
 Background: The cornerstones of sepsis management include early identification, early antimicrobial administration, and source control. The Surviving Sepsis Campaign guidelines recommend that blood cultures be drawn before starting antimicrobial therapy, however, obtaining cultures prior to antibiotics may be challenging due to shorter time windows (i.e. 1hr from identification) to initiate antibiotics. Some may prioritize administering antimicrobial agents before obtaining blood cultures to ensure they meet this core measure. This study (The FABLED Trial) tried to determine the sensitivity of blood cultures obtained both before and after initiation of antimicrobial therapy in patients with severe manifestations of sepsis.
Background: The cornerstones of sepsis management include early identification, early antimicrobial administration, and source control. The Surviving Sepsis Campaign guidelines recommend that blood cultures be drawn before starting antimicrobial therapy, however, obtaining cultures prior to antibiotics may be challenging due to shorter time windows (i.e. 1hr from identification) to initiate antibiotics. Some may prioritize administering antimicrobial agents before obtaining blood cultures to ensure they meet this core measure. This study (The FABLED Trial) tried to determine the sensitivity of blood cultures obtained both before and after initiation of antimicrobial therapy in patients with severe manifestations of sepsis.
What They Did:
- FABLED Trial: eFfect of Antimicrobial administration on Blood Culture positivity in patients with severe manifestations of sepsis in the Emergency Department
- Multicenter, patient-level, single-group, diagnostic study from 7 EDs in North America
- Evaluated the sensitivity of blood cultures obtained before and within 120 minutes of initiation of antimicrobial treatment (protocol was amended to include participants with repeated blood cultures up to 240 minutes after antimicrobial therapy due to difficulties in obtaining repeated blood cultures within 120 minutes of treatment initiation)
Outcomes:
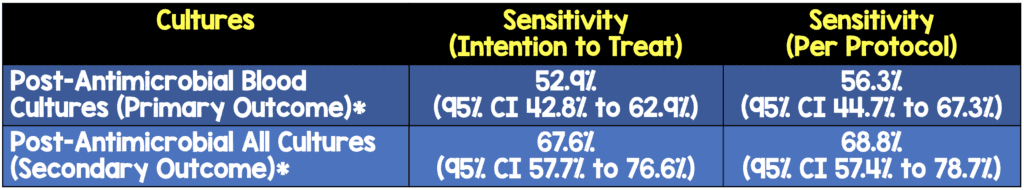
- Primary: Sensitivity of blood cultures obtained within 120 minutes of antimicrobial therapy was initiated in patients with severe manifestations of sepsis
- Secondary: Sensitivity of post-antimicrobial blood cultures interpreted in the context of microbiological culture results available from other anatomical sites
Inclusion:
- Age ≥18 years
- Presenting to ED
- Severe manifestations of sepsis (Definition = SBP <90mmHg or serum lactate ≥4mmol/L)
- 2 sets of blood cultures done before and within 2hrs after starting antimicrobial treatment
Exclusion:
- Potential risk of harm from additional venipuncture:
- Clinically significant bleeding disorder
- Platelet count <20,000 x109 cells/L
- INR > 6.0
Results:
- 3164 patients screened
- 442 patients were eligible to be included in the study (≈25% excluded due to the following reasons: Declined to participate, were assessed >2hr after initiation of antibiotics, did not receive antibiotic tx in the ED, had hypocoaguable state, died before repeat blood cxs)
- 325 patients included in the study
- 264 (81.2%) patients had post-antimicrobial blood cultures drawn between 30 and 120 minutes after initiation of antimicrobial therapy
- Median time to blood cultures being repeated after antimicrobial therapy = 70 minutes (Range 50 – 110 minutes)
- Most common sites of infection: Respiratory (32.9%), GU (17.8%), and GI (16.9%)
- Most common organisms isolated from pre-antimicrobial blood cultures were Escherichia coli (22.5%), Staphylococcus aureus (15.7%), and Streptococcus pneumoniae (12.7%)
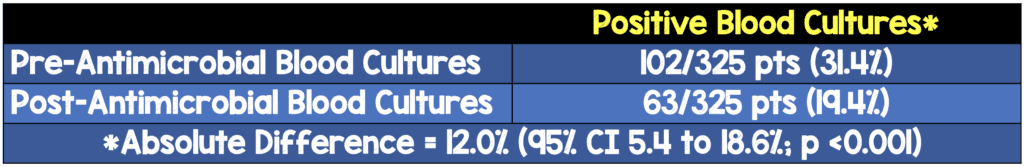
*Pre-antimicrobial blood cultures were the reference standard for bacteremia. Therefore, a noncontaminant organism growing in any of the pre-antimicrobial blood cultures but absent from all post-antimicrobial blood cultures was defined as a discordant result. In the setting of a polymicrobial bloodstream infection, all noncontaminant organisms recovered in the pre-antimicrobial blood cultures must have been present in the post-antimicrobial blood cultures to have been considered concordant
