
 So I was recently invited to the Texas College of Emergency Physicians meeting in Austin, TX (April 23rd – 26th, 2015) and was asked to give a lecture on sepsis, titled “Optimizing ED Management of Sepsis.” I was able to record my audio from that lecture and will summarize it on this blogpost and attach the audio to the lecture as well. Now usually on REBELCast I do a mini-critical appraisal of recent literature with Swami and Matt, but in this episode I am going to try and give you a succinct summary of the recent sepsis trials that have been released over the past 6 – 12 months.
So I was recently invited to the Texas College of Emergency Physicians meeting in Austin, TX (April 23rd – 26th, 2015) and was asked to give a lecture on sepsis, titled “Optimizing ED Management of Sepsis.” I was able to record my audio from that lecture and will summarize it on this blogpost and attach the audio to the lecture as well. Now usually on REBELCast I do a mini-critical appraisal of recent literature with Swami and Matt, but in this episode I am going to try and give you a succinct summary of the recent sepsis trials that have been released over the past 6 – 12 months.
REBEL Cast Episode 9: Sepsis Care in 2015
Click here for Direct Download of Podcast
I have uploaded the slides to this presentation on SlideShare where you can download them for FREE!!!
What Mean Arterial Pressure (MAP) should we target in sepsis?
- Surviving Sepsis Campaign recommends MAP≥65mmHg (Level 1C)
- Ledoux D et al [1]: 10 patients with septic shock –> Increased pressors to MAP of 65, 75, and 85 mmHg –> Increasing the MAP from 65 mm Hg to 85 mm Hg with norepinephrine increased CO, but no diff in lactate or UOP
- Bourgoin A et al [2]: 28 patients with septic shock –> Increased pressors to MAP of 65 to 85 mmHg –> Increased CO, but no difference renal function or UOP
-
Dunser et al [3]: Retrospective cohort study 274 septic patients
- One or more episodes of MAP <60 mmHg = increased risk of death by 2.96
- One or more episodes of MAP < 75mmHg = increased need for renal replacement therapy
-
 SEPSISPAM Trial [4] was published along side ProCESS trial April 2014
SEPSISPAM Trial [4] was published along side ProCESS trial April 2014
- Multicenter, open label trial of 776 patients with septic shock from 29 hospitals in France
- Low Target Group (MAP 65 – 70mmHg) vs High Target Group (MAP 80 – 85mmHg)
- Primary Outcome: 28 day mortality
- Also looked to see if higher MAP beneficial in patients with chronic HTN
- No Difference in 28 or 90 day mortality
- No Difference in 28 day survival without organ support
- High Target Group with increased Atrial Fibrillation (7% vs 3%)
- High Target Group on pressors longer (4.7 vs 3.7 days) and higher dose of levophed (0.40 vs 0.35µg/kg/min)
- Clinical Bottom Line: We should target a MAP of ≥65mmHg in patients with sepsis

What Hemoglobin Transfusion Threshold should we target in sepsis?
- Surviving Sepsis Campaign Recommends Keep Hematocrit (Hct) ≥30% during 1st 6 hours, then use a transfusion threshold of ≤7g/dL (Level 1B)
- Hebert PC et al. NEJM 1999 [5]: Restrictive vs Liberal Transfusion strategy in critically ill –> Mortality rate during hospitalization was lower in restrictive group 22.3% vs liberal group 28.1% (p = 0.05), but 30 day mortality had no difference 18.7% vs 23.3% (p = 0.11)
-
 Vincent JL et al. Anesthesiology 2008 [6]: Multicenter, observational study (198 European ICUs) –> Higher 30 day survival rate in the transfusion group
Vincent JL et al. Anesthesiology 2008 [6]: Multicenter, observational study (198 European ICUs) –> Higher 30 day survival rate in the transfusion group - Park DW et al Crit Care Med 2012 [7]: Multicenter, observational study (22 ICUs in Korea) –> transfused patients had a lower mortality at 28 days (24.3% vs 38.8%)
-
Transfusion Requirements In Septic Shock (TRISS) [8]: Multicenter, parallel group trial of patients in the ICU with septic shock and Hb ≤9g/dL –> 32 ICUs in Denmark, Sweden, Norway, and Finland (998 patients) –> compared liberal transfusion strategy (Hb ≤9g/dL) vs Restrictive strategy (Hb ≤7g/dL)
- No Difference in 90D Mortality: 43% vs 45% (p = 0.44)
- 1545U vs 3088 Units PRBCs transfused
- 36.1% vs 1.2% did not require transfusion
- Clinical Bottom Line: We should be using a restrictive transfusion strategy (Hb ≤7g/dL) in sepsis
How good is SIRS criteria at screening for severe sepsis?
