
 Background: The mainstays for management of stroke include admission to a stroke center and management of modifiable risk factors.1,2,3 It is estimated that most strokes are ischemic (87%),4 and atrial fibrillation and/or flutter are thought to be responsible for approximately one third of all ischemic strokes.5 Patients with atrial fibrillation at highest risk for stroke are those with an elevated CHA2DS2-VASc (congestive heart failure, hypertension, age 75 years, diabetes, previous stroke or transient ischemic attach [TIA], vascular disease, age 65 to 74 years, sex category) score.6 Due to this increased risk of stroke in this population, it is important to identify atrial fibrillation so that they can be managed with guideline recommended oral anticoagulation to prevent recurrent strokes, although clinically, it is unclear what the minimum burden of atrial fibrillation is that requires anticoagulation.7
Background: The mainstays for management of stroke include admission to a stroke center and management of modifiable risk factors.1,2,3 It is estimated that most strokes are ischemic (87%),4 and atrial fibrillation and/or flutter are thought to be responsible for approximately one third of all ischemic strokes.5 Patients with atrial fibrillation at highest risk for stroke are those with an elevated CHA2DS2-VASc (congestive heart failure, hypertension, age 75 years, diabetes, previous stroke or transient ischemic attach [TIA], vascular disease, age 65 to 74 years, sex category) score.6 Due to this increased risk of stroke in this population, it is important to identify atrial fibrillation so that they can be managed with guideline recommended oral anticoagulation to prevent recurrent strokes, although clinically, it is unclear what the minimum burden of atrial fibrillation is that requires anticoagulation.7
In patients who have had a stroke without identification of atrial fibrillation on Holter or electrocardiographic monitoring, it is recommended that they undergo additional electrocardiographic monitoring for 2-4 weeks.8This is based on data suggesting that continuous monitoring may identify up to a quarter of patients who have had a prior stroke with atrial fibrillation.9 The available monitoring methods include external Holter and implantable loop recorder monitoring. There has not been a head-to-head comparison in detection rates of atrial fibrillation between these two methods, until now… Enter the STROKE-AF and PER DIEM trials.
Papers:
Effect of Long-term Continuous Cardiac Monitoring vs Usual Care on Detection of Atrial Fibrillation in Patients with Stroke Attributed to Large- or Small-Vessel Disease: The STROKE-AF Randomized Clinical Trial10
AND
Effect of Implantable vs Prolonged External Electrocardiographic Monitoring on Atrial Fibrillation Detection in Patients with Ischemic Stroke: The PER DIEM Randomized Clinical Trial11
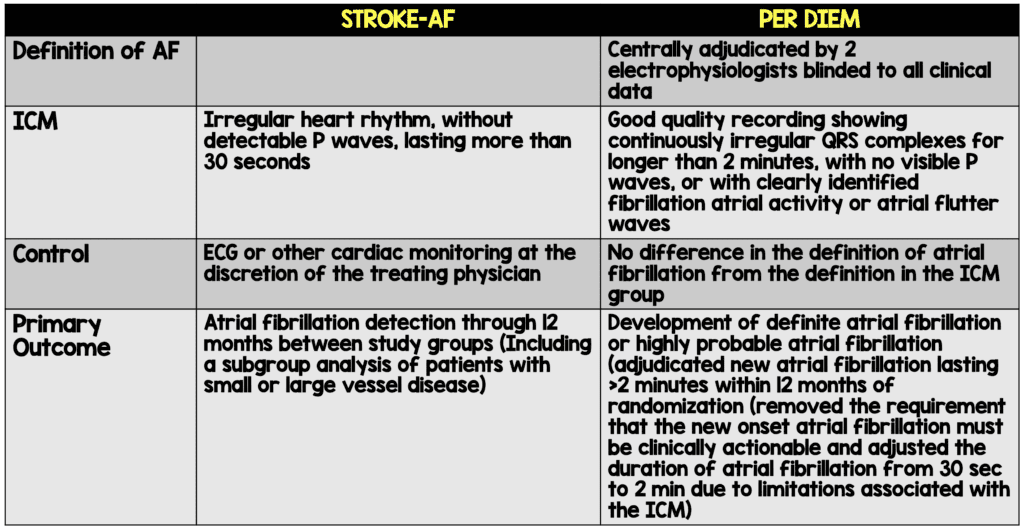
Clinical Question: What is the rate of atrial fibrillation (AF) detection in patients with an implantable cardiac monitoring (ICM) device compared to external cardiac monitoring in patients with a previous ischemic stroke (PER DIEM) or stroke due to large- or small-vessel disease (STROKE-AF)?
