

Background: The overall mortality in sepsis has decreased quite a bit in the last decade or so, however for a subset of patients, like those with Septic Shock, the mortality still remains high (as high as 50%). There have been hundreds of studies trying to identify the holy grail to decrease mortality further, but one has not been found thus far. Marik PE et al [1] published a study in Chest 2016 that has found a potential front runner. In addition, the authors go on to say, in order to have an impact on a global scale, treatments would not only need to be effective, but also cheap, safe, and readily available; the authors of the following paper may have found just that..
What They Did:
- Electronic Heath Record (EHR) retrospective before-after clinical study
- Compared the clinical course and outcome of consecutive severe sepsis (maybe clarify that this is the new definition?) and septic shock patients and a procalcitonin (PCT) ≥2ng/mL:
- Treatment Group: Treated with standard sepsis care + intravenous vitamin C, hydrocortisone and thiamine within 24 hours of ICU admission
- Control Group: Treated with standard sepsis care only.
Standard ICU Care:
- Empiric broad spectrum antibiotics giving initially, which were de-escalated according to microbiological data and clinical progress
- Conservative physiologic fluid based therapy
- Intravenous hydrocortisone 50mg q6hr
- Lung protective strategy and avoidance of hyperoxia
- Limited use of sedative agents (dexmedetomidine was the preferred agent)
- Norepinephrine was the vasopressor of choice (titrated to a dose of 20ug/min targeting a MAP >65mmHg)
- If needed, the next vasopressor added was vasopressin at 0.04 U/min, followed next with by phenylephrine or epinephrine
- Enteral nutrition was initiated 24 hours after ICU admission and clinical stability achieved
- DVT prophylaxis with enoxaparin (or heparin in patients with creatinine clearance <30ml/min) and sequential compression devices
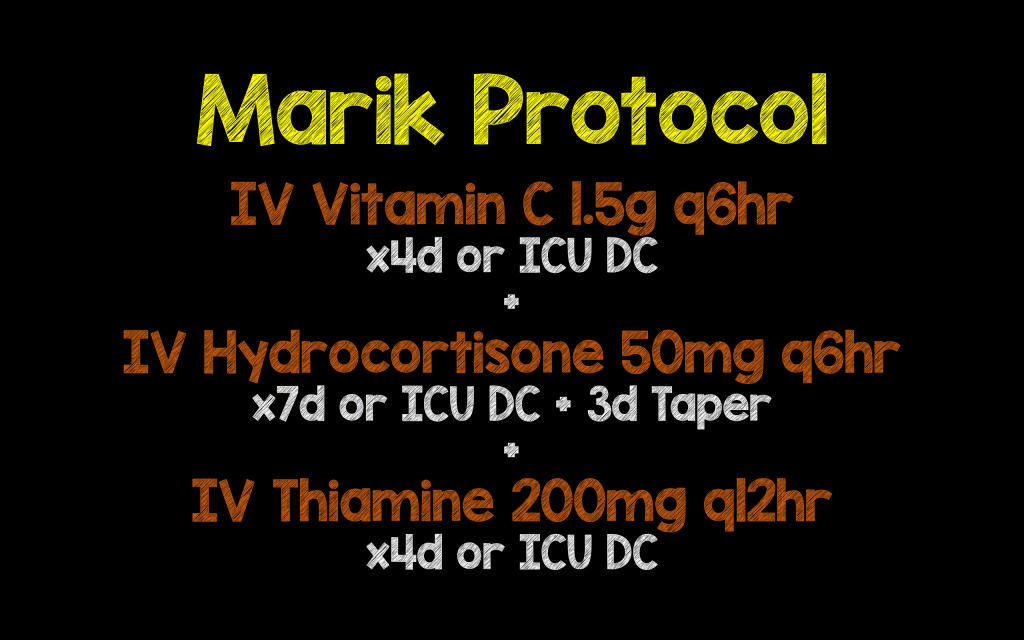
Vitamin C (Marik) Treatment Protocol:
- Standard ICU care (see above), plus:
- Intravenous vitamin C 1.5g q6hr x4d or until ICU discharge
- Hydrocortisone 50mg q6hr x7d or until ICU discharge followed by a taper over 3d
- Intravenous thiamine 200mg q12hr x4 or until ICU discharge
Outcomes:
- Primary: Hospital survival
- Secondary:
- Duration of vasopressor therapy
- Requirement for renal replacement therapy (RRT) in patients with AKI
- ICU length of stay
- Change in serum procalcitonin (PCT)
- Change in SOFA score over the first 72hours
Exclusion:
- <18 years of age
- Pregnancy
- Patients with limitations of care (DNR/Palliative)
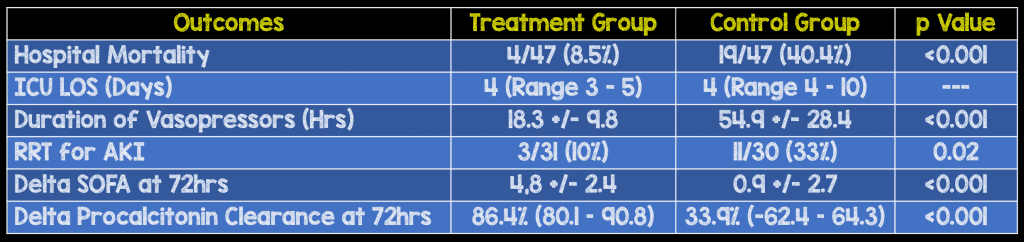
Results:
- 94 patients included in study
Strengths:
- No difference in baseline characteristics between groups
- Consecutive patients enrolled
- The studied interventions were cheap, seemingly safe (we don’t really know the long term outcomes), and readily available.
- This was the first study to evaluate the combination of intravenous vitamin C, hydrocortisone, and thiamine
Limitations:
- Not a RCT
- Small sample size
- Only a single center study
- Use of non-concurrent controls (i.e., patients were not evaluated during the same timeframe)
- PCT is not readily available at every hospital
Discussion:
