
 Background: In patients with stable coronary artery disease the goals of treatment are to reduce the risk of death, ischemic events, and to improve quality of life. In order to achieve those objectives all patients with coronary artery disease should be treated with guideline based medical therapy. Currently, many of them undergo elective angiography and placement of stents if needed when they have abnormal stress tests. Before the widespread use of drug-eluting stents, trials evaluating incremental effects of revascularization added to medical therapy did not show a reduction in the rates of death or MI. However, those trials did not include sufficient numbers of participants, and only included those with known coronary anatomy prior to randomization.
Background: In patients with stable coronary artery disease the goals of treatment are to reduce the risk of death, ischemic events, and to improve quality of life. In order to achieve those objectives all patients with coronary artery disease should be treated with guideline based medical therapy. Currently, many of them undergo elective angiography and placement of stents if needed when they have abnormal stress tests. Before the widespread use of drug-eluting stents, trials evaluating incremental effects of revascularization added to medical therapy did not show a reduction in the rates of death or MI. However, those trials did not include sufficient numbers of participants, and only included those with known coronary anatomy prior to randomization.
Paper: Maron D.J et al. Initial Invasive or Conservative Strategy for Stable Coronary Disease. NEJM 2020. PMID: 32227755.
Clinical Question: In patients with stable coronary artery disease and moderate to severe ischemia, does the addition of routine invasive therapy to optimal medical therapy (conservative) alone improve clinical outcomes?
What They Did:
- International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (ISCHEMIA)
- International multi-center (320 sites in 37 countries) parallel randomized trial with 5,179 participants with moderate or severe ischemia on stress testing
- Participants were randomized to
- Routine invasive strategy (n= 2,588) with cardiac catheterization followed by revascularization (PCI or CABG) if feasible + optimal medical therapy (OMT) [lifestyle modifications and pharmacologic intervention]
- Conservative strategy (n=2,591) of OMT with cardiac catheterization and revascularization reserved for those who fail OMT
- Duration of follow-up = 3.3 years
Outcomes:
-
Primary:
- Composite endpoint of:
- Death due to cardiovascular (CV) causes
- Non-fatal myocardial infarction (MI)
- Hospitalization for resuscitated cardiac arrest, unstable angina, heart failure
-
Secondary (major):
- Composite endpoint of:
- Death from CV causes
- MI and angina-related quality of life
- Composite endpoint of:
- Composite endpoint of:
Inclusion:
- Moderate to severe ischemia on noninvasive stress testing
- Age ≥ 21 years
Exclusion:
- estimated glomerular filtration rate (eGFR) <30 mL/min/1.73m2
- recent myocardial infarction (MI)
- left ventricular ejection fraction <35%
- left main stenosis >50% (from blinded computed tomography) *
- Class III or IV heart failure (NY Heart Association classification)
- Unacceptable angina at baseline despite maximal medical therapy (at maximum acceptable doses)
- Prior PCI or CABG within last year
- Many other exclusion criteria were mentioned in the original trial (e.g pregnancy, severe valvular disease, non-adherence to medication, weight exceeding size limit for CCTA, cardiac transplant…etc)
* Most enrolled participants with normal renal function first underwent blinded coronary computed tomography angiography (CCTA) to exclude those with left main coronary artery disease (CAD) and without obstructive CAD. Of the 5,179-undergoing randomization, 73.0% (3783) underwent blinded CCTA.
