivity="" sieve="" span="" the="" those="" to="" uk="">0>
Discussion
In this study, we have demonstrated that pragmatic modifications to the MPTT, in the form of the MPTT-24, can be implemented while maintaining comparable performance at predicting the need for life-saving intervention in both civilian and military trauma registry populations. With these modifications, the MPTT-24 continues to outperform the existing UK Military Sieve.
In keeping with the existing UK Military Sieve,2 we have included an assessment of catastrophic external haemorrhage in the MPTT-24. While experience of such injuries is likely to be limited in day-to-day civilian trauma care, we note previous European terrorist major incidents (Paris 2015 and London 2007) where the demand for tourniquets was high.15 In the context of an ongoing Marauding Terrorist Firearms Attack, the ability to provide treatment will be limited; controlling catastrophic external haemorrhage through tourniquets or haemostatic dressings may help to preserve life until the incident becomes more permissive.
The MPTT assesses the patient’s conscious level using the GCS, with patients scoring 13 or lower being considered P1. While this represents the optimum threshold of conscious level at predicting need for life-saving intervention, it is not without limitations.5 Previous studies have demonstrated wide inter-rater reliability when using the GCS.8 Calculating the GCS requires familiarity and prior experience with the scale, but even then it can be time consuming. The AVPU score was designed as a rapid assessment of conscious level and is a simpler alternative to the GCS.16 17 A number of studies have looked at the correlation between GCS and AVPU with agreement that the division between being ‘alert’ and ‘responds to voice’ occurs at a median GCS of 13.9 16 18 For the purposes of simplifying the conscious level assessment in the primary triage process, we have replaced ‘GCS<14 able="" allow="" and="" applicability="" be="" both="" in="" incident="" increasing="" its="" limited="" major="" medical="" mptt-24.="" mptt-24="" pragmatic="" responds="" results="" setting.="" should="" similar="" span="" step="" the="" this="" thus="" to="" training="" usability="" use="" users="" voice="" with="">14>
A key principle of primary major incident triage is that it can be conducted rapidly and measuring the respiratory rate can be time consuming. By increasing the upper respiratory rate threshold of the MPTT, users are able to measure the respiratory rate over a 15 second period, allowing for a potential reduction in the time required to prioritise patients with the MPTT-24 by up to 15 seconds. If this reduction is applied to a theoretical scenario with 20 patients requiring triage, then up to 5 min could be saved by using the MPTT-24 rather than the MPTT. However, we acknowledge that this increased threshold is unlikely to convey any additional time benefit if users choose to measure the respiratory rate over a 30 second period.
Adopting the MPTT-24 comes at the expense of a reduction in sensitivity and therefore a higher rate of undertriage (1 - sensitivity). Clinically, this increased rate in undertriage is negligible; within the military setting, 30 genuine P1 patients would need to be assessed before an additional patient is undertriaged by the MPTT-24. Likewise, the reduction in overtriage (1 - positive predictive value)is negligible between the MPTT and MPTT-24 and needs even greater number of patients before a difference is observed.
In the civilian setting, the rate of overtriage for both the MPTT-24 and MPTT is high (66.0% and 67.1%, respectively). Although this is comparable to the overall overtriage rate following the London 7/7 attacks (64%),19 we acknowledge that if sustained, this level may not be tolerable in the setting of a non-developed system or rural environment.20 The MPTT and MPTT-24 were designed for the purposes of primary major incident triage alone and not as a replacement to secondary triage. Within the UK, patients will undergo a secondary triage process, with a review of the original triage categories and where appropriate, those initially overtriaged can be reallocated to a lower triage category at the discretion of experienced clinicians, thus reducing the overall overtriage rate.1
A key limitation of our study is the use of first recorded hospital physiology to calculate triage priorities. While prehospital data is recorded on both the JTTR and TARN databases, complete data are available for only 16.7% and 37.2% of military and civilian cases, respectively, making prioritisation with prehospital data unreliable. However, when complete hospital and prehospital physiology were compared in both datasets, we observed that the median and IQR were almost identical.
