
 Background:Intubation is a commonly performed procedure in the ED and ICU. We have discussed the physiologically difficult intubation before on REBEL EM. One of the tenants in managing these patients is “resuscitate before you intubate.” Two publications in the past [1][2] discussed the incidence and risk factors associated with cardiac arrest complicating RSI. In the first study [1], 542 patient underwent emergency intubation, 4.2% had a cardiac arrest, meaning nearly 1 in 25 intubations were associated with cardiac arrest. In the second study [2], 2,403 patients underwent emergency tracheal intubation, and 1.7% had a cardiac arrest, meaning nearly 1 in 60 intubations were associated with cardiac arrest. A new study in Critical Care Medicine was just published looking at the prevalence and risk factors associated with intubation (RSI) in 64 ICUs in France.
Background:Intubation is a commonly performed procedure in the ED and ICU. We have discussed the physiologically difficult intubation before on REBEL EM. One of the tenants in managing these patients is “resuscitate before you intubate.” Two publications in the past [1][2] discussed the incidence and risk factors associated with cardiac arrest complicating RSI. In the first study [1], 542 patient underwent emergency intubation, 4.2% had a cardiac arrest, meaning nearly 1 in 25 intubations were associated with cardiac arrest. In the second study [2], 2,403 patients underwent emergency tracheal intubation, and 1.7% had a cardiac arrest, meaning nearly 1 in 60 intubations were associated with cardiac arrest. A new study in Critical Care Medicine was just published looking at the prevalence and risk factors associated with intubation (RSI) in 64 ICUs in France.
What They Did: This was a retrospective analysis of prospectively collected data from 6 prospective randomized and observational studies in 64 ICUs in France. The goal of the authors was to determine the incidenceof and risk factors associated with cardiac arrest during intubation in the ICU and its effect on immediate and 28 day mortality.
Outcomes: The primary outcome was intubation-related cardiac arrest while secondary outcomes included cardiac arrest without ROSC, complications related to the intubation, and 28 day mortality. Complications were defined as follows:
- Severe Hypoxemia: O2 sat <80% or decrease in saturation >10% in cases where highest O2 sat before intubation was <90%
- Severe Cardiovascular Collapse: SBP < 65mmHg recorded at least once or <90mmHg lasting 30 min despite 500 – 1000cc fluid load or decrease of SBP > 20% if <65mmHg before intubation or requiring pressors
- Moderately Difficult Intubation: > 2 attempts, severe VT or SVT requiring intervention, esophageal intubation, agitation, pulmonary aspiration, and dental injuries
Inclusion: Critically ill patients ≥18 years of age requiring intubation in the ICU
Exclusion: Patients admitted for cardiac arrest or intubated for cardiac arrest were excluded from the analysis
Results:
- 1,847 intubations were included for analysis
- Overall 28d Mortality Rate: 31.2%
- 49 (2.7%) patients from the of the overall population had cardiac arrest (This is nearly 1 cardiac arrest per 40 intubations)
- 14 (28.6%) patients from the cardiac arrest cohort had no ROSC
- 35 (71.4%) patients from the cardiac arrest cohort had ROSC
- Most common indications for intubation were acute respiratory failure (39%) and coma (21%)
- Anesthesiologists managed airways in 68% of cases
- Neuromuscular blockade was used in 80% of the intubations (73% succinylcholine, 11% rocuronium, and 15% other NMBs)
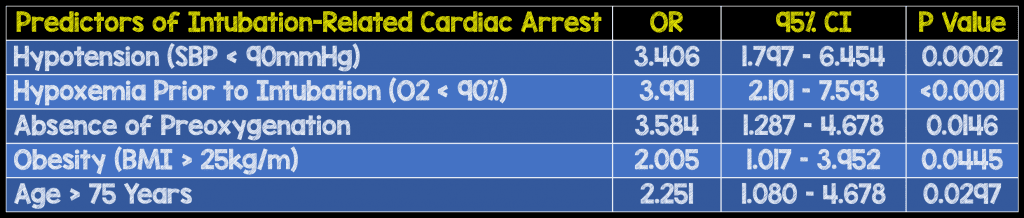
- Multivariate Analysis Identified 5 Predictors of Intubation-Related Cardiac Arrest:
- Overall 28d Mortality:
- Cardiac Arrest: 73.5%
- No Cardiac Arrest: 30.1%
- P < 0.001
- Intubation-related cardiac arrest was an independent risk factor for 28-day mortality: HR 3.9; 95% CI 2.4 – 6.3; ; < 0.0001
Strengths:
- A power calculation was performed a priori to ensure the study would be powered sufficiently to detect clinically important differences in variables allowing the authors to detect a difference ≥5.1% in their primary outcome. This reduces the risk of the study being underpowered or a false-negative/positive result. This was the first study to be adequately powered to assess risk factors for intubation-related cardiac arrest. The authors also ran multiple models to confirm the risk factors for RSI and their association with cardiac arrest, thus strengthening their conclusion.
