
 In terms of airway management, cricothyrotomy is one of the most advanced airway procedures an ED physician will perform. It is a last resort procedure when a patient is not able to be ventilated/oxygenated and/or intubated. Typically, this procedure requires the identification of certain landmarks such as the cricothyroid membrane, but what if you can’t identify any landmarks? What do you do? We got Rob Bryant on the show to discuss some aspects of a recent nightmare airway case he had.
In terms of airway management, cricothyrotomy is one of the most advanced airway procedures an ED physician will perform. It is a last resort procedure when a patient is not able to be ventilated/oxygenated and/or intubated. Typically, this procedure requires the identification of certain landmarks such as the cricothyroid membrane, but what if you can’t identify any landmarks? What do you do? We got Rob Bryant on the show to discuss some aspects of a recent nightmare airway case he had.
REBEL Cast Episode 52 – A Nightmare Airway with Rob Bryant
Click here for Direct Download of Podcast
Front Of Neck Access (FONA) with a Twist
The patient involved in this case has given permission to share the story, and relevant images with the knowledge that this information will be used for the purposes of education.
Rob’s Case: I was finishing a day shift at a small community hospital (we typically do not see any new patients after the arrival of the 2pm physician). At 2:30 one of the nurses radioed for a provider to come to room 25. This can either mean something interesting and exciting is happening, there is also the chance of getting sucked into an unenjoyable time vortex.
The patient was in his 50’s, sitting bolt upright, with impressive increased work of breathing. He had room air sats of 86% and an impressive goiter, and his wife explained that he had a breathing tube placed 1 week ago for similar breathing difficulties. He was phonating normally, but seemed to be getting simultaneously more distressed, and more fatigued.
While the patient was being moved to a critical care room I confirmed his history on the EMR. (Intubated with difficulty 5 days earlier for an H. flu tracheitis). I was called back to the room because the patient had become unresponsive.
The patients sats were in the 60’s, he would intermittently resist attempts at IV placement. The initial airway plan was to perform a Ketamine assisted awake intubation. The patient received 100mg of IV Ketamine, and BVM breaths were delivered with difficulty. Due to the difficulties we were having pre-oxygenating him, we proceeded with a dose of Rocuronium (100mg), he was then easier to bag, and pre-intubation sats were 99%.
The team now consisted of myself, my colleague, 2 nurses, a respiratory therapist, 2 critical care techs, and the nursing house supervisor. The plan was to look with VL, and attempt the passage of a small ET tube over a pocket bougie. The vocal cords were easily visualized, and all upper laryngeal structures appeared normal. There was obvious swelling to the trachea below the cords.
Multiple attempts with multiple combinations of bougies, ET tubes on regular, and gliderite stylets, and ‘straight bougie’ approach with DL were performed. We were unable to get anything to pass down the trachea. With an estimated duration of attempts of 3 minutes, the patient did not desaturate. An Air-Q LMA was placed, the patient was able to be ventilated with difficulty, with a lot of bubbling coming out of the mouth. (This was felt to be due to the high tracheal resistance from the tracheal stenosis). Sats were holding in the low 90’s, and a reliable ETCO2 tracing was obtained. The patient was felt to not be stable enough for the 15 min HEMS transfer across town.
[embedyt] http://www.youtube.com/watch?v=LTN6ATZW6fU[/embedyt]
There was no ENT available, anesthesia was called by the nursing supervisor as we started the surgical airway:
In this facility, anesthesia doesn’t consider surgical airways to be part of their skillset. The initial response from the anesthesiologist who was caught off guard on an otherwise very busy day for them was “I don’t do those”. They did respond to the resuscitation, where the surgical airway was underway. They later confirmed that a surgical airway is a procedure that they feel they are not trained in, and do not feel comfortable performing.
The patient had sats in the low 90’s at the start of the procedure. The anterior neck was infiltrated with 1% lidocaine with epi. The patient received an additional 100mg of Ketamine.