What They Did:
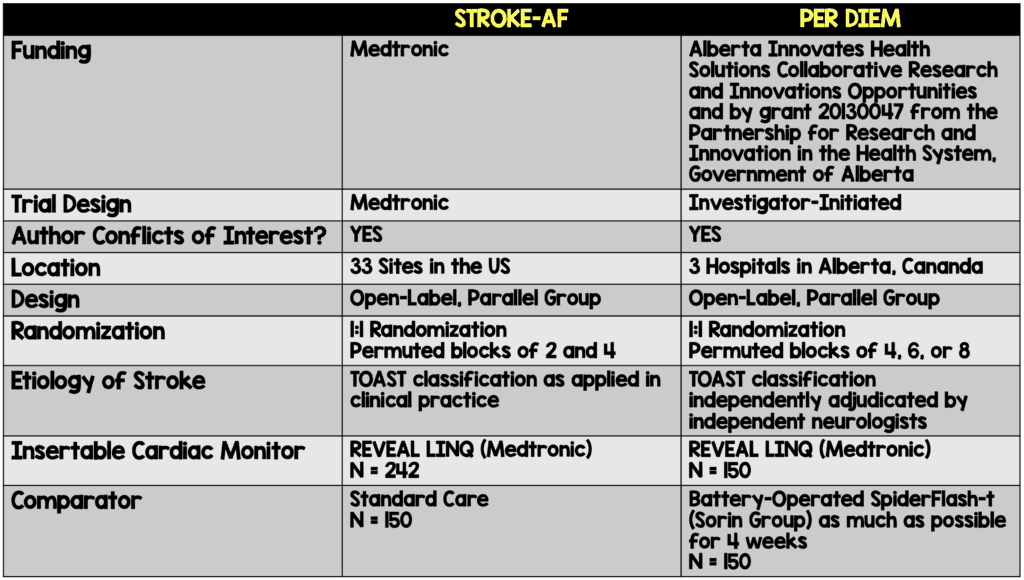
Stroke AF:
PER DIEM:
Outcomes:
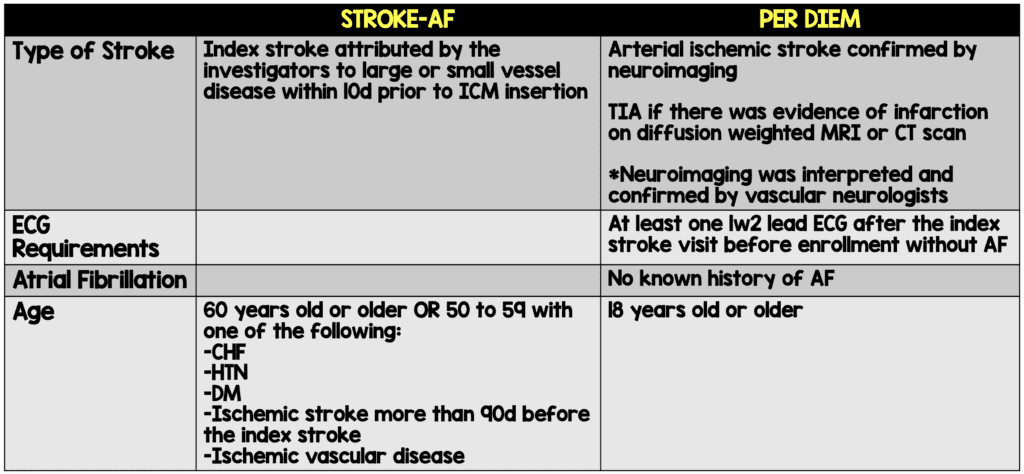
Inclusion:
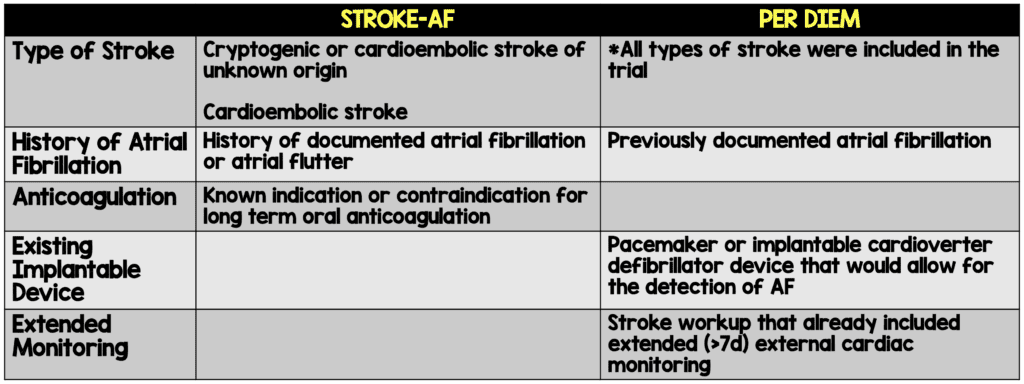
Exclusion:
Results:
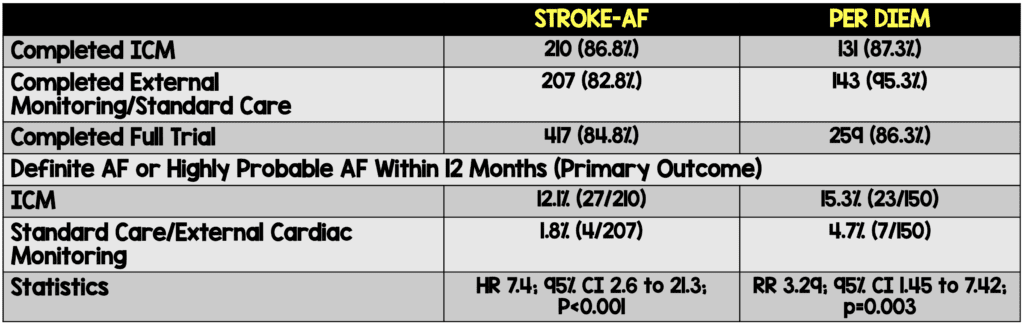
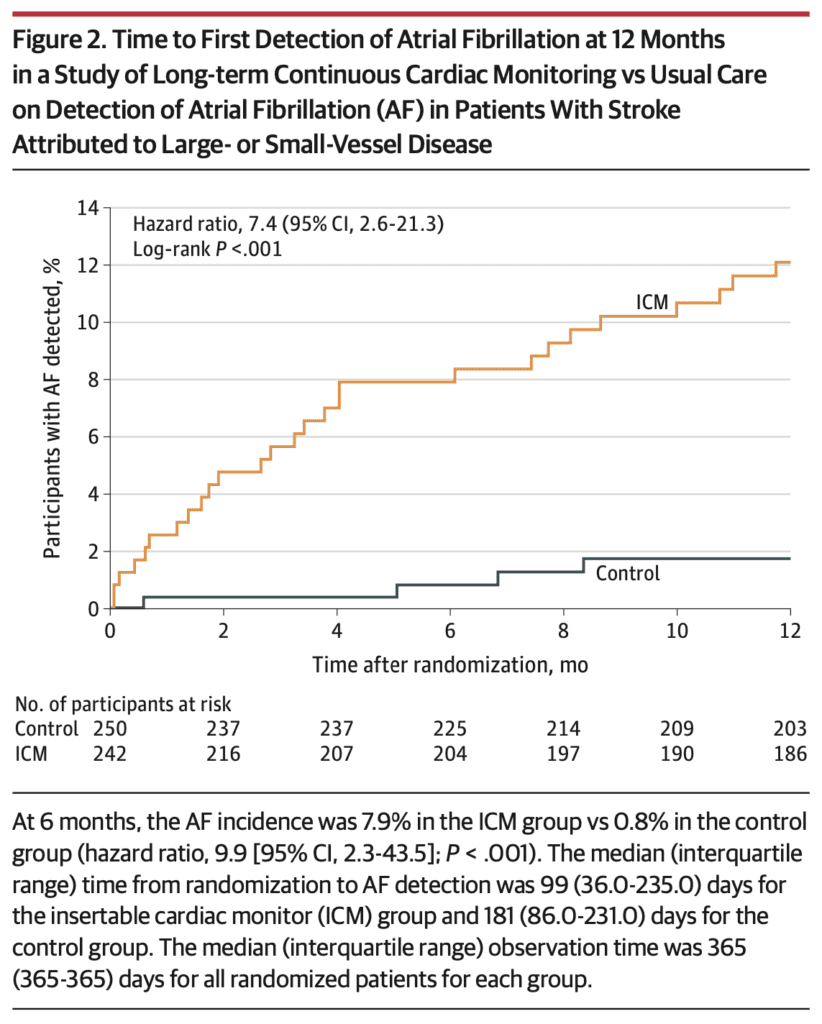
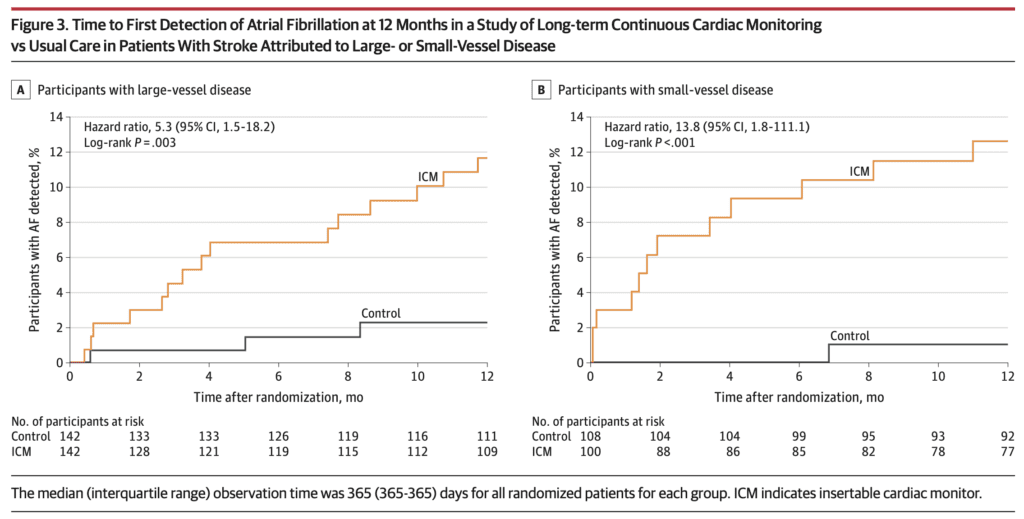
Stroke AF:
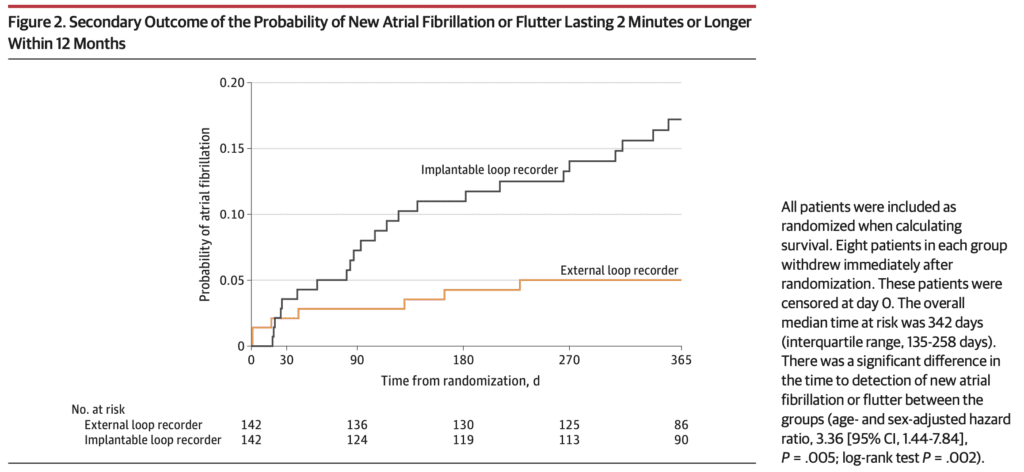
PER DIEM:
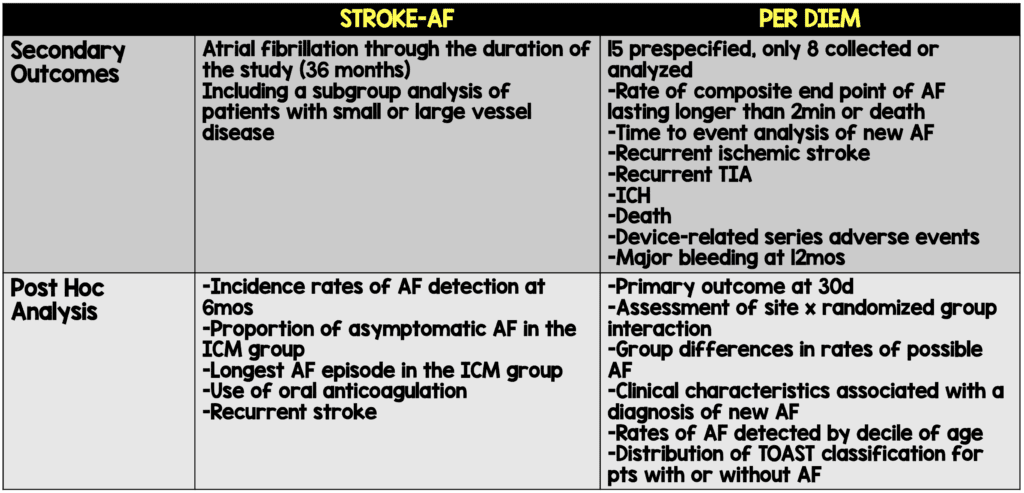
Secondary Outcomes
- STROKE AF
- PER DIEM:
Strengths:
STROKE-AF
- Prospective randomized control trial
- With PER DIEM, the first trial to directly compare internal cardiac monitoring to other forms of cardiac monitoring
- Enrollment after initial stroke event was very quick, a median of 4 (2-6) days with insertion of the cardiac monitoring device also being quick, a median of 5 (3-8) days
- Enrolled patients with a stroke thought to be due to small- or large-vessel occlusion, a group with sparse data on long-term cardiac monitoring. These strokes are generally thought to be due to atherosclerosis, not embolic phenomena.12
- Included data regarding serious adverse events associated with insertable cardiac monitoring. There were 4 in total (1.8%): 1 site infection, 2 insertion site hemorrhage, 1 site pain.
