
 Background: In patients with acute respiratory distress syndrome (ARDS) the National Heart, Lung, and Blood Institute ARDS clinical trials network recommends a target partial pressure of arterial oxygen (Pao2) between 55 and 80 mmHg. Goals of arterial oxygenation are not based on robust experimental data and prior evidence has shown the feasibility of targeting a lower partial pressure of arterial oxygen in patients with ARDS. The authors of this trial, aptly named the study, LOCO2 (Liberal Oxygenation vs Conservative Oxygenation). They sought to determine whether a lower oxygen strategy was safe in patients with ARDS.
Background: In patients with acute respiratory distress syndrome (ARDS) the National Heart, Lung, and Blood Institute ARDS clinical trials network recommends a target partial pressure of arterial oxygen (Pao2) between 55 and 80 mmHg. Goals of arterial oxygenation are not based on robust experimental data and prior evidence has shown the feasibility of targeting a lower partial pressure of arterial oxygen in patients with ARDS. The authors of this trial, aptly named the study, LOCO2 (Liberal Oxygenation vs Conservative Oxygenation). They sought to determine whether a lower oxygen strategy was safe in patients with ARDS.
Paper: Barrot, M.D et al. Liberal or Conservative Oxygen Therapy for Acute Respiratory Distress Syndrome. NEJM 2020. PMID: 32160661
Clinical Question: Does targeting the lower limit of recommended partial pressure of arterial oxygen (PaO2) improve outcomes in patients with ARDS?
What They Did:
- This was a prospective, comparative, randomized, multicenter, open study that took place in 13 ICUs in France (June 2016 to September 2018).
-
Patients with ARDS who have been intubated and mechanically ventilated for less than 12 hours are enrolled and allocated to either:
- Liberal Oxygen arm (LO) (target Pao2 90 to 105 mmHg; Sp02 > 96%)
- Conservative Oxygen arm (CO) (target Pao2 55 to 70 mmHg; Sp02 88 to 92%)
- The intervention continued for the first 7 days of mechanical ventilation, or until the patient was extubated (if less than 7 days)
- The same protocols and mechanical ventilation strategies were used in both groups.
- Sp02 levels were maintained at > 96% in the liberal group, and between 88% and 92% in the conservative group
Outcomes:
-
Primary
- Death from any cause at 28 days
-
Secondary
- Death in the ICU and at Day 90
- Days free of mechanical ventilation in ICU
- Sequential Organ Failure Assessment (SOFA) Score [calculated without the respiratory component at day 0, 3 and 7]
- Ventilator associated pneumonia [during the first 28 days]
- Septicemia [during the first 28 days]
- Sepsis-related Organ Failure Score (SOFA)
-
Score of morbidity [at day 28 ]
- This score is based on three points: need for mechanical ventilation, need for morbidity are renal replacement therapy, need of catecholamine or need for ventilation
-
Cardiovascular complications
- New onset of arrhythmia, cardiac ischemia and the use of vasopressors (recorded every morning over first 7 days)
- Respiratory weaning success at days 28 and 90
-
Neurological status
- measured with daily Richmond Agitation Sedation Scale score (RASS), seizures, new stroke on imaging, daily sedation doses, neuroleptic administration and delirium.
-
Antibiotic consumption (first 28 days)
- Number of days exposed to antibiotics divided by the number of days spent in ICU
- Respiratory autonomy [on day 28 and 90 ]
- Need for oxygen or mechanical ventilation support
Inclusion:
-
Intubated due to ARDS and receiving mechanical ventilation for less than 12 hours.
