 Severe sepsis and septic shock affect millions of patients worldwide and have high rates of morbidity and mortality as well as high resource utilization. The way we manage sepsis has changed quite a bit since the Rivers et al randomized controlled trial of early goal-directed therapy (EGDT) 1 , which had an absolute decrease in mortality from 46% with “usual care” to 31% with EGDT. What we now know is that a proactive approach to septic patients will result in lower mortality rates and better outcomes (i.e. early identification, early intravenous fluids, and early antibiotics). Patients with sepsis are still missed despite the fact that we understand the benefits to morbidity and mortality with early recognition. In this blast from the past study from 2007, Howell et al 2 answered the important question of does elevated lactic acid simply reflect a patient’s hemodynamic status or can it independently predict 28 day in-hospital mortality after controlling for other potential confounders in patients with sepsis.
Severe sepsis and septic shock affect millions of patients worldwide and have high rates of morbidity and mortality as well as high resource utilization. The way we manage sepsis has changed quite a bit since the Rivers et al randomized controlled trial of early goal-directed therapy (EGDT) 1 , which had an absolute decrease in mortality from 46% with “usual care” to 31% with EGDT. What we now know is that a proactive approach to septic patients will result in lower mortality rates and better outcomes (i.e. early identification, early intravenous fluids, and early antibiotics). Patients with sepsis are still missed despite the fact that we understand the benefits to morbidity and mortality with early recognition. In this blast from the past study from 2007, Howell et al 2 answered the important question of does elevated lactic acid simply reflect a patient’s hemodynamic status or can it independently predict 28 day in-hospital mortality after controlling for other potential confounders in patients with sepsis.
What They Did
- Single-center, prospective, observational cohort study of patients with clinically suspected infection
- To determine, in the early stages of suspected infection, the independent relationship of the presenting venous lactate level to 28-day in-hospital mortality
- 1,287 adult patients admitted through the emergency department with clinically suspected infection and an initial lactate measurement
Outcomes
- Relationship of initial venous lactate to 28-day in-hospital mortality
Results
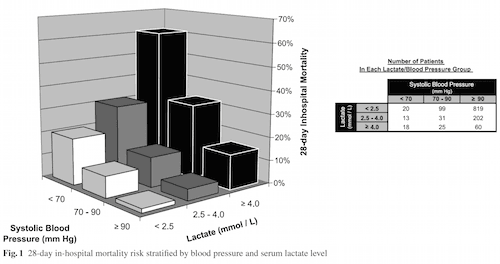
- Lactate level was strongly associated with mortality. The study used a lactate level of <2.5 mmol/L as the reference group:
- Unadjusted odds of death (lactate level 2.5 – 4.0 mmol/L) = 2.7
- Unadjusted odds of death (lactate level ≥4 mmol/L) = 12.6
- When controlled for blood pressure, lactate was still significantly associated with mortality (p <0.0001)
- After controlling for age and blood pressure, lactate was still significantly associated with mortality when using a lactate level of <2.5 mmol/L as the reference group:
- Adjusted odds of death (lactate level 2.5 – 4.0 mmol/L) = 2.2
- Adjusted odds of death (lactate level ≥4 mmol/L) = 7.1
- Patients with presence of shock or elevated lactate had a mortality rate of 28% vs 2.5% in patients who did not fulfill either criterion
Limitations
- The mortality rate in this study is much lower than what has traditionally been seen in other sepsis studies (i.e. 5.7% in this study vs 46% in the Rivers trial). This could imply that this was a healthier patient population, and there may be other variables that may be significant independent predictors of mortality that could not be accounted for.
- Even though this was a prospective cohort of patients, predictor variables were recorded from medical records. Some variables may have been incorrectly recorded, which could cause misclassification of patients, but this would be expected to weaken not strengthen the relationship of predictors to mortality.
- During the study period an EGDT protocol was being used in patients with clinically suspected infection, meaning in order to generalize the lactate level to predict mortality in centers not using this protocol would require external validation.
- There were also 58 patients included with do-not-resuscitate (DNR) status of which 11 died.
- The median length of stay in the emergency department was 8 hours. This makes it possible that initial lactate levels were drawn in some patients after having received some resuscitative measures prior to lactate sampling, which could skew the results.
- Infected patients may have been missed if their lactate level was not measured, which creates a selection bias. Inclusion in the study depends on two things: a lactate level was drawn and physicians suspicion of an infection. This could exclude really well appearing patients with infection if not recognized by the physician. Adding this population of patients to the study may have created a stronger association between lactate levels and mortality.
Discussion
- There were 835 patients with clinically suspected infection did not have lactate levels measured and were not included in this analysis, but it is important to note that the morality rate was much lower in this group (i.e. 10/835 or 1.2%) compared to the population that did have lactate levels drawn.
- This study tells us that among patients admitted to the hospital with clinically suspected infection, a single measurement of the venous lactate level provides important prognostic information over and above that conveyed by hemodynamic status and comorbidities.
- Physiologically, in patients with clinically suspected infection and failure of oxygen extraction at the microvascular level, there will be a rise in circulating lactate levels early in the course of disease, when vital signs are not yet compromised, allowing for earlier identification of these patients with occult shock.
- It is also important to remember that by the time patients arrive to the intensive care unit (ICU), they have usually received initial treatment and resuscitation. Therefore, predicative instruments validated in the ICU, may not perform as well in an emergency department population who has not had initial attempts at resuscitation.
- Also noteworthy from this study was the fact that elevated BUN levels and low platelets are independently associated with increased mortality in sepsis patients
- Finally, a screening lactate will improve the number of patients identified with sepsis, but will not catch all patients with occult sepsis. This study does not comment on that fact.
Author Conclusion
In patients admitted with clinically suspected infection, the venous lactate level predicts 28-day in-hospital mortality independent of blood pressure and adds significant prognostic information to that provided by other clinical predictors
Clinical Take Home Message
A screening venous lactate will help identify a substantial number of patients who may have normal vital signs but still have clinically important hypoperfusion and may otherwise remain undetected.
Author information
The post Blast From the Past: Occult Sepsis, Lactic Acid, and Mortality appeared first on ALiEM.