- No patients in the treatment group died from complications related to sepsis, rather their mortality was secondary to complications of their underlying disease
- PCT typically decreases in a linear fashion in patients with severe sepsis (sepsis?)_and septic shock, reaching about 30% of their baseline value within 72 hours. A fall greater than 30% over 72 hours usually indicates improved survival
- The authors’ hypothesis is that vitamin C, hydrocortisone, and thiamine have synergistic effects that reverse vasoplegic shock and potentially limit the duration of vasopressor treatment resulting in a reduction in organ and limb ischemia from the vasopresors themselves.
- The paper goes on to discuss and hypothesize how the combination of vitamin C, hydrocortisone, and thiamine works. The gist of their discussion, however, is that instead of one drug working on a single pathway in sepsis, the combination of these three drugs affects multiple pathways with the added benefit of an overlapping and synergistic effect.
- The exact dosing strategy for Vitamin C is unknown, as it is not been well studied. The authors conclude that up to 6 grams daily should be enough without running the risk of conversion to oxalate and potentially causing worsening renal impairment from oxalate crystal formation and renal deposition.
Author Conclusion: “Our results suggest that the early use of intravenous vitamin C, together with corticosteroids and thiamine may prove to be effective in preventing progressive organ dysfunction including acute kidney injury and reducing the mortality of patients with severe sepsis and septic shock. Additional studies are required to confirm these preliminary findings.”
Clinical Take Home Point: Although the results of this study are very promising, it is important to remember that this was only a hypothesis generating study. We still need an external validation before implementation (How many other treatments in sepsis have been touted as a “cure” and not panned out in subsequent studies?).
Expert Peer Review

Haney Mallemat
University of Maryland School of Medicine, Baltimore, MD
Assistant Professor of Emergency Medicine
Twitter: @criticalcarenow
Blog: Keynotable
There have been many exciting clinical trials for critically ill patients over the years (e.g., Early Goal Directed Therapy, tight glycemic control, etc.). Many of these trials have generated excitement when they were first published, but many have also failed replication during external validation. For example, you will recall that tight glycemic control [2] was only demonstrated to have benefit for patients in a single center surgical ICU, but based on this single study by Van der Berg, tight glycemic control was extrapolated to many subsets of critically-ill patients and even non-critically ill patients in the hospital. Subsequent studies could not demonstrate the same benefits that were seen in Van der Berg’s trial and in fact, a strategy of tight glycemic control was found to cause increased harm (e.g., hypoglycemia, seizures, etc.) This is not only an example of a failure of an initial, single center study that could not be externally validated, but this is also an example of a seemly benign treatment (i.e., keeping glucose levels normal) that was subsequently shown to have patient harm once it was rigorously studied.