PER DIEM
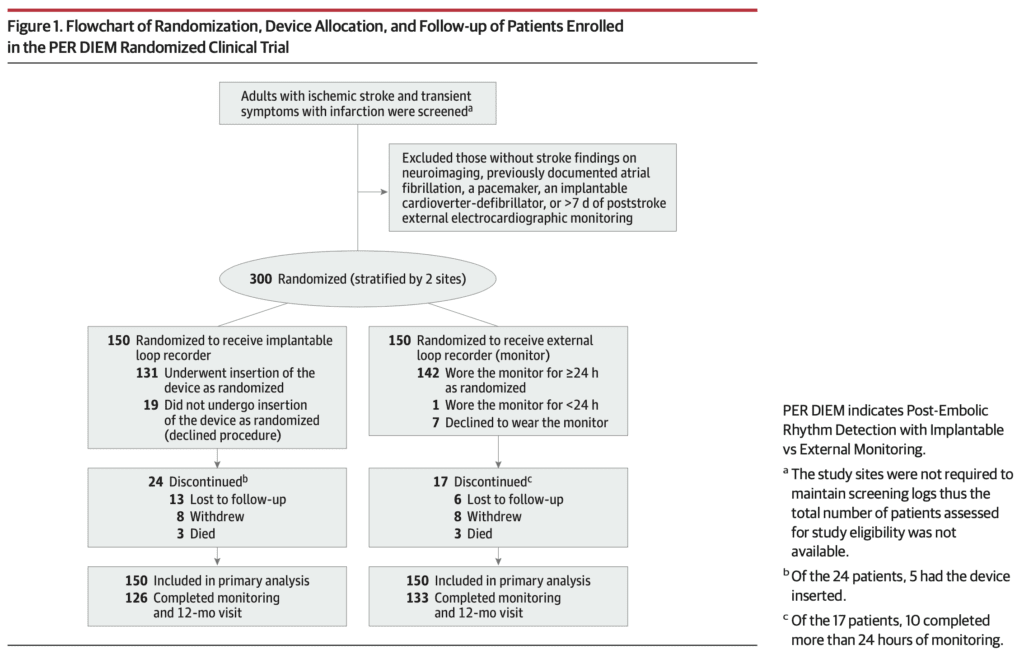
- Prospective randomized control trial
- With STROKE-AF, the first trial to directly compare internal cardiac monitoring to external cardiac monitoring for the detection of atrial fibrillation
- Investigator initiated and funded by the Province of Alberta
- Standardized control group of external cardiac monitoring (Holter monitoring)
- Per protocol analysis included in the data
- Included data regarding serious adverse events associated with insertable cardiac monitoring.
- Survey regarding the satisfaction with treatment group. 54/126 (42.9%) of patients in the ICM group were very satisfied with their care compared to 26/129 (20.2%) of patients in the control group.
Limitations:
STROKE-AF
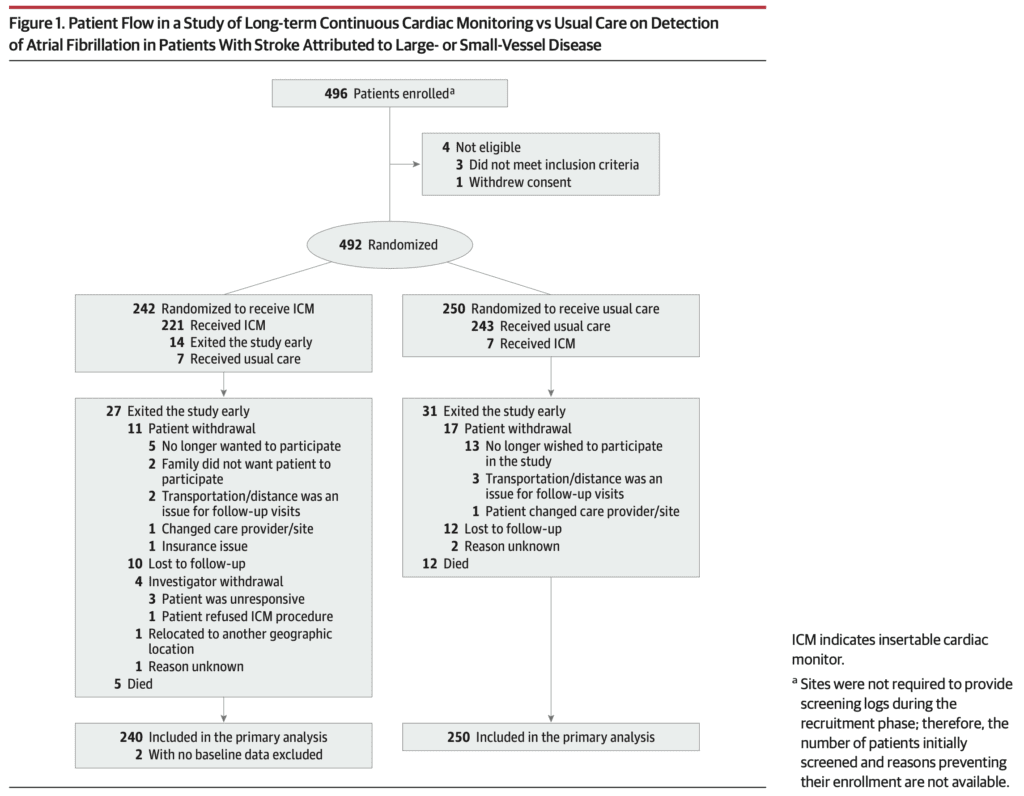
- Industry funded trial with multiple conflicts of interest in the author list. While this does not affect the methodology of the study (it appears sound), there is an inherent risk of bias when the device being compared is produced by the company providing the funding for the study.