-
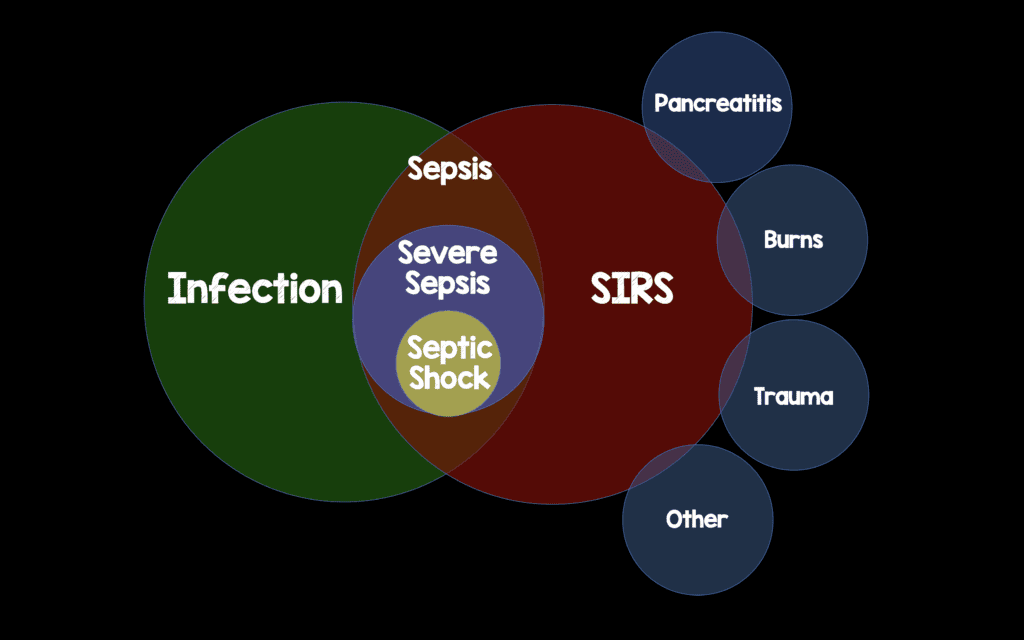 Systemic Inflammatory Response Syndrome (SIRS)
Systemic Inflammatory Response Syndrome (SIRS)
- Temp > 100.4 or < 95.0
- RR > 20 or PaCO2 < 32mmHg
- HR > 90/min
- WBC >12k or <4k or Band > 10%
- Sepsis = SIRS + Infection
- Severe Sepsis = Sepsis + Organ Dysfuncion
- Septic Shock = Severe Sepsis + Persistent Hypotension after 30cc/kg IVF Resuscitation
- Infection isn’t the only thing that can cause SIRS (poor specificity, but maybe also poor sensitivity)
- The SIRS criteria was created as a consensus statement from American College of Chest Physicians (ACCP) & Society of Critical Care Medicine (SCCM) in 1992 (Over 20 years ago)
-
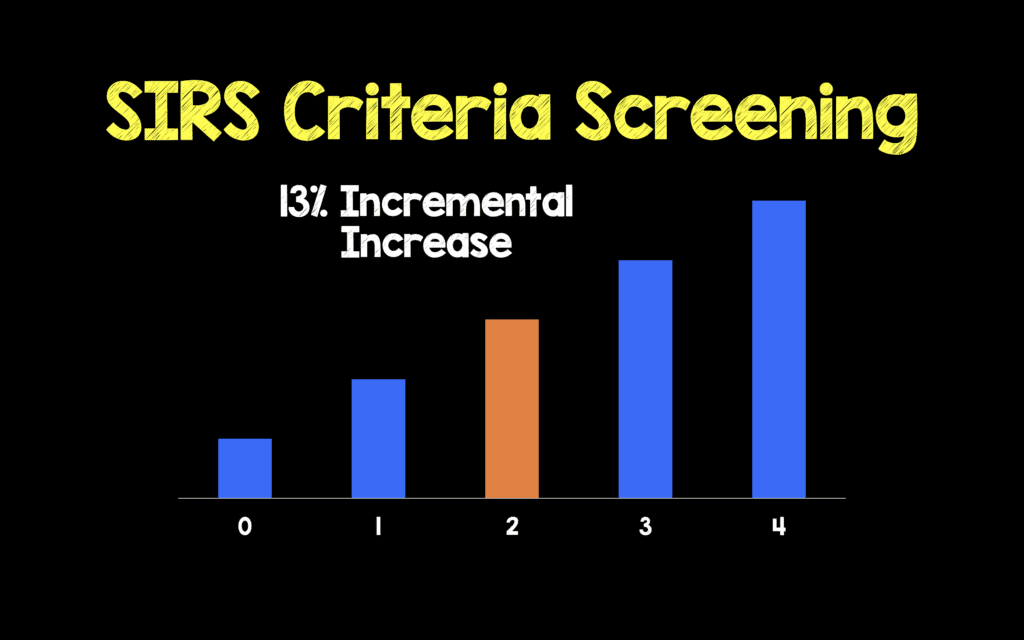 Kaukonen KM et al [9]: Retrospective analysis from 172 ICUs in Australia & New Zealand with 109,663 patients –> Looked at patients with positive infection with organ dysfunction (severe sepsis) and looked to see who had 2 SIRS Criteria
Kaukonen KM et al [9]: Retrospective analysis from 172 ICUs in Australia & New Zealand with 109,663 patients –> Looked at patients with positive infection with organ dysfunction (severe sepsis) and looked to see who had 2 SIRS Criteria
- 87.9% had 2 or more SIRS criteria
- 12.1% did not have 2 or more SIRS criteria
- Using SIRS alone will miss 1 in 8 patients with severe sepsis
- Each Additional SIRS Criteria Increased Mortality by 13% in a linear fashion without a transitional increase when 2 criteria were met….there is nothing magical about two SIRS Criteria
- Clinical Bottom Line: Using ≥2 SIRS criteria alone lacks both sensitivity and specificity for severe sepsis
What are the take home messages from the sepsis trilogy?
- There is no clear superior method in management of septic shock patients, but these studies did make it clear no one resuscitative pathway is bad or better. This gives us flexibility in the management of our patients with sepsis.
- An empiric fluid strategy in patients with sepsis should target 3 – 4.5 L IVF in 1st 6 hours.