Now let’s turn our attention to Marik’s article discussed in this post. The components of Marik’s life-saving sepsis cocktail are simply steroids and vitamins, a therapy, which many have said is harmless, but may improve sepsis survival dramatically. Steroids for sepsis have been around decades, and although there have been several trials evaluating its benefits in the septic patient; it is safe to say that the use of steroids remains controversial. The recently completed HYPRESS trial did not demonstrate a benefit for steroids in patients with sepsis. How about the use of vitamin C and thiamine? This is not a new concept and there are studies demonstrating benefit so perhaps, combining all these “harmless” therapies would work on the deranged physiologic pathways that are present in the septic patient.
So the conjecture here is that Marik’s new cocktail has little patient harm because the individual components are individually benign and have been studied before. In fact, Marik himself has made the claim that withholding this therapy while waiting for a multicenter trial to be completed would be unethical. In support of his statement he has even invoked the infamous “parachute analogy” where some therapies are so obvious that it would be illogical to test them in a clinical trial.
Before we get carried away and start vigorously applying the findings of this trial on our septic patients, let’s just remember a few things: 1) this was not a large trial, 2) this trial was not a randomized control trial, it was a before and after trial (which breeds all types of biases), 3) it was a single center study, and 4) we do not know the optimal dosing strategy of these drugs (or if there even exists one). But here’s my biggest problem with using this therapy on my patients, we simply do not know if these therapies are truly benign, either alone or in combination. Until a trial is done to truly evaluate the effects of this combination therapy and the harm that might not have been detected yet, I would claim that it is unethical to use this therapy in the routine septic patient.
If we have learned anything from our history, it is that even things that seem benign such as tight glycemic control can be harmful if not carefully looked at systematically. Whether this therapy eventually does turn out to be life saving (or whether it causes harm), we must remember that our primary job as clinicians is to administer therapies that have been vigorously proven by science and not simply based on parachute reasoning. If we hold ourselves to a standard less than that, and one based on logical reasoning then we would have never demonstrated in multiple subsequent trials that tight glycemic control was actually harmful to patients. Therapies based on only logic should only be considered when there are no other alternatives.
I hope that Marik’s new therapy for sepsis will prove to be as robust as the authors have demonstrated. As such, I sincerely hope that a prospective multi-center randomized control trial will be conducted soon so we may improve our patients’ mortality in sepsis. But let’s not forget that such a trial might actually demonstrate patient harm when systematically looking for it in a clinical trial.
References:
- Marik PE et al. Hydrocortisone, Vitamin C and Thiamine for the Treatment of Severe Sepsis and Septic Shock: A retrospective Before-After Study. Chest 2016. S0012-3692(16)62564 – 3. PMID: 27940189
- Van den Berghe G et al. Intensive Insulin Therapy in Critically Ill Patients. NEJM 2001; 345(19) 1359 – 67. PMID: 11794168
For More Thoughts on This Topic Checkout:
- Steve Mathieu at The Bottom Line: An Orange a Day Keeps Sepsis at Bay?
- Ryan Radecki at EMLit of Note: Vitamin C for Sepsis
- Josh Farkas at PulmCrit (EMCrit):Metabolic Sepsis Resuscitation – The Evidence Behind Vitamin C
- Scott Weingart on EMCrit: Paul Marik on the Metabolic Resuscitation of Sepsis
- Pharmacy Joe: Vitamin C, Hydrocortisone, and Thiamine for Severe Sepsis and Septic Shock
- Adam Rieves at Everyday EBM: Vitamin C in Sepsis – Splashes in the Popular Press
- PulmCCM: Could Vitamin C Save Lives in Sepsis? These Hospitals Aren’t Waiting for Proof
- Dan Horner at St. Emlyn’s Blog: JC – Vitamin SCepTiC?
- Ken Milne at The SGEM: SGEM#174 – Don’t Believe the Hype – Vitamin C Cocktail for Sepsis
Post Peer Reviewed By: Haney Mallemat (Twitter: @CriticalCareNow)
The post The Marik Protocol: Have We Found a “Cure” for Severe Sepsis and Septic Shock? appeared first on REBEL EM - Emergency Medicine Blog.