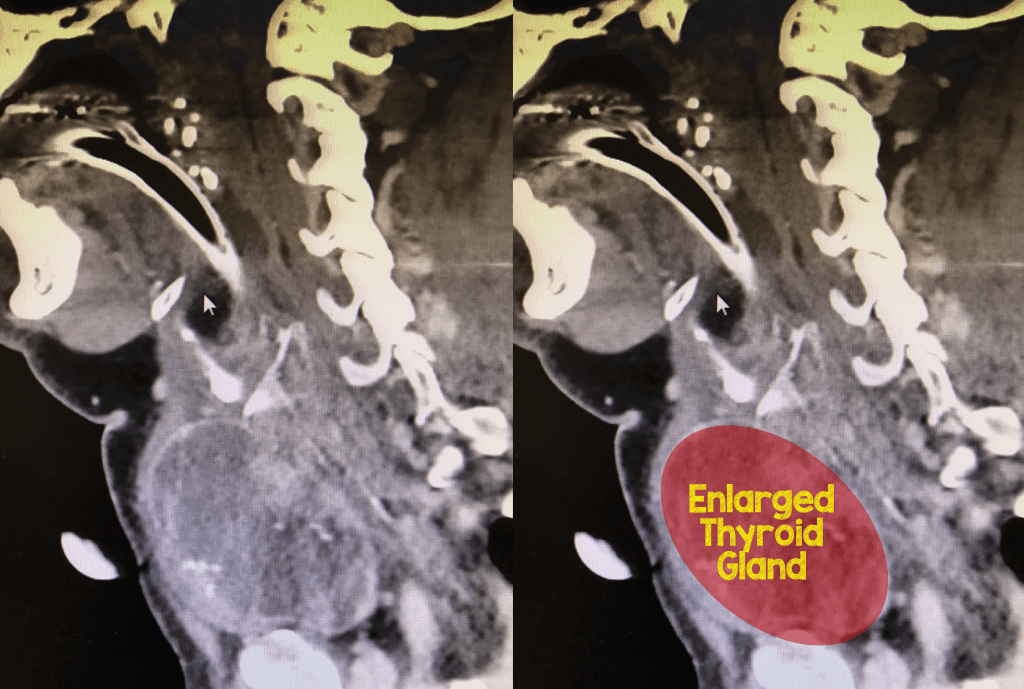
Laryngeal structures were very difficult to palpate. The hyoid and upper thyroid cartilage was palpable. The cricoid, and cricothyroid membrane were not palpable due to the overlying large thyroid isthmus. (see image from CT scan of the neck from previous week). A deliberately high vertical incision was made by my colleague to allow identification of the thyroid cartilage, and to avoid the thyroid mass.
The hyothyroid membrane, and thyroid cartilage was palpable through the incision. Neither I, nor my colleague could definitively identify or palpate the cricothyroid membrane. We could both feel the lower border of the thyroid cartilage, however with a finger on the lower edge of the thyroid cartilage we were touching the thyroid isthmus. Knowing the approximate location of the cricothyroid membrane, a percutaneous cricothyrotomy kit was used by my colleague. Air was able to be aspirated into the saline containing syringe attached to the needle. The guide wire was advanced with a little difficulty. A careful incision was made adjacent to the guidewire. The guidewire was fed into the combination dilator / tracheostomy and this was advanced through the cricothyroid membrane. Lack of familiarity with the kit caused the dilator to briefly slide out of the tracheostomy on the first attempt.
The patient was easily bagged through the tracheostomy with a normal ETCO2 waveform. The wound was soaked in TXA, and a single suture was placed through the incision. A cervical collar was placed over the tracheostomy to provide some stabilization. The patient was transferred to the receiving facility, a tracheostomy and removal of thyroid isthmus was performed the following day. The patient had no recollection of any portion of the procedure.
