 Background: Many providers and health care workers place oxygen on patients as a way to overcome hypoxemia or for patient comfort. Also in STEMI patients, many of us have learned the mnemonic “MONA” to remember the treatments for acute coronary syndrome. MONA stands for morphine, oxygen, nitroglycerin, and aspirin. It is however important to remember that oxygen is a drug; just like any other drug, there are side effects. Some of the best known side effects of hyperoxia are direct lung toxicity, peripheral vasoconstriction, and increase in production of reactive oxygen species. The PROXI Trial (Perioperative Oxygen Fraction-Effect on Surgical Site Infection and Pulmonary Complications After Abdominal Surgery) and the AVOID Trial (Air Versus Oxygen in Myocardial Infarction) showed increased long-term mortality and larger myocardial infarction size respectively in patients with supra-normal oxygen levels (hyperoxia). In this episode we will explore the effect of higher oxygen levels through in ICU and STEMI patients by reviewing two trials:
Background: Many providers and health care workers place oxygen on patients as a way to overcome hypoxemia or for patient comfort. Also in STEMI patients, many of us have learned the mnemonic “MONA” to remember the treatments for acute coronary syndrome. MONA stands for morphine, oxygen, nitroglycerin, and aspirin. It is however important to remember that oxygen is a drug; just like any other drug, there are side effects. Some of the best known side effects of hyperoxia are direct lung toxicity, peripheral vasoconstriction, and increase in production of reactive oxygen species. The PROXI Trial (Perioperative Oxygen Fraction-Effect on Surgical Site Infection and Pulmonary Complications After Abdominal Surgery) and the AVOID Trial (Air Versus Oxygen in Myocardial Infarction) showed increased long-term mortality and larger myocardial infarction size respectively in patients with supra-normal oxygen levels (hyperoxia). In this episode we will explore the effect of higher oxygen levels through in ICU and STEMI patients by reviewing two trials:
The Oxygen ICU Trial
The SOCCER Trial
February 2017 REBEL Cast: The All Hyperoxia Edition
Click here for Direct Download of Podcast
The OXYGEN ICU Trial
Girardis M et al. Effect of Conservative vs Conventional Oxygen Therapy on Mortality Among Patients in an Intensive Care Unit: The Oxygen-ICU Randomized Clinical Trial. JAMA 2016; 316(15): 1583 – 1589. PMID: 27706466
What They Did:
- Single-center, open-label, parallel-group, randomized clinical trial of all adults admitted to the intensive care unit with an expected length of stay of ≥72 hours
- Comparison of conservative oxygen therapy (PaO2 between 70 – 100mmhg or SpO2 between 94 – 98%) versus standard conventional ICU practice (PaO2 up to 150mmHg or SpO2 between 97 – 100%)
Outcomes:
- Primary: ICU Mortality
- Secondary: New Organ Failure and Infection ≥48hours after ICU admission or need for re-operation in surgical patients.
Inclusion:
- Age ≥18 years
- Expected length of stay of ≥72 hours
Exclusion:
- Age <18 years
- Pregnancy
- ICU readmission
- Decision to withhold life-sustaining treatment
- Immunosuppression
- Neutropenia
- Enrollment in Another Study
- Acute Decompensation of Chronic Obstructive Pulmonary Disease
- Acute Respiratory Distress Syndrome with a PaO2:FiO2 ratio < 150
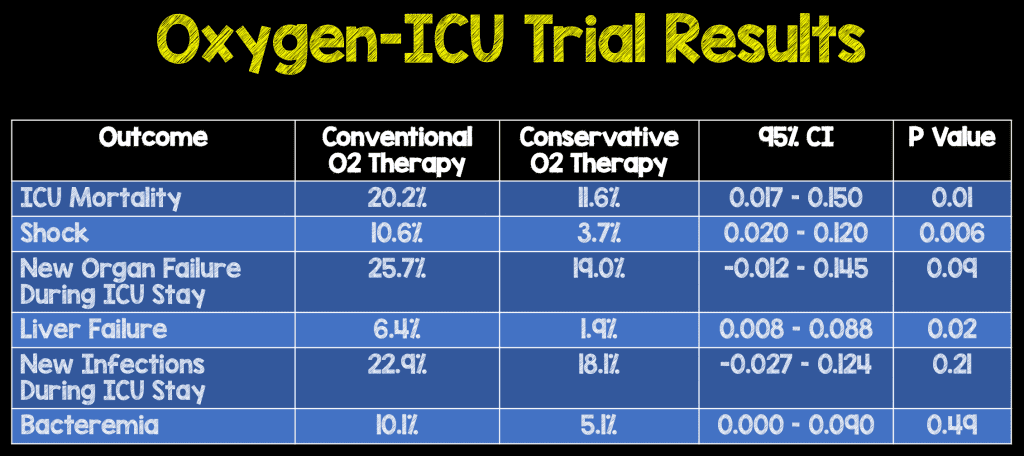
Results:
- 434 patients included in the modified intention to treat analysis
- Conventional Oxygen Therapy = 218 patients
- Conservative Oxygen Therapy = 216 patients
Strengths:
- Clinically important question with patient oriented outcomes
- Randomized patients by a computerized random-number generator in a 1:1 ratio
- There was a difference in PaO2 between the conservative and conventional groups
Limitations:
- A sample size of 660 patients was needed to detect an absolute difference in mortality of 6% (Recruitment stopped at 480 patients due to an earthquake)
- Single-center study
- Unable to give a detailed analysis of effects of hyperoxia in different population subsets (i.e. stroke, traumatic brain injury, acute myocardial infarction)
- Patients in the conventionally treated group had a trend toward higher illness severity at baseline (This would make results potentially more favorable for the conservative oxygen group)
- Daily time weighted PaO2 may only approximate true exposure to hyperoxia in patients where only 1 – 2 blood gas analyses performed daily
- Incidence of new infection may have been underestimated due to confirmed microbiological samples as the sole consideration of infection
Discussion:
First randomized clinical trial to evaluate the effect of a conservative oxygen therapy on mortality vs standard, more liberal strategies
Author Conclusion:
“Among critically ill patients with an ICU length of stay of 72 hours or longer, a conservative protocol for oxygen therapy vs conventional therapy resulted in lower ICU mortality. These preliminary findings were based on unplanned early termination of the trial, and a larger multicenter trial is needed to evaluate the potential benefit of this approach.”