Results:
- 5179 patients randomized
- Invasive strategy group
- 96% underwent angiography
- 79% underwent revascularization (74% PCI, 26% CABG)
- Total numbers of invasive procedures 5337
- Conservative strategy group
- 26% underwent angiography
- 21% underwent revascularization
- 19% underwent angiography and 15% underwent revascularization before the occurrence of a primary outcome
- Total number of invasive procedures 1506
- Invasive strategy group
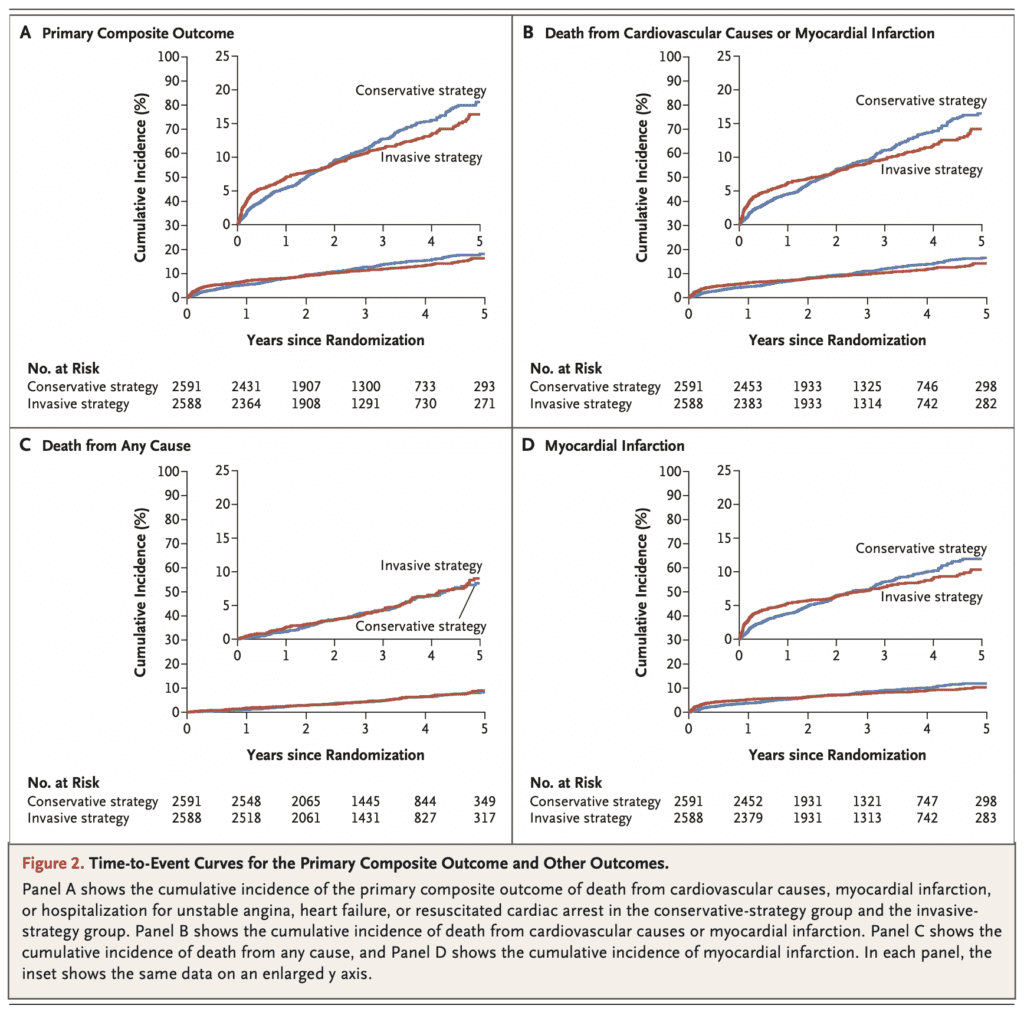
- Primary Outcome:
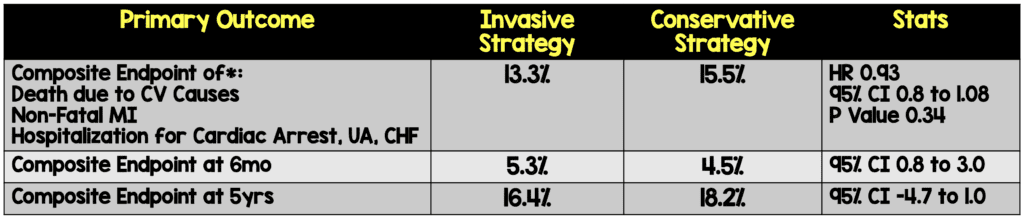
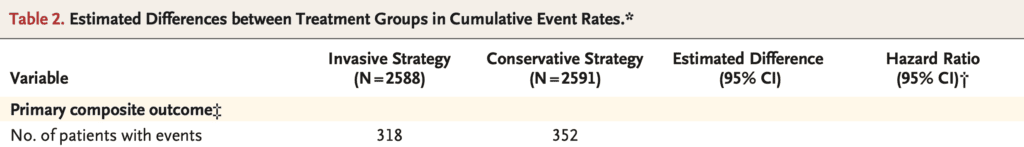
*These numbers don’t seem to match Table 2 in the document:
Invasive Strategy: 318/2588 = 12.3%
Conservative Strategy: 352/2591 = 13.5%
-
- Invasive therapy was associated with harm (~2% absolute increase) within the first 6 months and benefit within 4 years (~2% absolute decrease)
- Before trial launch the primary outcome was changed to a composite of death from cardiovascular causes or MI, with a protocol to revert to the original five-component primary outcome if needed to preserve statistical power. Slow recruitment and lower than expected aggregated event rates triggered this prespecified contingency plan. With the secondary definition of MI, the estimated cumulative event rate for the primary outcome:
- At 6 months 10.2% invasive strategy vs 3.7% in conservative strategy (95% CI 5.2 – 7.9)
- At 5 years 21.2% invasive strategy vs 19.0% conservative strategy (95% CI -0.7 to 5.2%)
- Secondary Outcomes:
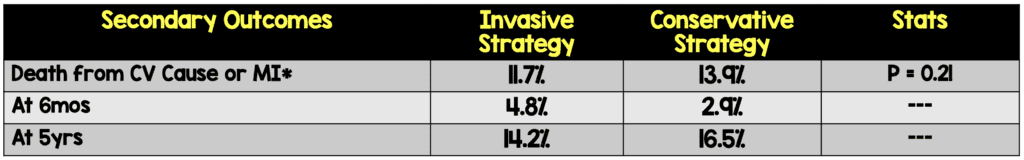
*These numbers also don’t seem to match Table 2:
Invasive Strategy: 276/2588 = 10.7%
Conservative Strategy: 314/2591 = 12.1%
-
- The restricted mean time free from death from CV causes or MI over 5 years was similar in the two groups (9.4 days longer in the invasive-strategy group; 95% CI, -16.5 to 35.2)
- All cause death
- 6.4% of the invasive group
- 6.5% of the conservative group