- We have lower mortality rates now compared to the original Rivers et al study now and should give credit to Emanual Rivers. He has forever changed how we manage septic patients. Our “usual care” is now proactive and not reactive in the management of sepsis, but even after >10years since his landmark trials, none of these other trials proved superiority
- Sick patients need early fluids, antibiotics, and supportive therapies (i.e. Early critical care and resuscitation), but they don’t need CVP and SCVO2 monitoring to dictate their care .
For a full review of the sepsis trilogy, check out prior posts here:
References:
- LeDoux D et al. Effects of Perfusion Pressure on Tissue Perfusion in Septic Shock. Crit Care Med 2000. PMID: 10966242
- Bourgoin A et al. Increasing Mean Arterial Pressure in Patients with Septic Shock: Effects on Oxygen Variables and Renal Function. Crit Care Med 2005. PMID: 15818105
- Dunser MW et al. Arterial Blood Pressure During Early Sepsis and Outcome. Intensive Care Med 2009. PMID: 19189077
- Asfar P et al. High Versus Low Blood-Pressure Target in Patients with Septic Shock. NEJM 2014. PMID: 24635770
- Hebert PC et al. A Multicenter, Randomized, Controlled Clinical Trial of Transfusion Requirements in Critical Care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. NEJM 1999. PMID: 9971864
- Vincent JL et al. Are Blood Transfusions Associated with Greater Mortality Rates? Results of the Sepsis Occurrence in Acutely Ill Patients Study. Anesthesiology 2008. PMID: 18156879
- Park DW et al. Red Blood Cell Transfusions are Associated with Lower Mortality in Patients with Severe Sepsis and Septic Shock: A Propensity-Matched Analysis*. Crit Care Med 2012. PMID: 22975891
- Holst LB et al. Lower Versus Higher Hemoglobin Threshold for Transfusion in Septic Shock. NEJM 2014. PMID: 25270275
- Kaukonen KM et al. Systemic Inflammatory Response Syndrome Criteria in Defining Severe Sepsis. NEJM 2015. PMID: 25776936
The post REBEL Cast Episode 9: Sepsis Care in 2015 appeared first on REBEL EM - Emergency Medicine Blog.
