 This year ACEP 2018 took place in San Diego, CA from Oct 1st– 4th, 2018. There were lots of amazing speakers and topics as was evidenced by the eruption of everyone’s twitter feeds with the #ACEP18 hashtag. I was fortunate enough to not only attend, but also speak at this amazing conference. I was approached by several attendees requesting that I put together a list of my favorite pearls from this conference, as I have done in years past on REBEL EM. Below is my top 10 list, in no particular order.
This year ACEP 2018 took place in San Diego, CA from Oct 1st– 4th, 2018. There were lots of amazing speakers and topics as was evidenced by the eruption of everyone’s twitter feeds with the #ACEP18 hashtag. I was fortunate enough to not only attend, but also speak at this amazing conference. I was approached by several attendees requesting that I put together a list of my favorite pearls from this conference, as I have done in years past on REBEL EM. Below is my top 10 list, in no particular order.
Pearl #1: Plateau Pressure is More Important than the Peak Inspiratory Pressure When Patients are on the Ventilator – Mike Winters
- Although EM physicians frequently intubate patients, many are not facile with ventilator management
- 394 EM attendings surveyed, 211 responded (53.6%) à5% reported receiving ≤3 hours of ventilation-related education from EM sources over the past year and 46% reported receiving between 0 – 1 hour of education [1]
- Ventilator Pressures: Peak Inspiratory Pressure & Plateau Pressure
- Peak Pressure – Reflects the pressure from airflow resistance and respiratory system compliance (measured during inspiratory flow); it is the pressure to overcome endotracheal tube and the large proximal airways & the elastic pressure of the lung (pressure to distend the small airways and the alveoli)
- Plateau Pressure (PPlat): The pressure needed to distend the small airway and alveoli (Measure with end-inspiratory hold); The goal is to keep PPlat <30cm H20.
Pearl #2: Computerized Interpretation of the Electrocardiogram is NOT Accurate [2] – Amal Mattu
- 855 triage ECGs collected à222 (26%) interpreted by computer as normal à1/222 had clinical significance [3]
- If we get on average 10 ECGs per shift + Work 15 Shifts in a month = 150 ECGs/month àOver 12 months this equals 1,800 ECGs/year àThis means we would miss 8 clinically significant bad outcomes over the course of the year if we depended on computerized interpretation of ECGs
- ECG computers are not programmed to pick up subtle changes and if we depend on this read will miss subtle signs of ACS
