
 Background: First trimester vaginal bleeding is a common complaint seen in the emergency department. Patients are obviously stressed about the possibility of miscarriage while providers are stressed about missing diagnoses such as ectopic pregnancies. There have been multiple studies questioning the interrater reliability of the pelvic examination. A more important question however, is does the pelvic examination provide any benefit to these patients by enhancing management and decreasing morbidity?
Background: First trimester vaginal bleeding is a common complaint seen in the emergency department. Patients are obviously stressed about the possibility of miscarriage while providers are stressed about missing diagnoses such as ectopic pregnancies. There have been multiple studies questioning the interrater reliability of the pelvic examination. A more important question however, is does the pelvic examination provide any benefit to these patients by enhancing management and decreasing morbidity?
What They Did:
- Prospective, open-label, randomized, equivalence trial in pregnant patients presenting to the ED
- No pelvic exam vs pelvic exam only after an ultrasound confirmed IUP
Outcomes:
- Primary Composite Outcome at 30 days: Unscheduled return, subsequent admission, emergency procedure, transfusion, infection, and alternate source of symptoms)
- Secondary Outcome:
- ED throughput time
- Patient experience survey
Inclusion:
- ≥18 years of age
- English speaking
- Vaginal bleeding or lower abdominal pain
- Positive pregnancy test
- <16 week intrauterine pregnancy (IUP) by ultrasonography
Exclusion:
- Pelvic exam performed before consent and randomization
- Admission to the hospital
- Known history of cervical carcinoma
- Current pregnancy because of in vitro fertilization
- Suspicion for heterotopic pregnancy
- Reported heavy vaginal bleeding (soaking of > 10 menstrual pads in 24 hours)
- Hemodynamic instability (SBP < 90 mmHg or pulse rate > 110 beats/min)
- Report of or suspicion for penetrating vaginal trauma
- Intrauterine device in place
- Clinical suspicion for an alternative syndrome requiring pelvic examination (i.e. appendicitis, PID, or torsion)
- Reported sexual assault
- Prisoner
- Previous enrollment in the trial
- Inability to follow up by telephone
Results:
- 202 (of planned 720) patients enrolled
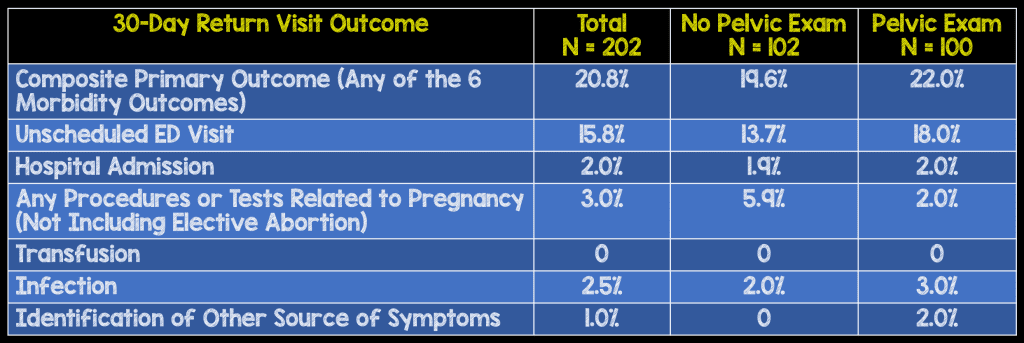
- The difference in primary composite outcome was driven by unscheduled return visits to the ED: 13.7% (no pelvic exam) vs 18.0% (pelvic exam)
- Patient reported feeling uncomfortable or very uncomfortable:
- No pelvic exam performed: 11.2%
- Pelvic exam performed: 23.7%
- 95% CI -23.0% – -2.0%
- No statistical differences in ED LOS or perceived thoroughness of care.
Strengths:
- Largest prospective randomized study looking at the utility of the pelvic exam in the ED
- First study with 30 day follow up outcomes
- Only lost 17 patients to follow up
Limitations:
- Convenience sample of patients, therefore potentially missing several patients with 1st trimester vaginal bleeding
- Ultrasonography performed by radiology or in the ED under the supervision of an ultrasonography credentialed EM physician (Neither of these may be an option at some facilities)
- This study did not have adequate sample size to reach statistical power (Required 720 participants and were only able to register 202)
- Only patients with ultrasound confirmed IUP were enrolled in this study (i.e. Patients with indeterminate US results or clearly identified ectopic pregnancies were excluded)
- Obviously, not possible to blind patients, providers, or research assistants to pelvic exam vs no pelvic exam
- Used a composite primary endpoint instead of individual morbidity endpoints
Discussion:
- Interesting point brought up in the paper. Of the 178 women who refused enrollment into the study, 74 (42%) did so because they did not want a pelvic exam, whereas only 4 (2%) refused because they wanted a pelvic exam
- In many facilities, a pelvic exam is performed before ordering a pelvic ultrasound. The pelvic exam can aid in finding alternative diagnoses of bleeding other than miscarriage and ectopic pregnancy (i.e. cervical carcinoma, vaginal lacerations, etc…).
Author Conclusion: “Although there was only a small difference between the percentage of patients experiencing the composite morbidity endpoint in the 2 study groups (2.4%), the resulting 90% CI was too wide to conclude equivalence. This may have been due to insufficient power. Patients assigned to the pelvic examination group reported feeling uncomfortable more frequently.”
Clinical Take Home Point: Although the evidence is starting to mount against the usefulness of the pelvic exam in the ED, this study was not powered to detect a difference in performing vs not performing a pelvic exam on morbidity outcomes. This paper should not change your practice of performing a pelvic exam in 1st trimester vaginal bleeding, as alternative diagnoses may be missed.
References:
- Linden JA et al. Is the Pelvic Examination Still Crucial in Patients Presenting to the Emergency Department With Vaginal Bleeding or Abdominal Pain When an Intrauterine Pregnancy is Identified on Ultrasonography? A Randomized Controlled Trial. Ann Emerg Med 2017. PMID: 28935285
For More Thoughts on This Topic Checkout:
- Ryan Radecki at EM Literature of Note: The End of the “Emergency” Pelvic Exam
- Salim Rezaie at ALiEM: Is the Pelvic Exam in the Emergency Department Useful?
Post Peer Reviewed By: Anand Swaminathan (Twitter: @EMSwami)
The post Usefulness of the Pelvic Examination in 1st Trimester Vaginal Bleeding appeared first on REBEL EM - Emergency Medicine Blog.