-
ARDS defined according to the Berlin definition:
- Hypoxemia defined with PaO2/FiO2 ratio less or equal to 300 mmHg with PEEP higher or equal to 5 cmH20,
- Less than 7 days between a known clinical insult or new or worsening of respiratory symptoms
- Bilateral opacities on chest Imaging not fully explained by effusions, lobar or lung collapse, or nodules
- Respiratory failure not fully explained by cardiac failure or fluid overload
-
ARDS defined according to the Berlin definition:
Exclusion:
- Long term oxygen therapy or noninvasive ventilation at home
- Cardiac arrest as the reason for ICU hospitalisation
- Traumatic brain injury or cranial hypertension as the reason for ICU hospitalisation
- Pregnancy
- Patient less than 18 years old
- Sickle cell disease
- Patient deprived of freedom or under a legal protective measure
- Hemoptysis with embolization or surgery
- Extracorporeal life support or Extracorporeal Membrane Oxygenation before randomization
- COPD with oxygen or non invasive ventilation at home (obstructive sleep apnoea syndrome is not an exclusion criteria)
- Patient with very high risk of death with IGS II (Simplified Severity Index II) than 90
- Indication of hyperbaric oxygenation : carbon monoxide intoxication, gas embolism, necrotizing fasciitis
- Cyanide intoxication, methemoglobinemia
- Untreated pneumothorax
- Lymphangitis carcinomatosa
- Eosinophilic pneumonia
- Intensive care management for organ donation
- Participation in another interventional study with mortality as a major outcome to avoid confounding factor
- Patient not affiliated to social security
Results:
- 396 patients were assessed for eligibility
- 191 were excluded (based on the above exclusion criteria)
-
205 underwent randomization*
-
103 assigned to conservative oxygen therapy
- 4 were excluded
- 99 were included in the analysis
- 102 assigned to liberal oxygen therapy, all were included in analysis with no exclusions.
-
103 assigned to conservative oxygen therapy
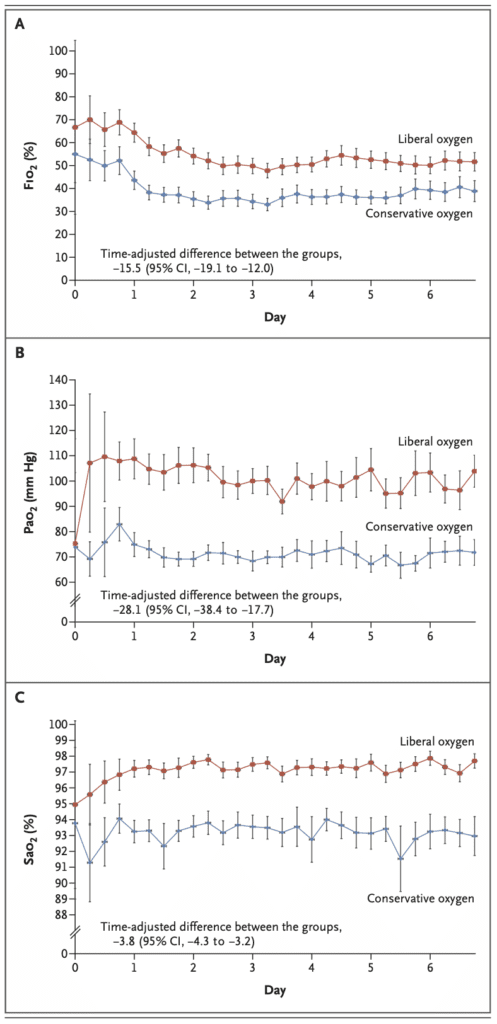
- During the 7 days of the protocol the mean Pa02, Sa02 and Fi02 were significantly lower in the conservative group
-
Primary outcome
-
At day 28, no significant difference in mortality between the two groups.