Conclusion
When compared with the existing MPTT, the MPTT-24 allows for the potential for a more rapid triage assessment, while maintaining comparable performance and continuing to outperform existing methods used in the UK. Within a military setting, the slight increase in undertriage is offset by a reduction in overtriage. We recommend that the MPTT-24 be considered as a replacement to the existing UK Military Sieve for the purposes of primary major incident triage.
Acknowledgments
Our thanks to Professor Fiona Lecky, Research Director and Antoinette Edwards, Chief Executive Officer, at the Trauma Audit and Research Network (TARN) for facilitating access to the TARN database.
References
↵Carley S, Mackway-Jones KAdvanced Life Support Group. Triage. In: Carley S, Mackway-Jones K, Major incident medical management and support. Oxford, UK: Blackwell Publishing Ltd, 2005:97–107.Google Scholar
↵Ministry of Defence. Clinical guidelines for operations (JSP 999). 2013 https://www.gov.uk/government/publications/jsp-999-clinical-guidelines-for-operationsGoogle Scholar
↵National Ambulance Resilience Unit, United Kingdom. NARU input to new triage sieve. 2014. Cited 26 May 2017 https://naru.org.uk/naru-input-to-new-triage-sieve/Google Scholar
↵Challen K, Walter D. Major incident triage: comparative validation using data from 7th July bombings. Injury 2013;44:629–33.doi:10.1016/j.injury.2012.06.026PubMedGoogle Scholar
↵Vassallo J, Beavis J, Smith JE, et al. Major incident triage: derivation and comparative analysis of the Modified Physiological Triage Tool (MPTT). Injury 2017;48:992–9.doi:10.1016/j.injury.2017.01.038Google Scholar
↵Vassallo J, Smith J, Bouamra O, et al. The civilian validation of the Modified Physiological Triage Tool (MPTT): an evidence-based approach to primary major incident triage. Emerg Med J 2017 (accessed 23 Jul 2017) [Epub ahead of print].doi:10.1136/emermed-2017-206647Google Scholar
↵Vassallo J, Horne S, Smith JE, et al. The prospective validation of the Modified Physiological Triage Tool (MPTT): an evidence-based approach to major incident triage. J R Army Med Corps 2017 (Epub ahead of print).doi:10.1136/jramc-2017-000771Google Scholar
↵Gill MR, Reiley DG, Green SM. Interrater reliability of Glasgow Coma Scale scores in the emergency department. Ann Emerg Med 2004;43:215–23.doi:10.1016/S0196-0644(03)00814-XCrossRefPubMedWeb of ScienceGoogle Scholar
↵Kelly CA, Upex A, Bateman DN. Comparison of consciousness level assessment in the poisoned patient using the alert/verbal/painful/unresponsive scale and the Glasgow Coma Scale. Ann Emerg Med 2004;44:108–13.doi:10.1016/j.annemergmed.2004.03.028CrossRefPubMedWeb of ScienceGoogle Scholar
↵Mackay CA, Burke DP, Burke JA, et al. Association between the assessment of conscious level using the AVPU system and the Glasgow Coma Scale. Pre-hospital Immediate Care 2000:17–19.Google Scholar
↵Smith JE. The epidemiology of blast lung injury during recent military conflicts: a retrospective database review of cases presenting to deployed military hospitals, 2003–2009. Philos Trans R Soc Lond B Biol Sci 2011;366:291–4.doi:10.1098/rstb.2010.0251Abstract/FREE Full TextGoogle Scholar
↵Kehoe A, Smith JE, Edwards A, et al. The changing face of major trauma in the UK. Emerg Med J 2015;32:911–5.doi:10.1136/emermed-2015-205265Abstract/FREE Full TextGoogle Scholar
↵Barnard EB, Morrison JJ, Madureira RM, et al. Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA): a population based gap analysis of trauma patients in England and Wales. Emerg Med J 2015;32:926–32.doi:10.1136/emermed-2015-205217Abstract/FREE Full TextGoogle Scholar
