
 Background: Humeral shaft fractures are commonly seen in the Emergency Department and emergency management is relatively straightforward: assess for other trauma, assess for radial nerve injury, analgesia, sling or functional bracing and follow up with orthopedics. However, there are debates in management specifically around operative vs non-operative management. The non-operative approach has been the standard but, the rate of surgery has markedly risen in the last decade (Schoch 2017). Operative management appears to reduce the risk of nonunion significantly but, comes with other risks including infections and iatrogenic radial nerve injuries. In the absence of high-quality evidence, marked practice variation persists.
Background: Humeral shaft fractures are commonly seen in the Emergency Department and emergency management is relatively straightforward: assess for other trauma, assess for radial nerve injury, analgesia, sling or functional bracing and follow up with orthopedics. However, there are debates in management specifically around operative vs non-operative management. The non-operative approach has been the standard but, the rate of surgery has markedly risen in the last decade (Schoch 2017). Operative management appears to reduce the risk of nonunion significantly but, comes with other risks including infections and iatrogenic radial nerve injuries. In the absence of high-quality evidence, marked practice variation persists.
Article: Ramo L et al. Effect of surgery vs functional bracing on functional outcome among patients with closed displaced humeral shaft fractures: The FISH randomized clinical trial. JAMA 2020. PMID: 32396179
Clinical Question: Does ORIF when compared to non-operative management result in better functional outcomes at 12 months in patients with displaced, closed humeral shaft fractures?
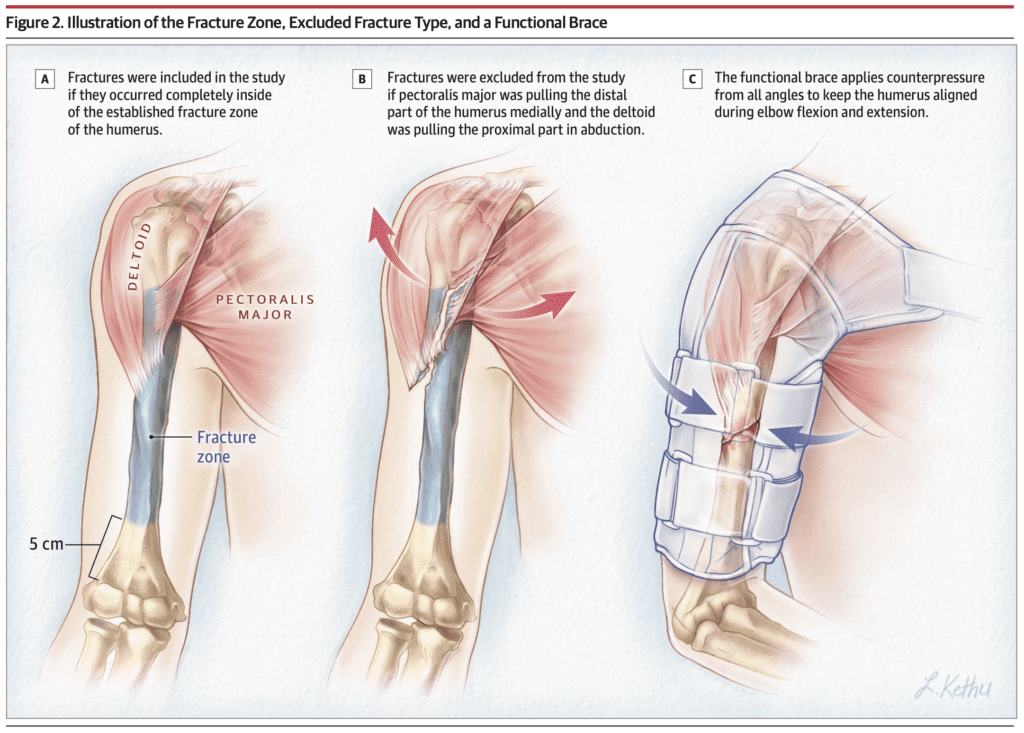
Population: Patients > 18 years of age presenting with a unilateral, displaced, closed humeral shaft fracture.