- 34 of 99 patients (34.3%) in the conservative group
- 27 of 102 (26.5%) in the liberal group
- Difference 7.8 percentage points; 95% CI -4.8 to 20.6
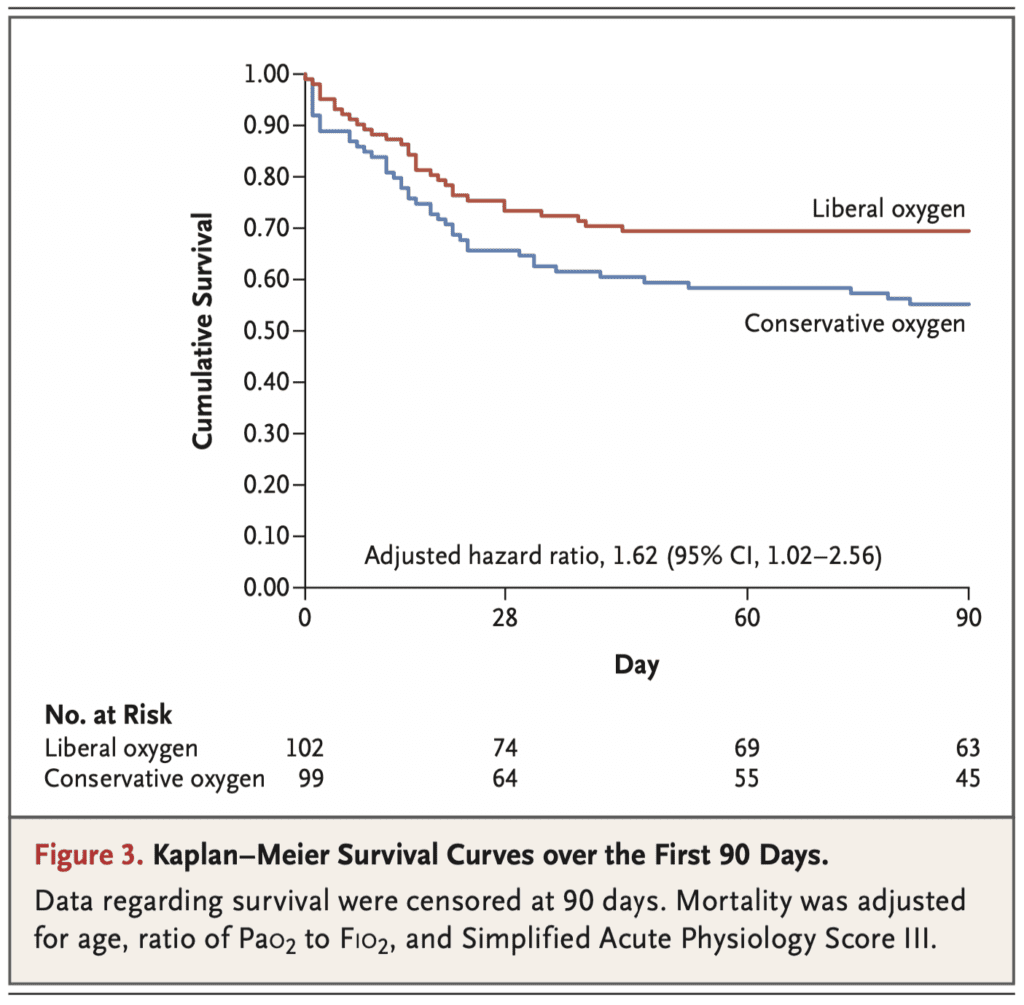
- At day 90, mortality was significantly higher in the conservative group (44.4% vs 30.4% in the liberal group). Difference: 14.0%; 95% CI 0.7 to 27.2
-
At day 28, no significant difference in mortality between the two groups.
