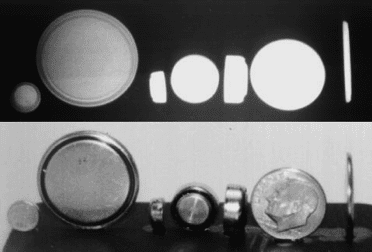
 Button Batteries: Small, disc shaped battery cells which are designed for use in small electronic devices. Common sources are kids toys, watches, calculators and hearing aids. Most batteries use lithium as a power source
Button Batteries: Small, disc shaped battery cells which are designed for use in small electronic devices. Common sources are kids toys, watches, calculators and hearing aids. Most batteries use lithium as a power source
Button Battery Ingestion Danger:
- Contact with mucosal surfaces (oropharynx, esophagus, nasal passage) results in transmission of current
- Current transmission causes chemical burns and necrosis via alkaline injury (sodium hydroxide)
- Tissue damage can progress rapidly and result in devastating injuries
- Nasal passage and esophagus are most susceptible to injury (narrow places for battery to become lodged)
-
Injury Patterns
- Viscous perforation
- Fistula formation
- Erosion into blood vessels and resultant bleeding and possible catastrophic bleeding with erosion into aorta
When to Suspect Ingestion:
-
Reported pediatric ingestion of unknown substance
- Parent may report seeing “shiny” object being placed in mouth
- Parent may report missing battery from open electronic device
-
Typical foreign body ingestion symptoms
- Coughing
- Gagging
- Drooling
- Dysphagia
- Increased work of breathing or stridor
-
Symptoms consistent with tissue damage
- Vomiting
- Chest discomfort
- Fever
- Hematemesis
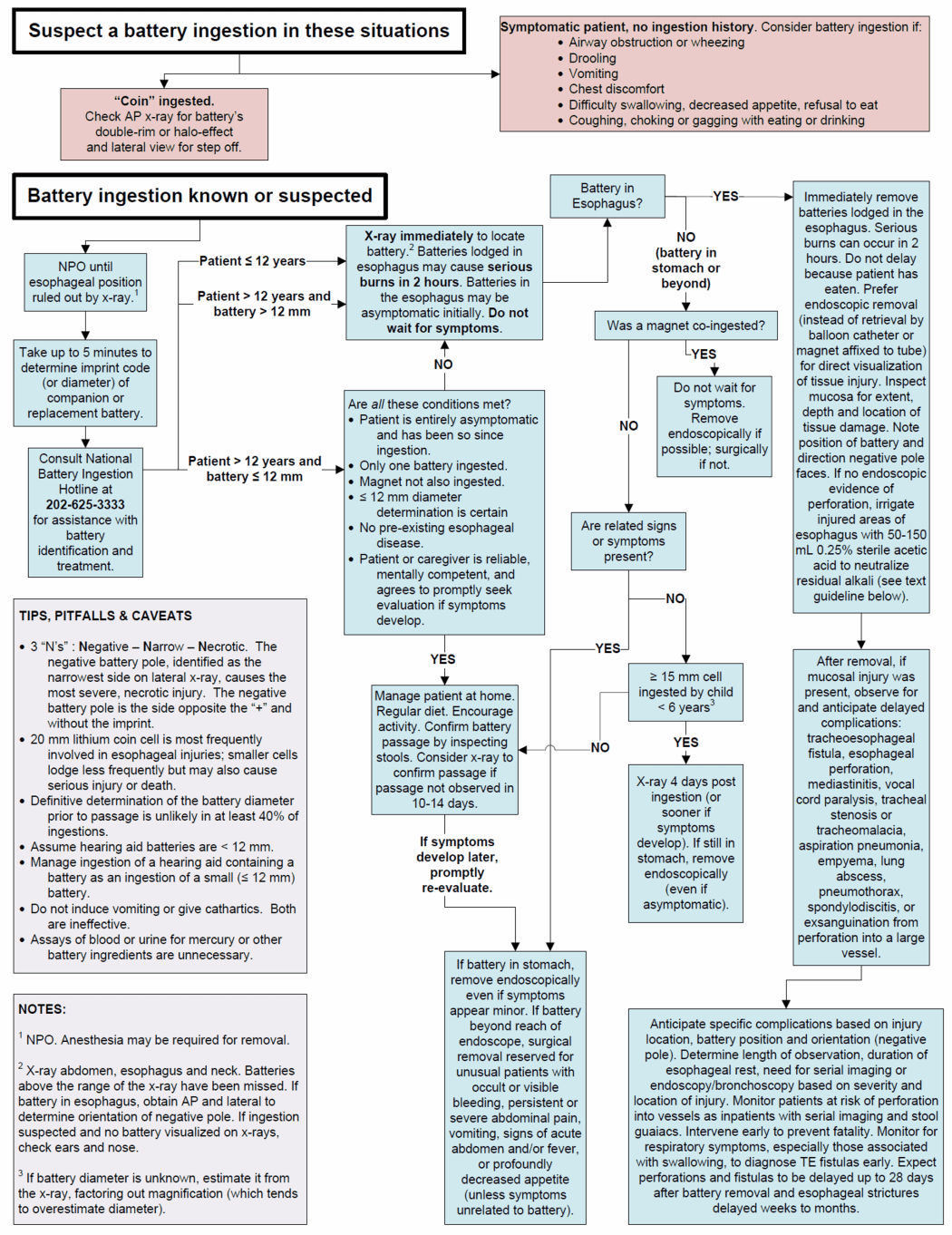
Imaging:
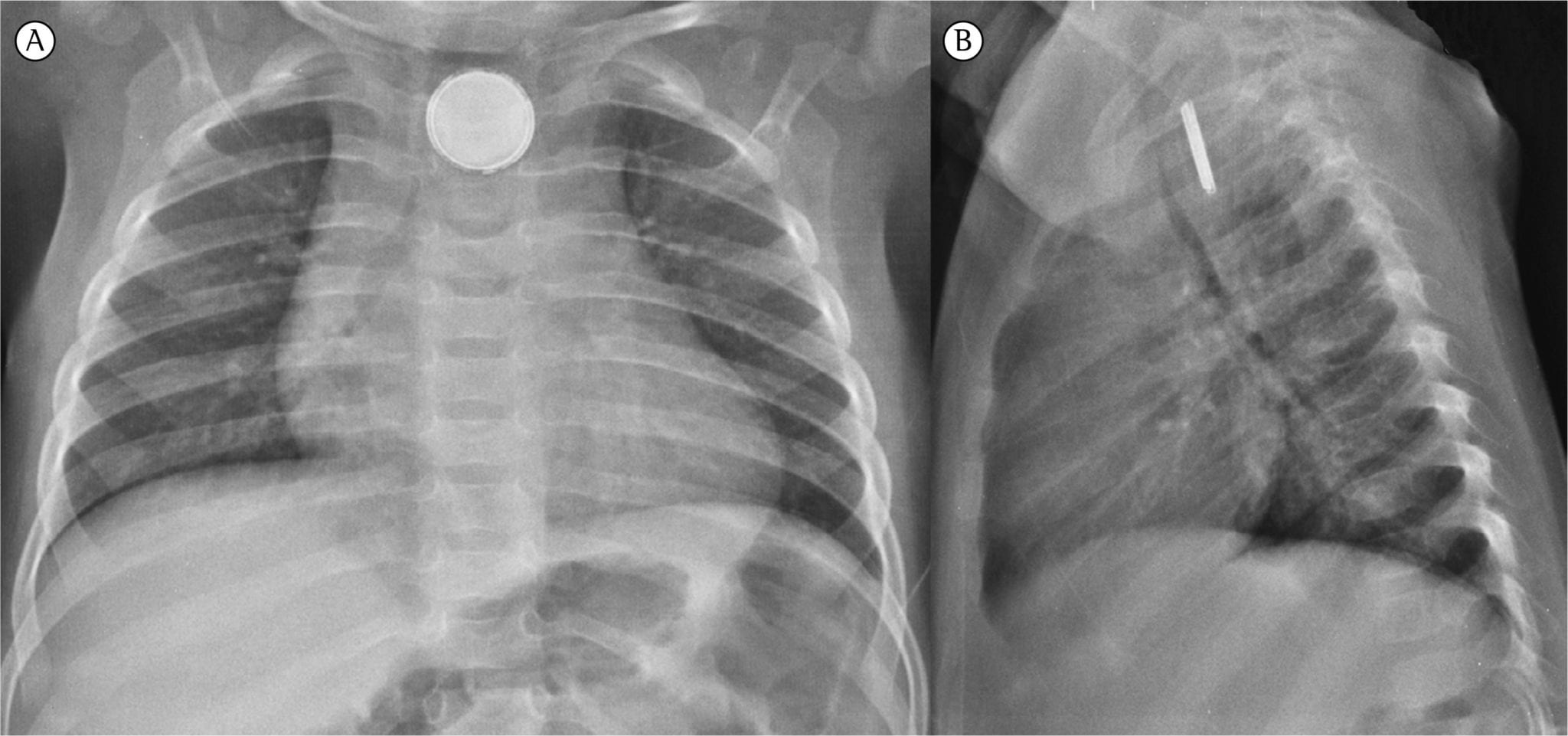
- Batteries are radio-opaque and will appear on plain X-rays
- Views: At least 2 (PA and lateral)