Limitations:
- The biggest limitation of this study is that the data collected was from other studies which may have a reporting bias. Reporting bias can lead to selective recall or suppression of information by those who are reporting it. Although, the authors did a nice job with multivariate regression analyses it is possible that there may be other unmeasured confounders resulting in cardiac arrest that are not accounted for. The final issue is this is a secondary analysis of studies whose intention was not to assess cardiac arrest outcomes.
Discussion:
- Of the 5 risk factors identified, severe hypoxemia (O2 ≤80%) was the most common risk factor and the number one culprit for difficult intubation and cardiac arrest.
- Cardiac arrest was the most common during real emergency or relative emergency intubations.This is an important point, as there may not be enough time for pre-oxygenation and hemodynamic support in these “crash” airways.
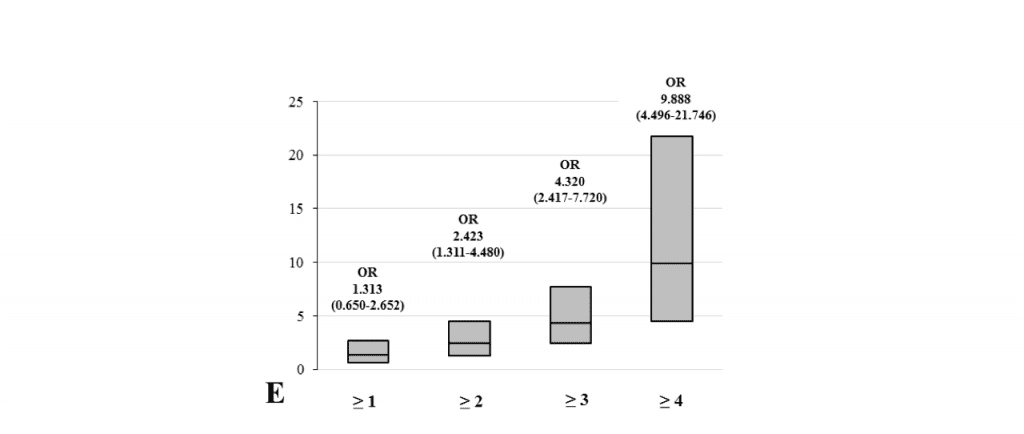
- To no one’s surprise, the more predictors of a difficult airway the patient has, the more likely the patient will have a cardiac arrest
Author Conclusion:“ICU intubation-related cardiac arrest occurs in one of 40 procedures with high immediate and 28-day mortality. We identified five independent risk factors for cardiac arrest, three of which are modifiable, possibly to decrease intubation-related cardiac arrest prevalence and 28-day ICU mortality.”
ClinicalTake Home Point: Intubation-related cardiac arrest is a real, and unfortunately common occurrence. Adding this studies numbers into the mix, anywhere from 1 in 25 to 1 in 60 ICU intubations can lead to cardiac arrest. Fortunately, there are some predictors of having a cardiac arrest due to intubation. Three of these factors are modifiable (Hypotenstion, Hypoxemia, Lack of Preoxygenation), whereas the other two are not (Obesity and Age > 75Years). So in patients that have physiologic derangements (Hypoxemia and/or Hypotension), “Resuscitate Before You Intubate!!!”
References:
- Heffner AC et al. Incidence and Factors Associated with Cardiac Arrest Complicating Emergency Airway management. Resuscitation 2013. PMID: 23911630
- Kim WY et al. Factors Associated with the Occurrence of Cardiac Arrest After Emergency Tracheal Intubation in the Emergency Department. Plos One 2014. PMID: 25402500
- De Jong A et al. Cardiac Arrest and Mortality Related to Intubation Procedure in Critically Ill adult Patients: A Multicenter Cohort Study. Crit Care Med 2018. PMID: 29261566
For More Thoughts on This Topic Checkout:
- REBEL EM: Critical Care Updates – Resuscitation Sequence Intubation – Hypotension Kills (Part 1 of 3)
- REBEL EM: Critical Care Updates – Resuscitation Sequence Intubation – Hypoxemia Kills (Part 2 of 3)
Post Peer Reviewed By: Anand Swaminathan (Twitter: @EMSwami)
The post RSI, Predictors of Cardiac Arrest Post-Intubation, and Critically Ill Adults appeared first on REBEL EM - Emergency Medicine Blog.