- 5 mesenteric ischemia events occurred in the conservative group, and none in the liberal group
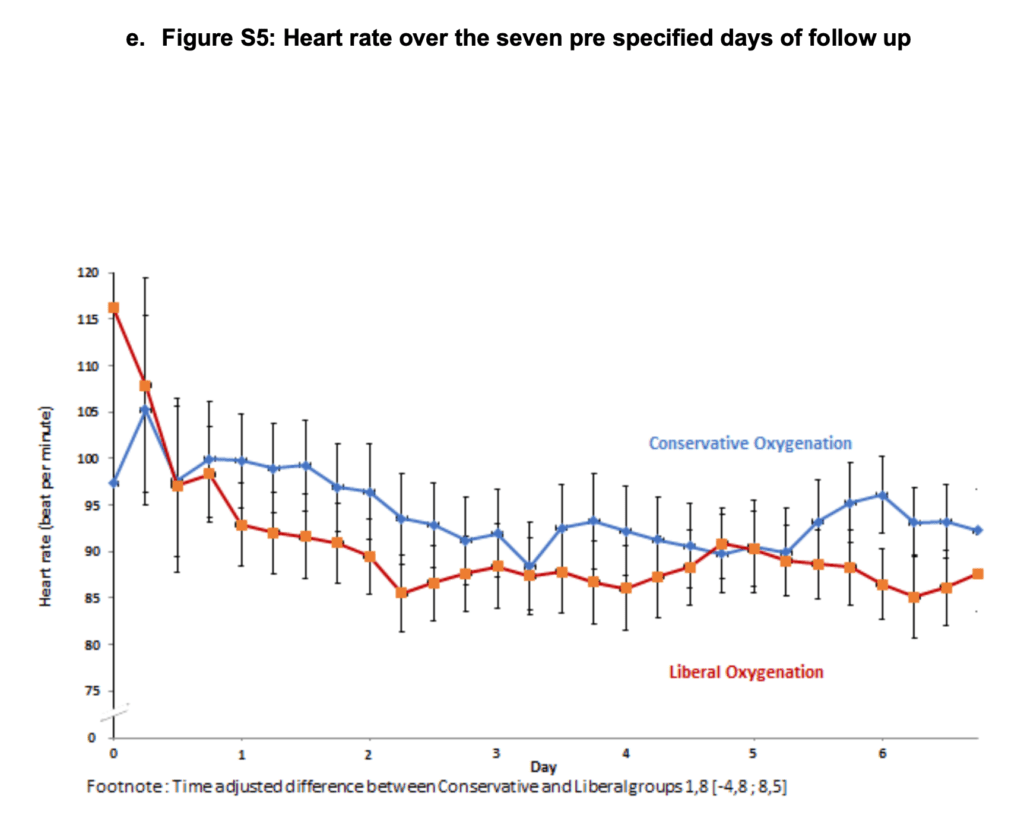
- Patients in the conservative group had higher heart rates than those in the conservative group.
- Other outcomes such as neurologic adverse events, cardiovascular events (e.g arrhythmias) and infections (e.g ventilator associated pneumonia) were similar in both groups.