- Nasal placement: Obtain skull X-ray
- Swallowed battery: Chest X-ray
-
Battery vs. Coin
- Battery can often be mistake for the more benign coin ingestion on X-ray
- En face view: may see a ring of radiolucency inside outer edge of object (“halo rim”)
- On edge view: may see a central bulge with a battery
ED Management:
-
Supportive Care
- Aggressively resuscitate patients with hematemesis and/or signs of shock
- Look for signs/symptoms of airway obstruction and control airway if necessary
- Keep patient NPO
- Obtain X-ray for localization of button battery
- Nasal and Esophageal batteries should be removed within 2 hours of presentation to avoid significant necrosis. Do Not Wait for Symptoms to Develop!
-
Nasal battery
- If battery can be visualized, can attempt removal with forceps, suction, skin glue on cotton swab or any other standard approach
- If cannot visualize battery, obtain ENT consultation for direct visualization and removal with fiberoptics
-
GI Tract Battery
-
X-ray localizes to esophagus
- Emergency consultation (Institution dependent – GI, Peds surgery) for direct visualization and removal
-
Removal without direct visualization (i.e. foley catheter removal) sub-optimal
- Does not allow for visualization of mucosal injury
- May result in translocation of of the battery from the esophagus to the trachea
- If patient exhibits any evidence of mucosal damage, admit for observation
-
X-ray localizes distal to esophagus (i.e. stomach, small intestine)
-
Symptomatic or magnet co-ingestion
- Emergency consultation (Institution dependent – GI, Peds surgery) for direct visualization and removal
- Battery and magnet can cause problems even after passage into stomach via attraction of geographically distinct parts of bowel leading to obstruction or mucosal necrosis