- Investigator initiated enrollment, not consecutive enrollment. This method of patient enrollment is associated with selection bias.
- Excluded younger patients. Patients age 60 or older or 50-59 with one of the CHA2DS2-VASc risk factors were included in the study. The generalizability of this study is limited to this selected population.
- Lack of blinding. It is difficult to be blinded to which group a patient was enrolled into when the have a device that you can visualize in their chest and are receiving transmitted data from the same device electronically. Nonetheless, the lack of blinding based on the study design is associated with bias regarding the results.
- Lack of direct control group. While this helps to provide real world data regarding atrial fibrillation detection, it is difficult to determine the benefit of using an insertable cardiac monitor when compared to multiple other forms of detection. Some of the forms of detection in the study included, “76 electrocardiograms in 57 patients, 26 Holter monitors/event recorders in 25 patients, and 2 mobile cardiac telemetry devices in 2 patients.”
- Lack of standardization in determining the type of stroke. In this trial, it was subjective and could have led to over- or under-enrollment of the intended population.
- Limited generalizability to all patients with stroke and only to the subset with stroke thought to be due to small- or large-vessel occlusion.
- Statistical analysis, although seemingly appropriate, was performed by Medtronic. This introduces further bias as the company producing the device used in the study were also the proving mathematically that it is better than “standard of care.”
- Although the definition of atrial fibrillation was set to 30 seconds, the ICM is set to a limit of 2 minutes and would not detect atrial fibrillation of a shorter duration.
- Unclear clinical utility. This study does an excellent job of providing data that using a device that implanted into a patient and is constantly monitoring for atrial fibrillation leads to a high rate of detection of atrial fibrillation.
- It was not powered to detect the significance in the rate of recurrent stroke in each group. 16 patients in the ICM group (7.2%) and 23 patients (9.8%) in the control group had a recurrent stroke. There was no difference in the rate of TIA (1.8% vs 0.4%) or hemorrhagic stroke (1 in each group).
- It is unclear what duration of atrial fibrillation is clinically significant. The median duration was 88 (10-526) minutes in the ICM group, but if it is unclear if there is a difference in the rate of recurrent stroke, does it really matter clinically?
PER DIEM
- Conflicts of interest in the author list. Although this study was funded by the Provence of Alberta, the device was provided free of charge by Medtronic. Both factors insert bias into the results of this study.
- Delay of 2 months from stroke onset and study enrollment. There may have been undetected episodes of atrial fibrillation in this group, but if it never recurred for the duration of the study, it is unclear if it matters clinically.
- Definition of atrial fibrillation was set to 2 minutes, due to the limitations of the ICM. Again, it is unclear what duration is clinically relevant in providing anticoagulation to prevent recurrent stroke. While this definition seems long, it makes sense when comparing the ICM to the Holter monitor to use the same definition.
- Unclear clinical utility. This is the same as the STROKE-AF study. Just because there is a device that is constantly evaluating for the presence of atrial fibrillation, does it matter clinically if it is detected?
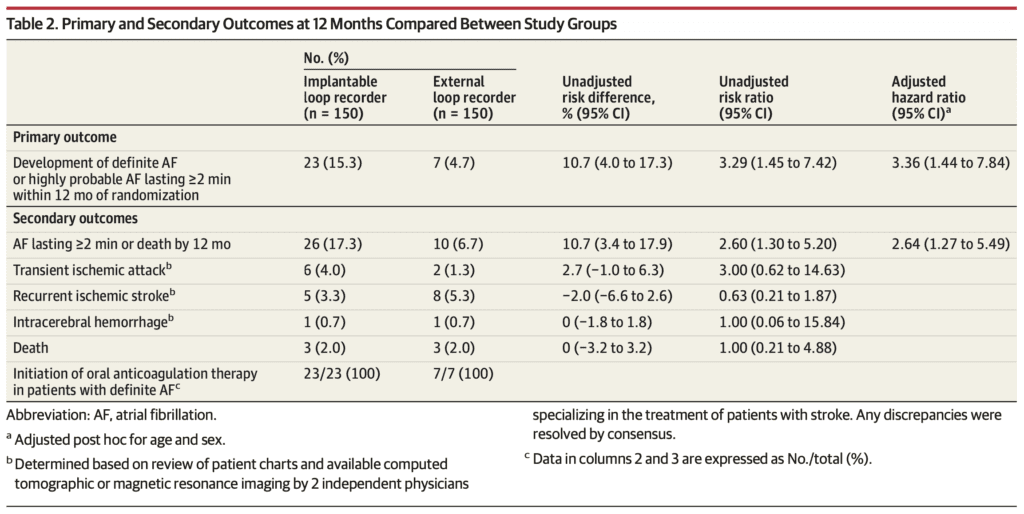
- Recurrent stroke was in the ICM group was 5 (3.3%) compared to 8 (5.3%). There was also no significant difference in rate of TIA (6 [4.0%] vs 2 [1.3%]), intracerebral hemorrhage (1 in each group), or death (3 in each group).