REBEL Cast Guest

Rob Bryant, MD
Emergency Medicine
Utah Emergency Physicians, Intermountain Medical Center
Salt Lake City, UT
Twitter: @RobJBryant13
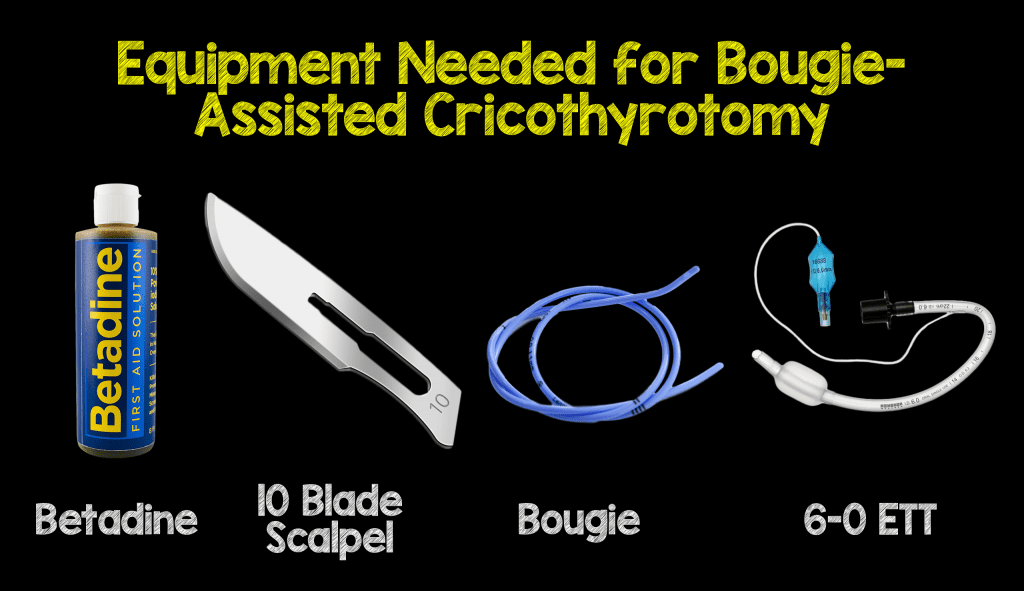
Equipment Needed for Bougie-Assisted Cricothyrotomy
Why Did Such a Stressful Case Go Well:
- A Quiet room: Everyone was engaged, calm, and responsive to requests for additional airway gear, and medications
- Well Trained Ancillary Staff:The critical care techs knew how to find everything. The nurses knew how to prepare medications swiftly and demonstrated excellent closed loop communication of med dosing. Skilled respiratory therapists
- Acknowledgement of Team Suggestions by Team Leader (ie: should we call the OR to see if there is an ENT there)
- Previous Annual In-Situ Simulation Training: The team had performed previous annual in situ simulation training for the preceding 2 years (no scenarios had involved a surgical airway) with a focus on a quiet room and closed loop communication.
- Practice/Previous Experience Helps: One of the operators had performed 2 previous surgical airways and the other operator had seen, and practiced with the percutaneous cric kit.
- Crisis/Social Worker: A crisis/social worker was on hand to help manage the patient’s spouse
Clinical Learning Points:
- Preparing for rare scenario’s pays off (Interdisciplinary team training and simulation training)
- There is a role for percutaneous front of neck access
- Practice excellent closed-loop communicationwith every sedation, and easy intubation so that it doesn’t seem forced / awkward when you need it
- You (the ED provider) may be the most experienced front of neck accessor in the room, even if you are joined by anesthesia. Some anesthesia providers (like some ED providers) have never performed a surgical airway, and do not consider it to be part of their skillset. When co-managing an airway with anesthesia this may present a significant cognitive hurdle when making the (appropriate, and timely) decision to proceed to a surgical airway.
For More on Airway Anatomy/Skills & Human Factors be Sure to Follow The Following Individuals on Twitter:
Airway
- Scott Weingart: @emcrit
- Richard Levitan: @airwaycam
- James Ducanto: @jducanto
Human Factors
- Chris Hicks: @humanfact0rz
- Victoria Brazil: @SocraticEM
- Cliff Reid: @cliffreid
- Jason Brooks: @phenomenaldocs
For More on This Topic Checkout:
- EMCrit: Mind Blowing Cricothyrotomy Video
- EM Ireland: Cricothyroidotomy
- EMCrit: Awake Intubation Lecture from SMACC
- EMCrit: Bougie-Aided Cricothyrotomy by Darren Braude
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)
The post REBEL Cast Ep 52: A Nightmare Airway with Rob Bryant appeared first on REBEL EM - Emergency Medicine Blog.