-
Asymptomatic
-
If battery > 15 mm in child < 6 years of age
- Lower risk of spontaneous passage
- Repeat X-ray in 4 days. If battery still in stomach, remove under endoscopy
-
Expectant Management
- Discharge home
- Regular diet
- Confirm passage by stool inspection or repeat X-ray in 10-14 days (if no passage, consider removal)
-
If battery > 15 mm in child < 6 years of age
-
Symptomatic or magnet co-ingestion
-
Continued Management
- Development of any symptoms in a patient with battery beyond esophagus should prompt removal
- Delayed perforation possible up to 28 days out of ingestion
- Some gastroenterologists recommend routine repeat endoscopy
-
X-ray localizes to esophagus
Take Home Points:
- Button battery ingestions are extremely dangerous. Necrosis, perforation and erosion into vessels can occur in as little as 2 hours
- ALL esophageal button batteries should be removed within 2 hours of presentation to minimize mucosal damage
- Consider button battery ingestion in children presenting with dysphagia, refusal to eat and hematemesis
- Co-ingestion of a button battery with a magnet requires emergency removal regardless of where it is in the GI system
For More on This Topic Checkout:
- National Capital Poison Center: NBIH Button Battery Ingestion Triage and Treatment Guideline
- Pediatric EM Morsels: Button Battery Ingestion
- St. Emlyn’s: Button Batteries – Hide and Seek in the Emergency Department
- ENT Blog: Lithium Disc Battery Danger for Kids
Post Peer Reviewed By: Salim Rezaie (Twitter: @srrezaie)
The post Button Battery Ingestion appeared first on REBEL EM - Emergency Medicine Blog.