- Also, when in doubt, get a 2ndECG, as ACS is a dynamic process
Pearl #3: There is NO High-Level Evidence that Pre-Hospital Spinal Immobilization in Trauma Patients Positively Impacts Patient Oriented Outcomes – Christopher Colwell
- Spinal Immobilization:
- Does NOT Help Immobilize the Cervical Spine [4]
- Does NOT Decrease Rates of Spinal Cord Injury [5]
- INCREASES the Difficulty of Airway management [6]
- CAN Cause Pressure Ulcers [7]
- CHANGES the Physical Exam [8]
- Worsens Pulmonary Function [9]
- INCREASES Intracranial Pressure [10]
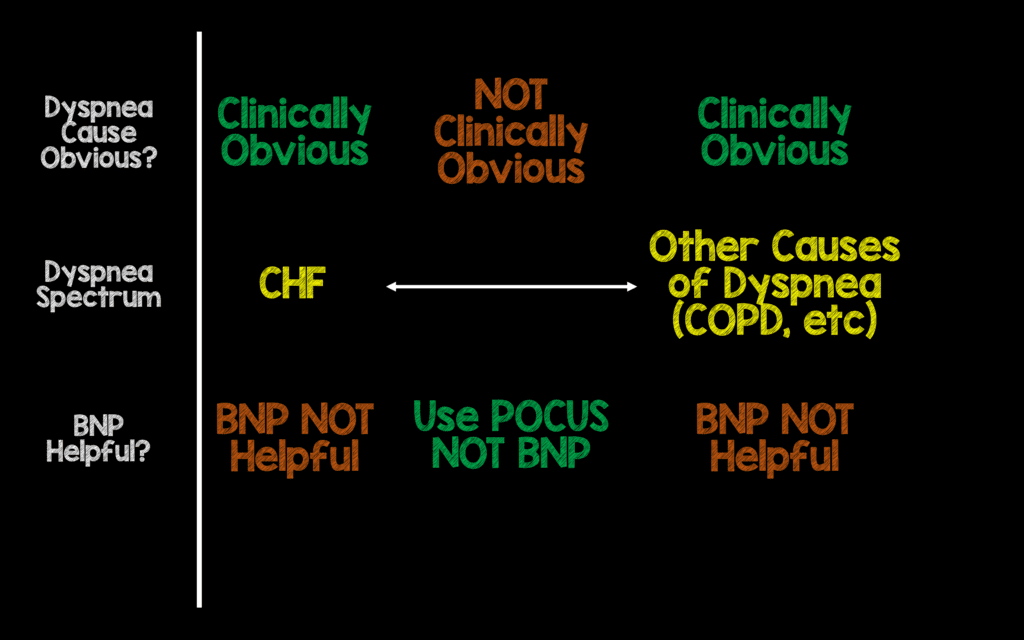
Pearl #4: BNP is NOT Helpful in the Diagnosis of CHF – Jerome Hoffman & Rick Bukata
- Physician gestalt is already accurate in patients with clinically obvious CHF
- BNP is not associated with improving patient oriented outcomes such as length of stay, return visits, and overall health care costs [11]
- 201 patients with intermediate probability of CHFàNo difference in the accuracy of ED physicians diagnosis, time to diagnosis, time to discharge, length of stay, ICU admission rate, or 60 day survival [12]
- BNP is NOT helpful at extremes when the diagnosis is clinically obvious, and less helpful in patients that are less clinically obvious. Use history & POCUS in these cases not BNP.
Pearl #5: Good PreOx Makes ApOx Superfluous in the ED in Most Cases – Anand Swaminathan
- Single Institution RCT of Apneic Oxygenation (ApOx) vs Usual Care à200 patients randomized àNo difference in mean lowest SpO2 [13]
- In patients who receive proper pre-oxygenation (PreOx), defined as 3 minutes with flush 100% O2, apneic oxygenation may be a superfluous intervention
- ApOx is not a complicated procedure, not expensive, and has not been shown to be harmful. The absence of benefit doesn’t mean there is no group who won’t benefit (i.e. prolonged apnea times and crash intubations) and should be continued to be used until we have better ways to predict which intubations are going to be difficult.
Pearl #6: It is Completely Normal and Expected to Have a Cough for 2 or even 3 Weeks After Onset of Upper Respiratory Illness – Jerome Hoffman & Rick Bukata
- Don’t forget to tell patients that cough from upper respiratory illness can last approximately 3 weeks
- A systematic review of 1821 patients with upper respiratory infection àDuration of cough 15.3 – 28.6 days [14]
- It is important to emphasize the natural history of cough from respiratory illness with patients when they seek care for an episode of acute cough from respiratory illness. It is also important to emphasize that they should seek care if they are having worsening symptoms.