- If we drew blood cultures after antibiotic administration this would equate to 1 in every 6.7 patients having a false-negative blood culture result!!! (See Discussion)
Strengths:
- Investigators remained unaware of the results throughout the enrollment period
- All potential blood culture contaminants were reviewed by 2 specialists in infectious diseases and medical microbiology
- Almost all study participants had complete data for the exposures and outcomes of interest (i.e. 5 patients were omitted due to missing data)
- Baseline characteristics were similar between groups with one exception…patients with positive pre-antimicrobial blood cultures were more likely to have respiratory failure (19.6% vs 8.9%) than patients with negative pre-antimicrobial blood cultures, which should have no impact on the outcomes of this study
- 1st study to prospectively quantify the decrease in sensitivity of blood culture sensitivity from the time of antimicrobial initiation
- Included cultures from other sources (i.e. Not blood cultures) to determine sensitivities of the original blood cultures
Limitations:
- There was a significant proportion of patients who had repeated blood cultures obtained outside the time window specified in the study protocol (i.e. 30 to 120 minutes after antibiotic initiation)
- Proportion of bacteremic patients (31.4%) was slightly lower than the expected (35%) in order to obtain a 90% power for this study
- The quantity of blood cultured differed among study sites due to local differences in study protocol and laboratory practices. This could affect the results of positive blood cultures and therefore inflate the difference in results (Total blood volume cultured before and after antimicrobial administration was different but at least 20mL)
- This was a convenience sample, with patients recruited only when study investigators were on site to screen and enroll patients. This means many patients may have not been enrolled and therefore not representative of an entire population and could result in a sampling bias
Discussion:
- Authors took into account contaminant organisms which they defined as low-virulence skin flora recovered from a single set of blood cultures when other sets were negative
- This was a decently sick patient population with 43.4% having serum lactate ≥4mmol/L, 37.8% having SBP <90mmHg, and 18.8% having both
- Although, 1 in 6.7 false negative patients is not a number to balk at, it is probably worth asking does the false negative blood cultures matter or do we care due to the potential to tailor our treatment? Approximately 70% of septic patients had negative blood cultures when they were drawn prior to antibiotics, and 80% of septic patients had negative blood cultures when they were drawn after antibiotics. Therefore, this would only affect an additional 10% of patients in which we could expand or narrow antibiotic coverage. This is simply a disease-oriented outcome (DOO), but the more important question, which this study doesn’t answer is what is the patient-oriented outcome (POO)?
Author Conclusion: “Among patients with severe manifestations of sepsis, initiation of empirical antimicrobial therapy significantly reduces the sensitivity of blood cultures drawn shortly after treatment initiation.”
Clinical Take Home Point: In a relatively sick septic patient population, drawing blood cultures after administration of antibiotic treatment reduces culture sensitivity which could affect downstream optimization of treatment as well as safe de-escalation of treatment.
References:
- Cheng MP et al. Blood Culture Results Before and After Antimicrobial Administration in Patients with Severe Manifestations of Sepsis: A Diagnostic Study. Ann Intern Med 2019. PMID: 31525774
For More on This Topic Checkout:
- The Bottom Line: FABLED
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)
The post The FABLED Trial: Blood Cultures 1st, Then Antibiotics in Sepsis appeared first on REBEL EM - Emergency Medicine Blog.