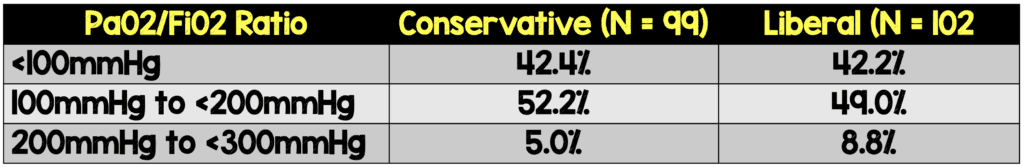
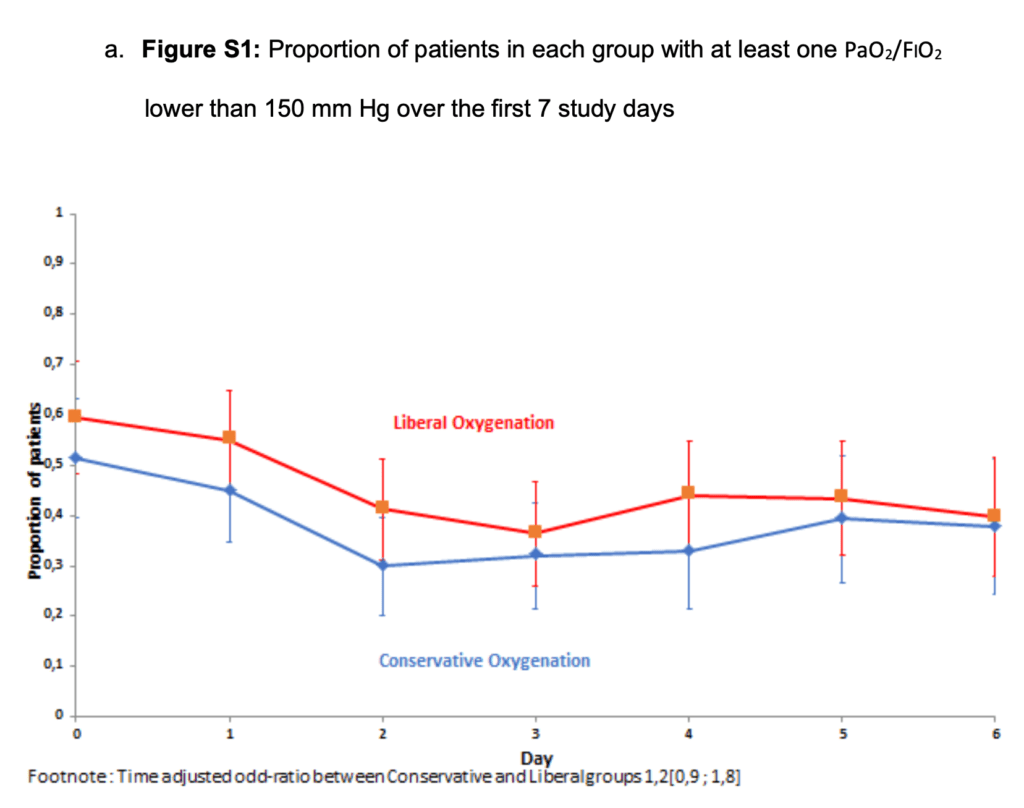
- While Pa02 was higher in the liberal arm (per protocol) there were more patients with the Pa02:Fi02 ratio lower than 150 over the 7 day period.
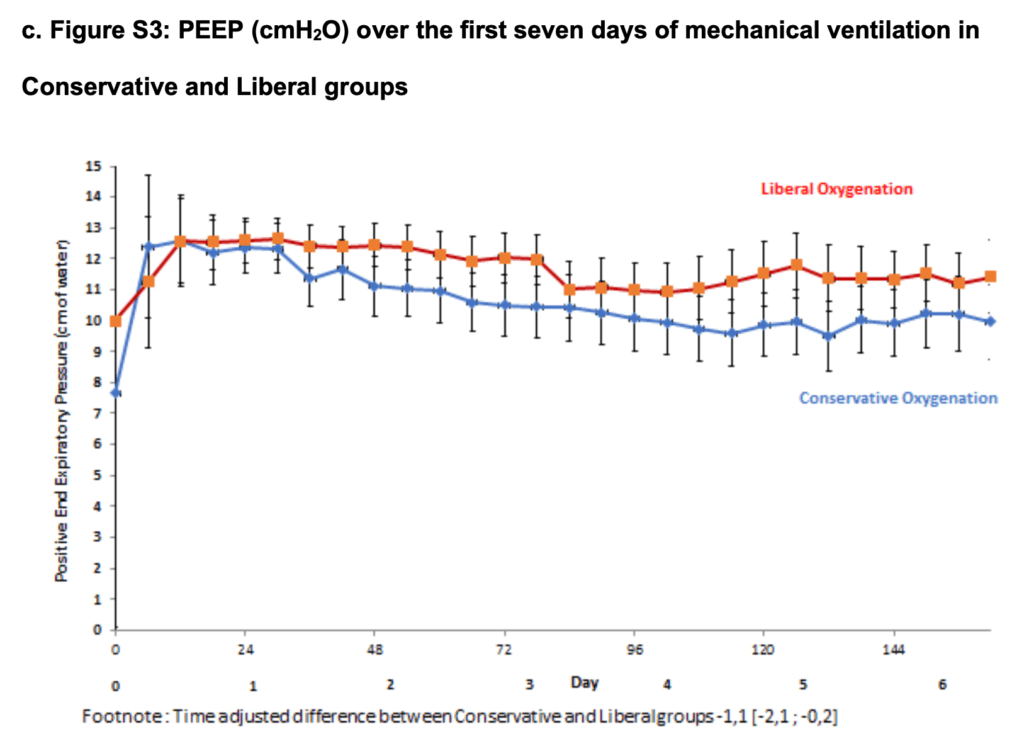
- Tidal volumes were not significantly higher, but PEEP was slightly lower in the conservative group compared to the liberal group.