- p = 0.67
- Again, these numbers don’t seem to match Table 2:
- 145/2588 (5.6%) in the invasive strategy group
- 144/2591 (5.6%) in the conservative strategy group
- Periprocedural myocardial infarction: (invasive/conservative hazard ratio [HR] 2.98, 95% confidence interval [CI] 1.87-4.74)
- Spontaneous myocardial infarction: (invasive/conservative HR 0.67, 95% CI 0.53-0.83)
- Other outcomes
- More hospitalization from heart failure and in invasive strategy group
- Fewer hospitalizations from unstable angina in invasive strategy group
Strengths
- Large multicenter, international study. Can be externally validated.
- CCTA was blinded, and randomization was done well.
- Well balanced randomization between two groups
- Baseline risk factor and medication use similar in both groups
- Over 99% of projected follow-up in both groups were completed
- The option of exercise-stress testing without imaging was added as a protocol addendum in 2014 to improve recruitment and generalizability of trial results
- Clinical outcomes were adjudicated by an independent clinical-event committee whose members were unaware of trial group assignments
- Industry sponsors did not have access to the data during the trial and did not participate in the trial design, data analysis, or manuscript preparation
- Used intention-to-treat analysis which extrapolates to real world practice
Limitations
- The power was decreased by reducing the sample size from 8000 to 5179 patients. This may have led to fewer event rates than expected
- The period of follow-up (3.2 years) was modest. Event rates past the median are subject to progressively greater uncertainty.
- During the investigation, a secondary definition of MI (whether or not procedural infarctions were included) was used. This had an effect on the analysis and increased sensitivity, thus the differences in event rates between the groups were greater in early follow-up.