↵Vassallo J, Smith JE, Bruijns SR, et al. Major incident triage: a consensus based definition of the essential life-saving interventions during the definitive care phase of a major incident. Injury 2016;47:1898–902.doi:10.1016/j.injury.2016.06.022Google Scholar
↵Hirsch M, Carli P, Nizard R, et al. The medical response to multisite terrorist attacks in Paris. Lancet 2015;386:2535–8.doi:10.1016/S0140-6736(15)01063-6CrossRefPubMedGoogle Scholar
↵Gill M, Martens K, Lynch EL, et al. Interrater reliability of 3 simplified neurologic scales applied to adults presenting to the emergency department with altered levels of consciousness. Ann Emerg Med 2007;49:403–7.doi:10.1016/j.annemergmed.2006.03.031CrossRefPubMedWeb of ScienceGoogle Scholar
↵Kheirabadi AR, Tabeshpour J, Afshari R. Comparison of three consciousness assessment scales in poisoned patients and recommendation of a new scale: AVPU plus. Asia Pac J Med Toxicol 2015;4:58–63.Google Scholar
↵McNarry AF, Goldhill DR. Simple bedside assessment of level of consciousness: comparison of two simple assessment scales with the Glasgow Coma scale. Anaesthesia 2004;59:34–7.doi:10.1111/j.1365-2044.2004.03526.xCrossRefPubMedWeb of ScienceGoogle Scholar
↵Aylwin CJ, König TC, Brennan NW, et al. Reduction in critical mortality in urban mass casualty incidents: analysis of triage, surge, and resource use after the London bombings on July 7, 2005. Lancet 2006;368:2219–25.doi:10.1016/S0140-6736(06)69896-6CrossRefPubMedWeb of ScienceGoogle Scholar
↵Frykberg ER. Medical management of disasters and mass casualties from terrorist bombings: how can we cope? J Trauma 2002;53:201–12.doi:10.1097/00005373-200208000-00001CrossRefPubMedWeb of
Contributors JV conceived the study and conducted the analysis supervised by JES. JV drafted the manuscript and all authors contributed substantially to its revision. JV takes the responsibility for the paper as a whole.
Competing interests JV and JES are serving members of HM Armed Forces.
Provenance and peer review Not commissioned; externally peer reviewed.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Request permissions
Copyright information: © Article author(s) (or their employer(s) unless otherwise stated in the text of the article) 2017. All rights reserved. No commercial use is permitted unless otherwise expressly granted.
This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/
Major Incident Triage: the Civilian validation of Modifed Physiological Triage Tool (MPTT) by The Royal College of Emergency Medicine PPT free Download
https://t.me/joinchat/GRsTvEHYjNLP8yc6gPXQ9Q Para profesionales de emergencias, salud, medicina, desastres, prehospitalaria a nivel global, concentrados principalmente en América Latina y Europa Latina
Dr Ramon REYES, MD,
Por favor compartir nuestras REDES SOCIALES @DrRamonReyesMD, así podremos llegar a mas personas y estos se beneficiarán de la disponibilidad de estos documentos, pdf, e-book, gratuitos y legales..
Por favor compartir nuestras REDES SOCIALES @DrRamonReyesMD, así podremos llegar a mas personas y estos se beneficiarán de la disponibilidad de estos documentos, pdf, e-book, gratuitos y legales..
Grupo Biblioteca/PDFs gratis en Facebook
https://www.facebook.com/groups/PDFgratisMedicina #DrRamonReyesMD
https://www.facebook.com/DrRamonReyesMD
https://www.instagram.com/drramonreyesmd/
https://www.pinterest.es/DrRamonReyesMD/
https://twitter.com/eeiispain
Blog
http://emssolutionsint.blogspot.com/2016/12/dr-ramon-reyes-diaz-md-emt-t-dmo.html
TELEGRAM
Group https://t.me/joinchat/GRsTvEHYjNLP8yc6gPXQ9Q
AED Automatic External Defibrillator . UN compacto, economico y seguro https://emssolutionsint.blogspot.com/2019/08/aed-automatic-external-defibrillator-un.html