Clinical Take Home Point: In critically ill ICU patients, FiO2 should be titrated to maintain normoxia as supraphysiologic levels appear to increase mortality.
The SOCCER Trial
Khoshnood A et al. Effect of Oxygen Therapy on Myocardial Salvage in ST Elevation Myocardial Infarction: The Randomized SOCCER Trial. Eur J Emerg Med 2016; [Epub Ahead of Print] PMID: 27893526
What They Did:
- Randomized controlled trial at 2 hospitals in Sweden
- Normoxic STEMI patients were randomized prehospital to either supplemental O2 (10L/min) or room air until PCI completed
- Cardiac MRI (CMR) was performed 2 – 6 days after inclusion into the trial
Outcomes:
- Primary: Myocardial salvage index assessed by CMR
- Secondary: Infarct Size and Myocardium at Risk
Inclusion:
- STEMI
- Symptom duration <6h
- Normal O2 Saturation (Defined as ≥94%)
- Accepted for Acute PCI
Exclusion:
- Previous Acute myocardial infarction
- Patient inability to make decision to participate (i.e. dementia)
- Severe claustrophobia
- Implanted magnetic material
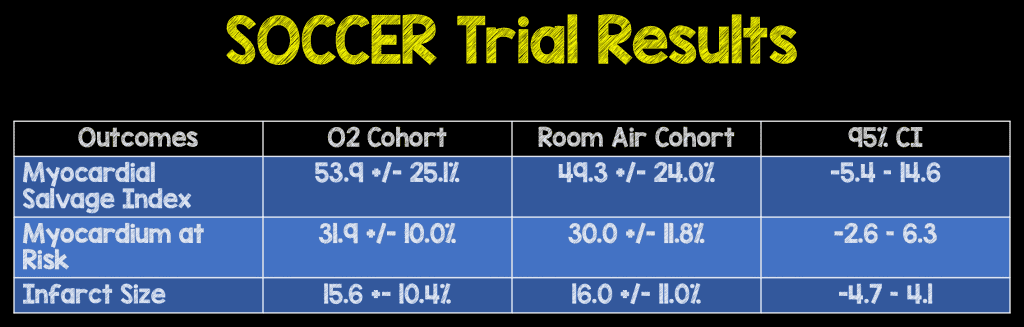
Results:
- 95 patients included in the study
- O2 Cohort = 46 patients
- Room Air Cohort = 49 patients
Strengths:
- Randomized controlled trial
- Randomized 1:1 to administration of either standard O2 therapy (10L/min) vs no Supplemental O2
- Patients in both groups received standard care in the ambulance
- Researchers blinded to group allocation
Limitations:
- Didn’t reach the 100 patients necessary for the assumption of myocardial salvage index of 60 +/- 20% in the O2 group, therefore making this an underpowered study.
- There was a trend toward more diabetes mellitus and hypertension in the room air group
- Not a patient oriented outcome as primary result, but a imaging oriented outcome (i.e. Cardiac MRI)
- Study uses surrogate outcomes to draw conclusions, and is not powered to detect differences in clinical events
- Patients only received supplemental O2 for an average of 86 minutes. It is possible that longer times may yield different results
- Ambulance and PCI lab personnel were aware of the patient’s group allocation potentially affecting patient treatment
Author Conclusion: “In STEMI patients undergoing acute PCI, we found no effect of high-flow oxygen compared with room air on the size of ischemia before PCI, myocardial salvage, or the resulting infarct size. The results support the safety of withholding supplemental oxygen in normoxic STEMI patients.”
Clinical Take Home Point: This was a small trial, which was underpowered, and used surrogate endpoints, therefore making the results inconclusive. At this time, more research is needed before changing practice to withholding oxygen therapy in normoxic STEMI patients.
References:
- Girardis M et al. Effect of Conservative vs Conventional Oxygen Therapy on Mortality Among Patients in an Intensive Care Unit: The Oxygen-ICU Randomized Clinical Trial. JAMA 2016; 316(15): 1583 – 1589. PMID: 27706466
- Khoshnood A et al. Effect of Oxygen Therapy on Myocardial Salvage in ST Elevation Myocardial Infarction: The Randomized SOCCER Trial. Eur J Emerg Med 2016; [Epub Ahead of Print] PMID: 27893526
For More Thoughts on These Topics Checkout:
- Josh Farkas at PulmCrit (EMCrit): Oxygen-ICU Trial – 100% Isn’t an A+
- David Slessor at The Bottom Line: Normal Oxygenation Versus Hyperoxia in the Intensive Care Unit (ICU) (OXYGEN-ICU)
- ScanCrit: The Oxygen-ICU Trial
- Michael Turchiano at CORE EM: Effect of Conservative vs. Conventional Oxygen Therapy on ICU Mortality
- WIKI Journal Club: OXYGEN-ICU
The post February 2017 REBEL Cast: The All Hyperoxia Edition appeared first on REBEL EM - Emergency Medicine Blog.