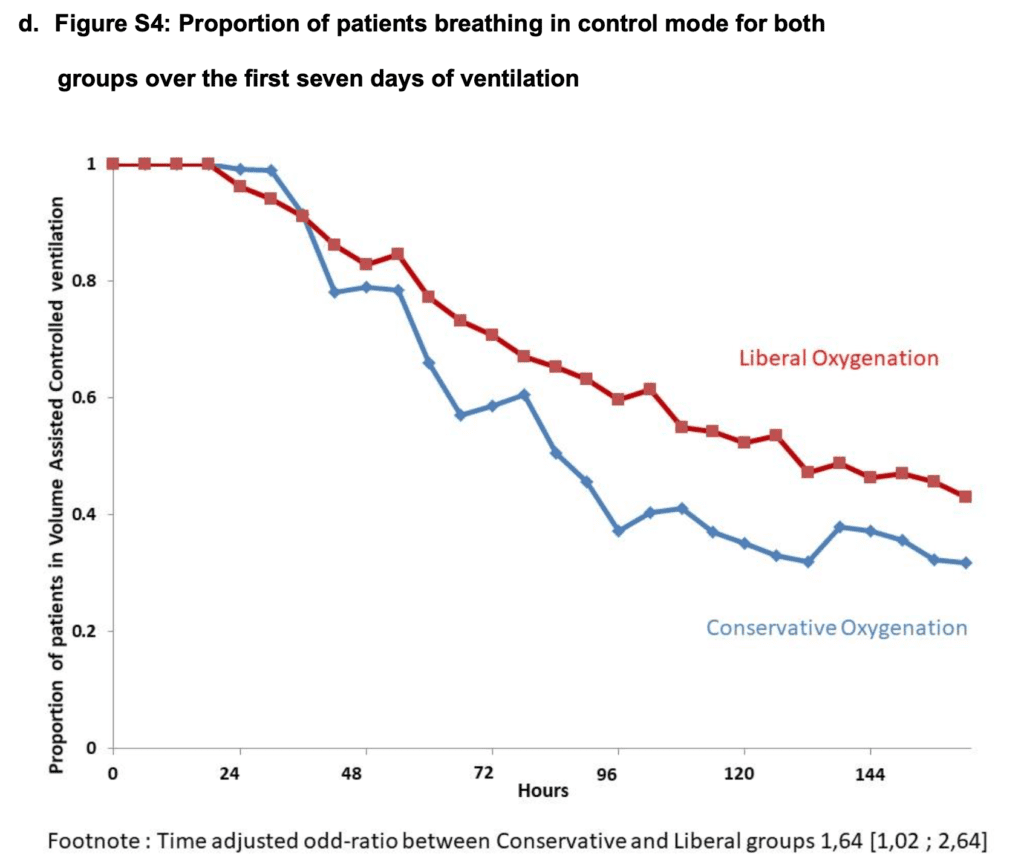
- Patients breathing in a volume assist control mode were higher in the liberal group vs conservative group.
