
 On Feb 21st, a patient by the name of Aldo, a 72-year-old male, came to our ED with fever and progressive dyspnea. In addition, his chest x-ray showed an interstitial pattern.
On Feb 21st, a patient by the name of Aldo, a 72-year-old male, came to our ED with fever and progressive dyspnea. In addition, his chest x-ray showed an interstitial pattern.
It was on this day that COVID19 had arrived in our emergency department…
In this post we will describe how we responded to the COVID19 challenge, the impressive number of patients seen in just a few days’ time and some suggestions to prepare your emergency department for the future.
Our Hospital System:
We are a level 1 trauma center, the only pediatric trauma center for 10 million people in our region. We are also the referral center for stroke, STEMI, ECMO, and have the only neurosurgery availability of the province. We see about 100,000 patients per year. The Bergamo province accounts for roughly 1.2 million people.
ED Organization Before the Epidemic:
- 1 shock room (6 beds)
- 1 intermediate acuity area (7 rooms for evaluation; 2 waiting rooms. Named BOX)
- 1 low acuity area (1 room for evaluation; 1 waiting room. Named Vertical)
- 1 isolation room (2 beds)
- Observation unit (10 beds)
- Acute medicine ward (11 + 6 beds)
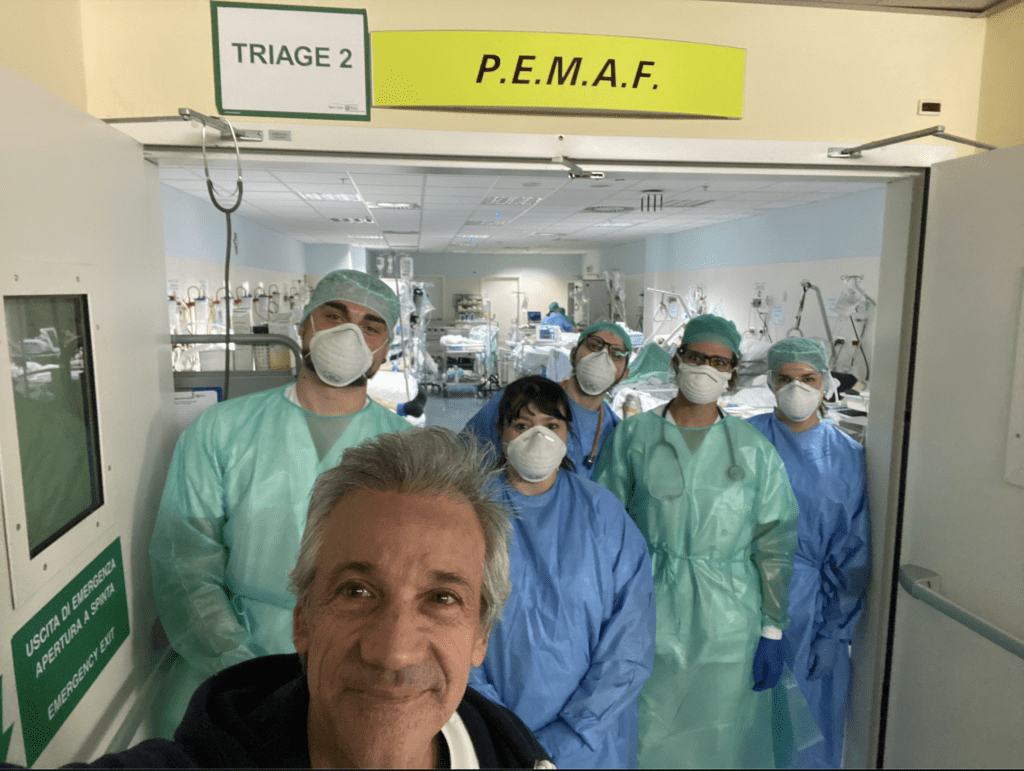
- 1 empty room dedicated to mass casualty events (named PEMAF, 24 oxygen sources)
- Ortho ED (1 evaluation room, 1 waiting room)
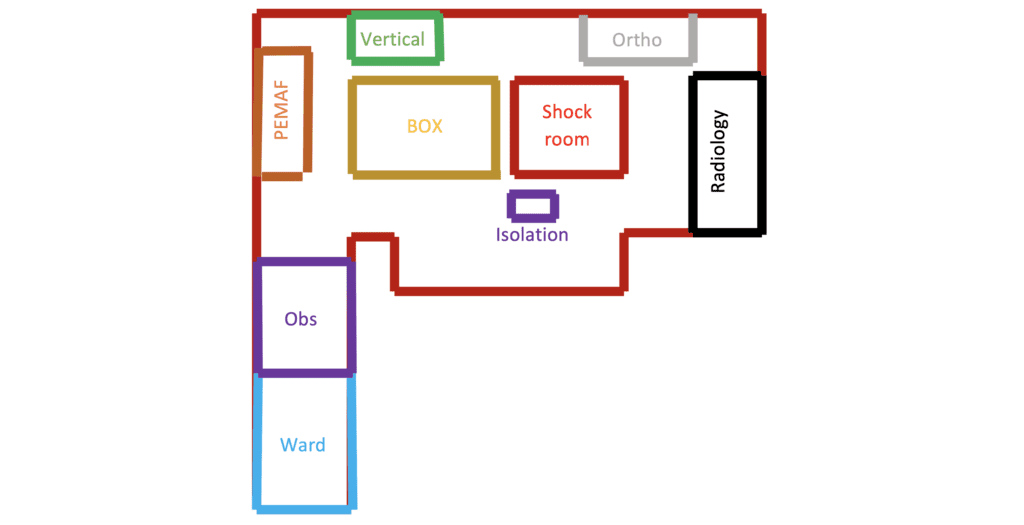
Figure 1: Organization of the ED Before the Epidemic
ED Physician Shifts Before the Epidemic:
- 26 total physicians
- 9 physicians worked shifts from 8am – 2pm
- 9 physicians worked shifts from 2pm – 8pm
- 3 physicians worked shifts form 8pm – 8am
ED Organization After the Bergamo Outbreak:
On 02/21, following the Italian (Codogno) outbreak, we created 2 different pathways: a “clean” pathway and a “dirty” pathway. The “dirty” pathway initially started with patients complaining of respiratory symptoms and/or a body temperature of >37.5C coming from suspected areas (The Lodi Province or China). The “clean” pathway was used for the evaluation of all other patients. Initially, the “dirty” pathway used 1 low acuity room plus 1 waiting room. After about a week (from 02/21) the volume of patients with respiratory complaints increased so much that we had to change the organization of the ED to all patients presenting with any respiratory symptoms and/or a temperature of >37.5 being evaluated in the “dirty” area (regardless of travel from suspected areas) and this area was extended to most of the ED.