Pearl #7: Measuring the Volume of Intra-Parenchymal Hemorrhage (IPH) on CT is as Simple as ABC/2 [15] – Matthew Siket
- Hemorrhage volume can be a predictor of 30-day mortality after spontaneous ICH
- ABC/2
- A = Largest hemorrhage diameter on CT
- B = Diameter 90 degrees to A on the same slice
- C = Approximate number of CT slices with hemorrhage multiplied by slice thickness (CT slices are usually measured in millimeters, so count # of 5mm cuts, then divide by 2)
- Divided by 2 (/2) = approximates an ellipsoid
- MDCalc has the formulafor you, so you can just type in the measurements
Pearl #8: Cardiovascular Testing in ED Patients with Low Risk Chest Pain is Associated with Increased Downstream Testing WITHOUT a Reduction in Acute Myocardial Infarctions [16] – Jerome Hoffman & Rick Bukata
- Retrospective cohort analysis of 926,633 patients between noninvasive testing or coronary angiography within 2 days or 30 days of presentation for chest pain vs no testing
- Testing within 2 days vs no testing associated with:
- Increase in coronary angiography (7.7 per 1000 patients tested) at 1 year
- Increase in revascularization PCI and/or CABG (15.0 per 1000 patients tested) at 1 year
- NO SIGNIFICANT change in AMI admission (2.3 per 1000 patients tested) at 1 year
- Testing within 30 days vs no testing associated with:
- Increase in coronary angiography (36.5 per 1000 patients tested) at 1 year
- Increase in revascularization – PCI and/or CABG (22.8 per 1000 patients tested) at 1 year
- Increase but NOT SIGNIFICANT change in AMI admission (7.8 per 1000 patients tested)
- No subgroup in which testing was performed was associated with reduction in AMI admissions
- Testing within 2 days vs no testing associated with:
- Cardiac testing in patients presenting to the ED with chest pain was associated with increased downstream testing and treatment without a statistically significant reduction in AMI admissions and deferral of testing is not associated with worse outcomes
Pearl #9: Capnography Tells you What Your Patients Oxygen Saturation Will Be, Pulse Oximetery Tells you What Your Patients Oxygen Saturation Was – Mike Winters
- Pulse Oximetry measures oxygenation or amount of arterial blood oxygen saturation via device clipped to the finger or earlobe. Pulse ox may take time to detect potential problems, and may appear normal even if a patient is not breathing (i.e. the pulse ox lag)
- Also, when a patient desaturates, the pulse ox will lag even when you are providing good oxygenation (i.e. delayed increase in pulse ox)
- Capnography reflects breath to breath ventilation, detects hypoventilation/apnea immediately, and does not appear normal if your patient is not breathing
- 70 patients underwent sedated diagnostic colonoscopy (35 with supplemental oxygen and 35 without supplemental oxygen) [17]
- After sedation SpO2 decreased as alveolar hypoventilation developed in each group
- At peak etCO2, SpO2 was significantly increased by more than 5% in the oxygen supplementation group when compared with the room air group (98.6% vs 93.1%)
- SpO2 monitoring during oxygen supplementation overestimates SpO2 and provides little information about adequacy of alveolar hypoventilation
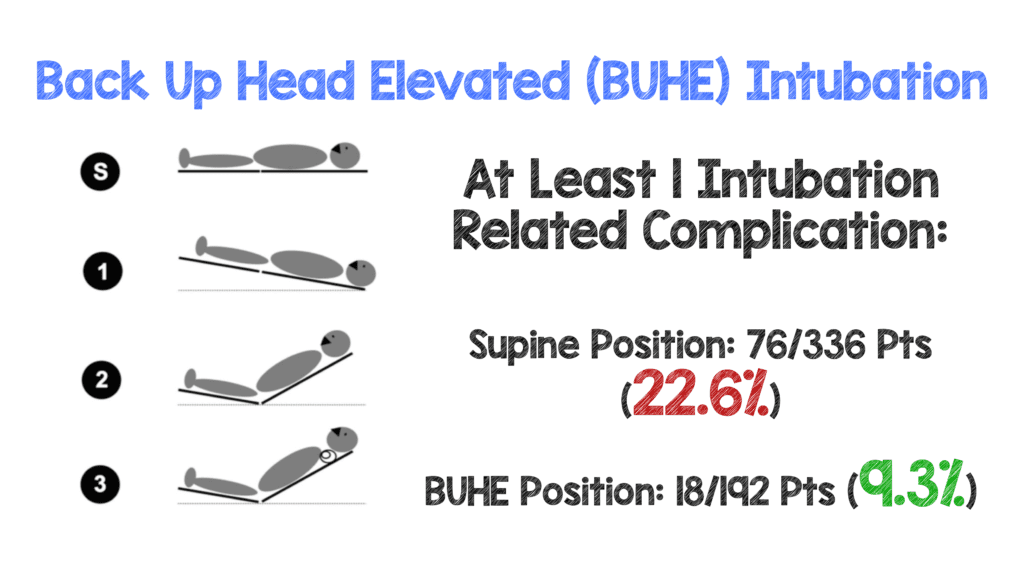
Pearl #10: Back Up Head Elevated (BUHE) Intubation is Better than Supine Intubation [18] – Anand Swaminathan