- The definition of recurrent stroke or TIA was based on a phone questionnaire. This may lead to under reporting of these events, but if it is the same in both groups, it should even out.
Authors Conclusion:
STROKE-AF:
“Among patients with stroke attributed to large- or small-vessel disease, monitoring with an ICM compared with usual care detected significantly more AF over 12 months. However, further research is needed to understand whether identifying AF in these patients is of clinical importance.”
PER DIEM:
“Among patients with ischemic stroke and no prior evidence of AF, implantable electrocardiographic monitoring for 12 months, compared with prolonged external monitoring for 30 days, resulted in a significantly greater proportion of patients with AF detected over 12 months. Further research is needed to compare clinical outcomes associated with these monitoring strategies and relative cost-effectiveness.”
Discussion:
An implanted device that is always on and created to detect atrial fibrillation lasting longer than 2-minutes leads to increased detection in atrial fibrillation when compared to other forms of detection of atrial fibrillation. It does seem that patients tend to be more satisfied with the implanted cardiac monitoring device when compared to a Holter monitor based on the PER DIEM trial, BUT in both trials, there was no difference in clinically meaningful outcomes such as stroke, TIA, intracranial hemorrhage, and death.
These trials do not address the clinical significance of the duration of atrial fibrillation. Is it 2 minutes, 30 minutes, or 2 weeks? We just don’t know and cannot answer that question based on this data. When performing a test, we must always think of the outcomes of that test and potential harms. Once atrial fibrillation is detected in a patient who has had a prior stroke, they will be started on oral anticoagulation. There are inherent risks associated with oral anticoagulation and they must be weighed against the benefits of this treatment. When the clinical significance of atrial fibrillation detection is unclear, so are the benefits of anticoagulation.
The results of these trials must also be interpreted in the context of significant bias. In both studies, there are significant author conflicts of interest. The STROKE-AF trial was not only funded by Medtronic (the manufacture of the REVEAL LINQ implanted cardiac monitoring device), but the statistics were performed by a statistician from Medtronic. There was selection bias based on convenient enrollment and not consecutive enrollment. When following up the patients, investigators were aware of the group the patient was assigned to and the results were not blinded. Finally, the control group was not standardized, making it unclear if there is a noninvasive form of monitoring that may be similar in the detection of atrial fibrillation.
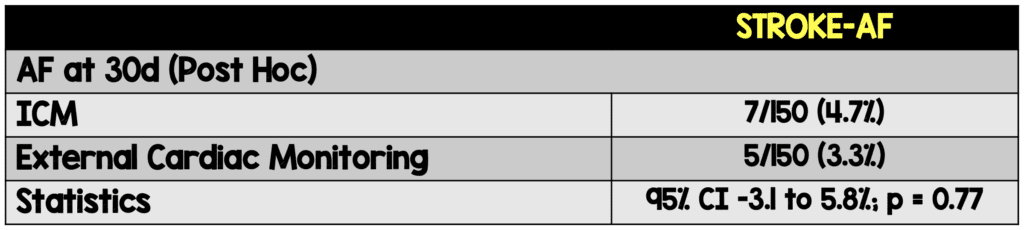
The PER DIEM Trial has a similar potential bias with author conflicts of interest. While the trial design was investigator initiated, the implanted cardiac monitoring device (REVEAL LINQ) was donated by Medtronic, which may also introduce bias into the results. The same lack of blinding was present in this study design as well. There was also a significant delay in enrollment from onset of stroke to implanted cardiac monitoring device insertion, but if there were instances of undiagnosed paroxysmal atrial fibrillation, the clinical significance of this delay is unclear. The control group in this trial was standardized to 30-days of Holter monitoring, and interestingly, there was no difference in the rate of diagnosis of atrial fibrillation between these groups at 30 days (4.7% in the ICM group vs 3.3% in the external cardiac monitoring group [95%CI, -3.1% to 5.8%]; P=0.77).