- Heart rates in the conservative group were higher than the liberal group.
*it was determined that inclusion of 850 patients would provide a power of 90% to show an absolute between-group difference of 9 percentage points in the primary outcome. The trial was prematurely stopped. At that point only 205 patients had been enrolled in the study.
Strengths
- Prospective, multicenter, randomized trial. Can be externally validated
- Randomization (computer generated) done well. Stratified according to center by age, and severity of ARDS. ⅔ of the patients had moderate to severe ARDS .
- Baseline characteristics of both groups did not differ significantly
- Determined the percentage reduction in risk of death observed based on the CLOSE and Oxygen-ICU trials
-
No significant difference in ARDS severity between the groups
- 75.8% in the conservative group had Pao2:Fio2 of 150 mmHg or less
- 76.5% in the liberal group had Pao2:Fio2 of 150 mmHg or less
- Clear and similar protocols for ventilation management and oxygenation targets for both groups
- The trial was designed and overseen by a steering committee, and was funded by a grant from the French Ministry of Health. There was additional oversight by the University Hospital of Besancon. The funder had no influence on the trial design , collection or analysis of data, or the writing of the manuscript.
- No commercial support was provided for the trial.
- The trial was monitored by an independent data and safety monitoring board. They were informed of all serious adverse events. Data was provided by the safety monitoring team.
Limitations
- The biggest limitation is that the trial was prematurely halted by the data and safety monitoring board because of potential increased risk of serious adverse events and futility. They had only enrolled 205 patients, far from the intended 850 which would give them 90% power to show an absolute difference of 9 percentage points in the primary outcome.
- Non Blinded. Investigators were aware of the intervention. It was difficult to mask the results of the ABG and Sp02
- Conservative group had less proning and lower PEEP levels compared to the liberal oxygen group
- Pa02/Fi02 was used to set PEEP level (according to the 200mmHg threshold). In the weaning process the Pa02/Fi02 is dependent on the Fi02 which is measured and could have affected weaning in the conservative oxygen group
- In the conservative oxygen group targeting a Pa02 of 55mmHg could have exposed patients to lower levels of O2 as ABGs were drawn every 6 hours and it is unclear what the O2 levels were between these lab draws
- Non-invasive preventive ventilation immediately post extubation was largely recommended, whereas curative non-invasive ventilation was not. However, the details and protocols of what is considered curative vs. preventive is missing.
- Clinicians were more inclined to switch to an unassisted ventilation mode with low Fi02 levels, so patients in the conservative arm, most likely received unassisted ventilation whereas patients in the liberal arm received controlled mode ventilation
- The patients’ biologic profiles types were not studied. This might have affected their response to such strategies
Discussion
- A conservative oxygenation strategy during the first 7 days of mechanical ventilation did not reduce mortality at 28 days as expected.
- Only 205 patients were enrolled before the trial was prematurely stopped by the data and safety monitoring board because of safety concerns and a low likelihood of a significant difference.
- There were signs of increased mortality (although not established) at 90 days and mesenteric ischemia among those in the conservative group. This caused the trial to stop early.
-
The difference in oxygen exposures between the groups in this trial was larger than previous trials (OXYGEN-ICU and the CLOSE trials)
- In this trial the oxygen exposure in the liberal groups was closer to that in the control group of the other trials
- Oxygen exposure in conservative groups was close to the lower limits recommended in various ARDS trials and guidelines.
-
There was a clinically relevant excess mortality in the conservative group with mortality that was 14 percentage points higher than that in the liberal group at 90 days. These results could be explained by
- The respiratory severity (Pa02:Fi02 ratio) was higher in this trial than the OXYGEN-ICU and CLOSE trials
-
The trial intervention occurred in the first 12 hours and for 7 days (or until extubation if less than 7 days). Patients were likely exposed to hypoxemia. Using a lower range of Pa02 (55 to 70 mmHg) might have exposed patients to unsafe Pa02 levels. Keep in mind:
- There are reports of increased mortality with exposure to Pa02 levels less than 67 mmHg in a retrospective study from the Netherlands.