- Retrospective review of all adult patients undergoing emergent tracheal intubation outside of the operating room
- 528 patients analyzed
- Intubation-related complications:
- ≥3 Attempts or >10min Duration
- Hypoxemia <90% SpO2
- Esophageal Intubation or Esophageal Aspiration
- Intubation Related Complication:
- Supine Position: 22.6%
- BUHE Position: 9.3%
References:
- Wilcox SR et al. Acdemic Emergency medicine Physicians’ Knowledge of Mechanical Ventilation. WJEM 2016. PMID: 27330658
- Schlapfer J et al. Computer-Interpreted Electrocardiograms: Benefits and Limitations. JACC 2017. PMID: 28838369
- Hughes KE et al. Safety of Computer Interpretation of Normal Triage Electrocardiograms. Acad Emerg Med 2017. PMID: 27519772
- Wampler DA et al. The Long Spine Board Does not Reduce Lateral Motion During Transport – A Randomized Healthy volunteer Crossover Trial. Am J Emerg Med 2016; 34(4): 717 – 21. PMID: 26827233
- Hauswald M et al. Out-of-Hospital Spinal Immobilization: Its Effect on Neurologic Injury. Academic Emergency Medicine 1998; 5(3): 214 – 219. PMID: 9523928
- Durga P et al. Effect of Rigid Cervical Collar on Tracheal Intubation Using Airtraq. Indian J Anaesth 2014; 58(4): 416 – 422. PMCID: PMC4155286
- Ham W et al. Pressure Ulcers From Spinal Immobilization in Trauma Patients: A Systematic Review. J Trauma Acute Care Surg 2014; 76(4): 1131 – 41. PMID: 24662882
- March J et al. Changes In Physical Examination Caused by Use of Spinal Immobilization. Prehosp Emerg Care 2002; 6(4): 421 – 4. PMID: 12385610
- Totten VY et al. Respiratory Effects of Spinal Immobilization. Prehosp Emerg Care 1999; 3(4): 347 – 52. PMID: 10534038
- Mobbs RJ et al. Effect of Cervical Hard Collar on Intracranial Pressure After Head Injury. ANZ J Surg 2002; 72(6): 389 – 91. PMID: 12121154
- Carpenter CR et al. Brain natriuretic Peptide in the Evaluation of Emergency Department Dyspnea: Is there a Role? JEM 2012. PMID: 22123173
- Steinhart BD et al. A Randomized control Trial Using a Validated Prediction Model for Diagnosing Acute Heart Failure in Undifferentiated Dyspneic Emergency Department Patients: Results of the GASP4Ar Study. Journal of Cardiac Failure 2017. PMID: 27565045
- Caputo N et al. EmergeNcy Department use of Apneic Oxygenation Versus Usual Care during Rapid Sequence Intubation: A Randomized controlled Trial (The ENDAO Trial). Acad Emerg Med 2017. PMID: 28791755
- Ebell MH et al. How Long Does a Cough Last? Comparing Patients’ Expectations with Data from a Systematic Review of the Literature. Ann Fam Med 2013. PMID: 23319500
- Kothari RU et al. The ABCs of Measuring Intracerebral hemorrhage Volumes. Stroke 1996. PMID: 8711791
- Sandhu AT et al. Cardiovascular Testing and Clinical Outcomes in Emergency department Patients with Chest Pain. PMID: 28654959
- Arakawa H et al. Does Pulse Oximetry Accurately monitor a Patient’s Ventilation During Sedated Endoscopy Under Oxygen Supplementation? Singapore Med 2013. PMID: 23624448
- Khandelwal N et al. Head-Elevated Patient Positioning Decreases Complications of Emergent Tracheal Intubation in the Ward and Intensive Care Unit. Anesth Analg 2016. PMID: 26866753
Post Peer Reviewed By:Anand Swaminathan, MD (Twitter: @EMSwami)
The post Clinical Pearls from ACEP 2018 – San Diego, CA appeared first on REBEL EM - Emergency Medicine Blog.