Outcomes:
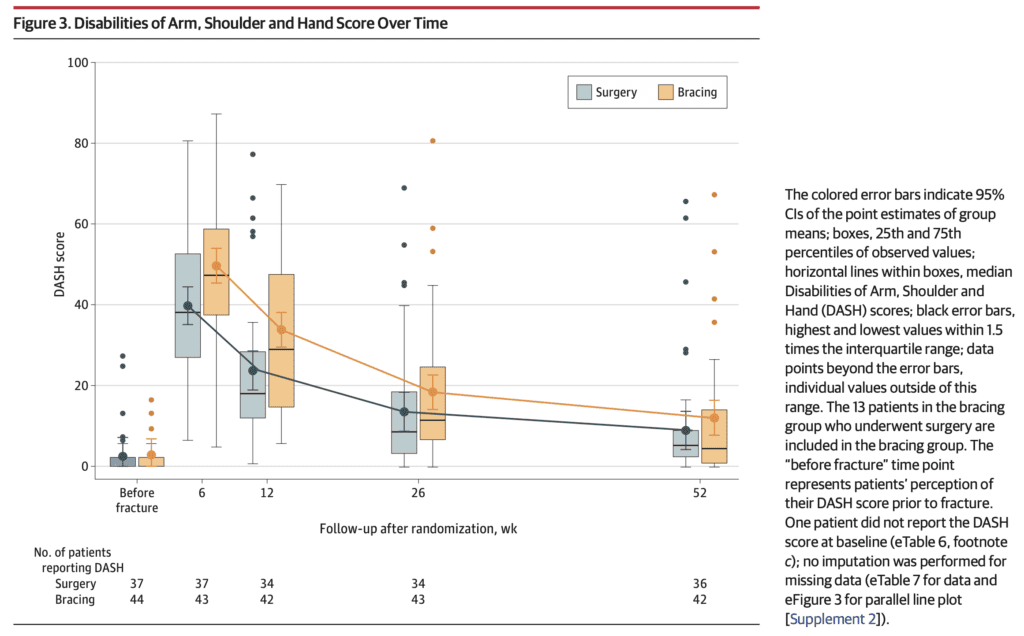
- Primary: Disabilities of Arm, Shoulder and Hand (DASH) score at 12 months (range 0 – 100 with 0 meaning no disability and 100 meaning extreme disability) with a minimal clinically important difference set at 10 based on an intention-to-treat (ITT) analysis
-
Secondary:
- Pain at rest
- Pain with activity
- Constant-Murley outcome score
- Elbow range of motion
- DASH score at other time points
- DASH work, sports and performing arts modules
- 15-dimensional tool
- Patients’ general satisfaction
Intervention: Standard open reduction and internal fixation (ORIF) with plate and screws
Control: Functional bracing (by a trained plaster technician)
Design: Non-blinded, randomized clinical trial at 2 university hospitals in Finland
Excluded:
- History of condition affecting function of injured upper limb
- Pathological fracture
- Other concomitant injury to the same upper limb
- Other fracture, internal organ, brachial plexus or vascular injury requiring surgery
- Cognitive disability preventing patient from following protocol
- Multimorbidity
- Multitrauma
Primary Results:
- Patients assessed n = 321
- Excluded n = 181
- Declined randomization n = 58
- Patients randomized n = 82
- Surgery arm n = 38
- Functional bracing arm n = 44
- Patients lost to follow-up n = 4 (2 from each group)
- Crossover to surgery within 12 months: n = 13 (8 for fracture nonunion)
Critical Findings:
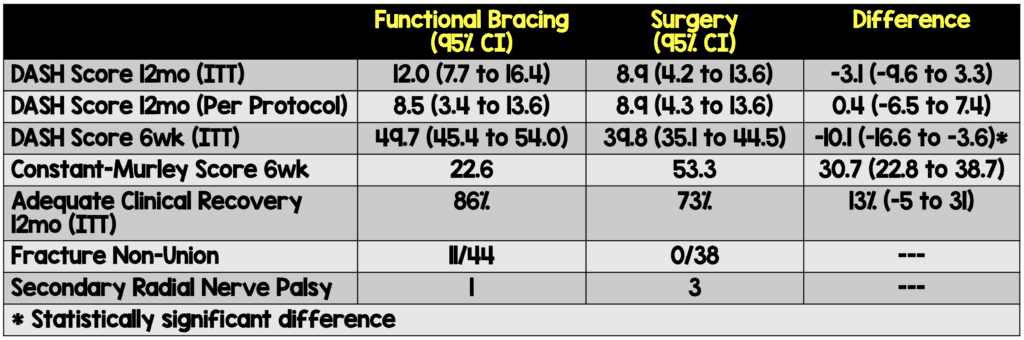
Constant-Murley Score (CMS): is a 100 point scale that is composed of a number of different parameters that define levels of pain and ability to carry out normal daily activities. The score is divided into four parts: Pain (15 points), activities of daily living (20 points), strength (25 points), and range of motion (40 points). The higher the score the higher the quality of function.