- The OXYGEN-ICU trial showed increased mortality with a Pa02 between 54 and 81 mmHg
- The ICU-ROX substudy involving patients with sepsis showed higher mortality in those exposed to conservative levels of oxygen.
- Targeting lower oxygen might decrease oxygen levels and transport. The heart rate was higher in the conservative group, there is a well known link to increased mortality in the ICUs
- The gut is sensitive to low oxygen delivery.
-
ABG samples in the conservative group:
- 58 patients (58.5%), a median of 2 arterial blood samples had a Pao2 (33.0 -54.8 mmHg) that was less than the threshold of 55.0 mmHg
- In 97 patients (97.8%), a median of 6 samples had a Pao2 (70.1 to 269.0 mmHg) that was greater than the threshold of 70.0 mmHg.
-
ABG samples in the liberal group
- 98 patients (96%) had blood gas Pao2 (40.8 to 89.9 mmHg) that was less than the threshold of 90 mmHg. (median of 8 samples)
- 98 patients had ABG with Pao2 (105.8 to 366.0 mmHg) that was greater than the threshold of 105.0 mmHg (median 7 samples)
-
There were a few differences and additional outcomes mentioned in the supplementary data that should be taken into consideration
- Over the 7 days of the intervention, prone positioning use was different in both groups. 34.3% in the conservative vs 51.0% in the liberal. The liberal group had 16.7 percentage points more in proning position, this is probably confounding the results and improving oxygenation in the liberal group.
- Renal replacement therapy was used more in the liberal group on days 1 and 3. (15% in the liberal vs 8.2% in the concervative on day one) and (14.9% in the liberal and 10.2% in the conservative on day 3). On day 6 there were 12% in the liberal and 13.7 in the conservative group who received RRT.
- Targeting Pa02 of 55 mmHg might have exposed patients to undetected lower arterial oxygen levels since it is difficult to maintain a lower limit of Pa02 continuously.
Author Conclusion
“Among patients with ARDS, early exposure to a conservative-oxygenation strategy with a Pao2 between 55 and 70 mm Hg did not increase survival at 28 days. A worrisome safety signal was observed in the group assigned to a lower oxygen exposure. The meaning of this signal to clinical practice is unclear”
Clinical Take Home Points
- In patients with acute respiratory distress syndrome (ARDS), conservative oxygen therapy may worsen mortality compared with liberal therapy possibly due to periods of time with lower, suboptimal oxygen saturations.
- Based on the Oxygen-ICU, ICU-ROX and LOCO2 trials, we can say that both hyperoxia (SpO2 >97%) and hypoxemia (SpO2 <90%) should be avoided. An SpO2 of 92% to 96% (PaO2 ~60s-90s) would be an ideal target.
References
- Barrot L, et al. Liberal or Conservative Oxygen Therapy for Acute Respiratory Distress Syndrome. NEJM 2020 PMID: 26334785
- Giradis M, et al. Oxygen-ICU. Effect of Conservative vs Conventional Oxygen Therapy on Mortality Among Patients in an ICU. JAMA 2016 PMID: 27706466
- Mackle D et al. Conservative Oxygen Therapy During Mechanical Ventilation in the ICU. NEJM 2019. PMID: 31613432
- Young PJ et al. Intensive Care Unit Randomised Trial Comparing Two Approaches to Oxygen Therapy (ICU-ROX): Results of the Pilot Phase. Crit Care Resus 2017. PMID: 29202261
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post The LOCO2 Trial: Liberal or Conservative Oxygen Therapy for Acute Respiratory Distress Syndrome appeared first on REBEL EM - Emergency Medicine Blog.