Clinical Take Home Point:
An implanated cardiac monitoring device designed to detect atrial fibrillation is able to diagnose atrial fibrillation at a higher rate when compared to standard of care (STROKE-AF) or 30 days of external cardiac monitoring (PER DIEM) at one year. I agree with the authors of both the STROKE-AF and PER DIEM trial, more research is needed to determine the clinical significance of long-term monitoring in the detection of atrial fibrillation using an implanted cardiac monitor when compared to standard of care.
Guest Post By:

Wilcox Medical Center
Kaua`i, HI
References:
- Gropen TI, Gagliano PJ, Blake CA, Sacco RL, Kwiatkowski T, Richmond NJ, Leifer D, Libman R, Azhar S, Daley MB; NYSDOH Stroke Center Designation Project Workgroup. Quality improvement in acute stroke: the New York State Stroke Center Designation Project. Neurology. 2006 Jul 11;67(1):88-93.PMID: 16832083.
- Kleinig TJ, Kimber TE, Thompson PD. Stroke prevention and stroke thrombolysis: quantifying the potential benefits of best practice therapies. Med J Aust. 2009 Jun 15;190(12):678-82. PMID: 19527202
- Xian Y, Holloway RG, Chan PS, Noyes K, Shah MN, Ting HH, Chappel AR, Peterson ED, Friedman B. Association between stroke center hospitalization for acute ischemic stroke and mortality. JAMA. 2011 Jan 26;305(4):373-80. PMID: 21266684; PMCID: PMC3290863.
- Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Shay CM, Spartano NL, Stokes A, Tirschwell DL, VanWagner LB, Tsao CW; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation. 2020 Mar 3;141(9):e139-e596. Epub 2020 Jan 29. PMID: 31992061.
- Freedman B, Potpara TS, Lip GY. Stroke prevention in atrial fibrillation. Lancet. 2016 Aug 20;388(10046):806-17. PMID:27560276.
- Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991 Aug;22(8):983-8. doi: 10.1161/01.str.22.8.983. PMID: 1866765.
- January CT, Wann LS, Calkins H, Chen LY, Cigarroa JE, Cleveland JC Jr, Ellinor PT, Ezekowitz MD, Field ME, Furie KL, Heidenreich PA, Murray KT, Shea JB, Tracy CM, Yancy CW. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2019 Jul 9;74(1):104-132. Epub 2019 Jan 28. Erratum in: J Am Coll Cardiol. 2019 Jul 30;74(4):599. PMID: 30703431.
- Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD, Fang MC, Fisher M, Furie KL, Heck DV, Johnston SC, Kasner SE, Kittner SJ, Mitchell PH, Rich MW, Richardson D, Schwamm LH, Wilson JA; American Heart Association Stroke Council, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on Peripheral Vascular Disease. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014 Jul;45(7):2160-236. Epub 2014 May 1. Erratum in: Stroke. 2015 Feb;46(2):e54. PMID: 24788967.
- Sposato LA, Cipriano LE, Saposnik G, Ruíz Vargas E, Riccio PM, Hachinski V. Diagnosis of atrial fibrillation after stroke and transient ischaemic attack: a systematic review and meta-analysis. Lancet Neurol. 2015 Apr;14(4):377-87. doi: 10.1016/S1474-4422(15)70027-X. Epub 2015 Mar 4. PMID: 25748102.
- Bernstein RA, Kamel H, Granger CB, Piccini JP, Sethi PP, Katz JM, Vives CA, Ziegler PD, Franco NC, Schwamm LH; STROKE-AF Investigators. Effect of Long-term Continuous Cardiac Monitoring vs Usual Care on Detection of Atrial Fibrillation in Patients With Stroke Attributed to Large- or Small-Vessel Disease: The STROKE-AF Randomized Clinical Trial. JAMA. 2021 Jun 1;325(21):2169-2177. PMID: 34061145; PMCID: PMC8170544 (available on 12/1/2021).
- Buck BH, Hill MD, Quinn FR, Butcher KS, Menon BK, Gulamhusein S, Siddiqui M, Coutts SB, Jeerakathil T, Smith EE, Khan K, Barber PA, Jickling G, Reyes L, Save S, Fairall P, Piquette L, Kamal N, Chew DS, Demchuk AM, Shuaib A, Exner DV. Effect of Implantable vs Prolonged External Electrocardiographic Monitoring on Atrial Fibrillation Detection in Patients With Ischemic Stroke: The PER DIEM Randomized Clinical Trial. JAMA. 2021 Jun 1;325(21):2160-2168. PMID: 34061146; PMCID: PMC8170545 (available on 12/1/2021).
- Fisher CM. Lacunar strokes and infarcts: a review. Neurology. 1982 Aug;32(8):871-6. PMID: 7048128.
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)
The post The STROKE-AF and PER DIEM Trials: Detection of Atrial Fibrillation After Stroke appeared first on REBEL EM - Emergency Medicine Blog.