Strengths:
- Study asks a clinically important question with a patient centered outcome
- Randomization was appropriately performed
- Used a validated tool for functional assessment (DASH score)
- Patients well balanced at baseline
- Low loss to follow-up (5%) and inclusion of the declined cohort strengthen the generalizability of the findings.
Limitations:
- Though the DASH score has been validated, it is a self-assessment tool (patient scores themselves). In an unblinded study, this may lead to bias
- A large percentage of patients (29%) crossed over from bracing to surgical management within 12 months leaving only a small group of patients (n=21) for analysis as a per-protocol group
- Only patients able to engage in the protocol with closed, isolated fractures were included in this study, and patients with more complex injuries or comorbidities were excluded
- Estimates on the incidence of adverse events specific to certain procedures are subject to considerable uncertainty due to the relatively small sample size
Discussion:
- The field of orthopedic surgery doesn’t have a large number of randomized controlled trials performed so it’s important to look for and review these types of studies when they come along. Unfortunately, the number of patients in each arm, particularly after crossover, is quite small. A prior study in 2017 (Matsunaga 2017) had similar results
- A small improvement in the DASH score at 6 months that was not clinically important to patient function 7/50 patients in the functional bracing group in this study experienced non-union and required surgical fixation
- Results of this trial are not applicable to all displaced humeral shaft fractures, for 50% (91 of 181) of screened patients were excluded due to a fracture that extended either too proximally (n = 56) or too distally (n = 35)
- When this trial began, the authors had originally decided to measure 3 primary outcomes: the DASH score, pain at rest, and pain in activities, all measured at 6 weeks and at 3, 6, and 12 months. During the recruitment phase, but before any data were assessed, the steering committee decided to include only the DASH score at 12 months as the primary outcome.
- Although surgery was not significantly different in the 2 treatment groups at 12 months, the findings suggest that initial surgery provides a faster and more predictable course of recovery than functional bracing
- Eligible patients who did not consent to being randomized participated in an observational cohort (declined cohort). They received standard care (surgery or bracing) according to their preference. Postoperative treatment and outcome measures were the same as in the randomized groups
Authors Conclusions:
“Among patients with closed humeral shaft fracture, internal fixation surgery, compared with nonoperative functional bracing, did not significantly improve functional outcomes at 12 months. However, the substantial amount of treatment crossover from nonoperative to surgical treatment should be considered when interpreting the trial results.”
Our Conclusions: We agree with the authors. There doesn’t seem to be a benefit to surgical intervention but, the study is too small to make meaningful conclusions. However, in combination with the Matsunaga 2017 study, we have a consistent signal that early surgery does not improve outcomes. Larger studies are needed to confirm these findings.
References:
- Schoch BS et al. Humeral Shaft Fractures: National Trends in Management. J Orthop Traumatol 2017. PMID: 5585093
- Matsunaga FT et al. Minimally Invasive Osteosynthesis With a Bridge Plate Versus a Functional Brace for Humeral Shaft Fractures: A Randomized Controlled Trial. J Bone Joint Surg Am 2017. PMID: 28375891
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post The FISH RCT: Surgical vs Non-Surgical Management of Displaced Humeral Shaft Fractures appeared first on REBEL EM - Emergency Medicine Blog.