- The findings of this study do not apply to patients with acute coronary syndromes including clinically significant left main coronary artery disease, low EF (Class II or IV heart failure), or those patients that are symptomatic despite the use of medical therapy at maximum acceptable doses
- Results of this trial should be interpreted in the context of quality of life outcomes and not mortality outcomes
Discussion:
- The definition of nonprocedural infarction was based on the 3rd Universal Definition of Myocardial Infarction types [3]
- Type 1: Spontaneous MI
- Type 2: Secondary MI
- Type 3: Sudden Death MI
- Type 4a: MI related to PCI
- Type 4b: MI related to stent thrombosis
- Type 4c: MI related to stent restenosis
- Type 5: MI related to CABG
- Silent MI
- Of the 8,518 patients enrolled, 3,339 were excluded for the following reasons:
- 1350 did not have moderate or severe ischemia according to stress testing
- 1218 did not have obstructive CAD
- 434 had unprotected LMCA disease (Defined as ≥50% LMCA stenosis without a bypass graft to the LAD)
- Authors also applied a Bayesian analysis to evaluate the post-trial probability of the 5-year rates of the primary outcome being greater than 3% as well as the 5-year rates of death being greater than 1%:
- 5-year rates of primary outcome >3%:
- 24.5% difference favoring invasive strategy & <0.1% favoring conservative strategy
- 5-year rates of death >1%:
- 10.7% difference favoring invasive strategy & 32.1% difference favoring conservative strategy
- Bayesian analysis uses probability to express beliefs about unknown quantities and clinical hypotheses in light of prior beliefs and the current study data
- 5-year rates of primary outcome >3%:
- Differences in Event Rates:
- Early Follow-Up: Initially the primary composite outcome (death from CV causes, MI, or hospitalization for unstable angina or heart failure) was more frequent in the invasive strategy group than in the conservative strategy group (5.3% vs. 3.4% at 6 months), due to procedure-related MI’s.
- Later Follow-Up: After about 2 years, the event curves crossed, and at 5 years, the incidence of the primary outcome was slightly higher in the conservative-strategy group (18.2% and 16.4%)
- Overall mortality was identical in the two groups
Author conclusion: “Among patients with stable coronary disease and moderate or severe ischemia, we did not find evidence that an initial invasive strategy, as compared with an initial conservative strategy, reduced the risk of ischemic cardiovascular events or death from any cause over a median of 3.2 years. The trial findings were sensitive to the definition of myocardial infarction that was used.”
Clinical Take Home Points:
- There is no need to rush to the cath lab after an abnormal stress test. Optimizing medical therapy and assessing response to therapy does not place patients at greater risk. If the patient’s symptoms and angina do not improve with OMT, then an invasive strategy is appropriate.
- In patients with stable moderate – severe coronary disease there were no clinically meaningful differences in outcomes over 4 years in those who were randomized to a conservative versus early invasive strategy.
- Clinicians can use the results of the ISCHEMIA trial in a shared decision–making process with their patients. However, we need additional analyses that enable us to use a risk-score tool in order to provide more precise advice to patients about the relative advantages/ risks of the two strategies.
- We should wait for a longer-term follow-up to see if any benefits of the invasive strategy become evident over time.
Guest Post By:

Leen Alblaihed, MBBS, MHA
Director of Residency Education
University of Maryland Upper Chesapeake Health Systems
Adjunct Assistant Professor
University of Maryland School of Medicine.
Baltimore, Maryland
Twitter: @LeenAlblaihed
References:
- Maron D.J et al. Initial Invasive or Conservative Strategy for Stable Coronary Disease. NEJM 2020. PMID: 32227755.
- Spertus JA et al. Health-Status Outcomes with Invasive or Conservative Care in Coronary Disease. NEJM 2020. PMID: 32227753
- Thygesen K et al. Third Universal Definition of Myocardial Infarction. JACC 2012. PMID: 22958960
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post The ISCHEMIA Trial: Initial Invasive or Conservative Strategy for Stable Coronary Disease? appeared first on REBEL EM - Emergency Medicine Blog.