The emergency department was then organized according to the severity of acute respiratory failure following the model developed by our EM colleague Stefano Paglia in Lodi, the first Italian hospital that faced the outbreak.
- 1 shock room (6 beds) converted to COVID Intubated room (Dedicated to intubated patients)
- PEMAF 16 beds, 24 oxygen sources was converted to an intermediate area (Dedicated to patients requiring NIV)
- 1 intermediate acuity area (7 rooms for evaluation; 2 waiting rooms) converted to a COVID Horizontal room (Cohort isolation; Dedicated to the evaluation of new patients)
- Observation unit (10 beds) & Acute medicine ward (11+6 beds) was converted to a COVID Horizontal area (Dedicated to patients needing oxygen and waiting for admission)
- 1 low acuity (1 box; 1 waiting room) converted to COVID Vertical room (Dedicated to patients not requiring oxygen)
- 1 isolation room (2 beds) was used for patients needing oxygen waiting for admission
- Ortho Room converted to the “Clean” pathway (Dedicated to patients without respiratory symptoms)
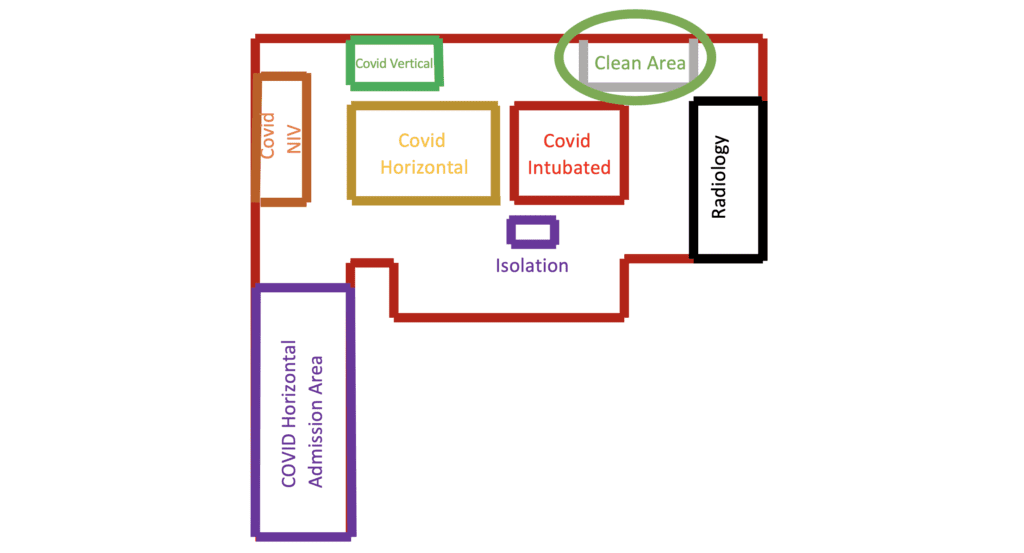
Figure 2: Organization of the ED after the Bergamo Outbreak
We also changed our shift organization, adding 1 physician on night shift and 1 physician on call during the day. We also reduced the night shift length to 10 hours.
Physician Schedule Re-Organized:
- 8 physicians 7am – 2pm
- 8 physicians 2pm – 9pm
- 4 physicians 9pm – 7am
Appropriate PPE is essential during this epidemic as evidenced by the fact on 02/24 we started to lose medical resources:
- 02/24 1st physician in quarantine (Didn’t come back until 03/02 after a negative nasal swab)
- 03/07 1st physician ill
- 03/09 2nd physician ill
- 03/10 3rd physician ill (Didn’t come back until 03/15)
- 03/17 4th physician ill
Hospital Organization:
- We work in an 880-bed hospital, with 80 intensive care beds
- At the start of Chinese epidemic, the infectious disease ward was dedicated to suspected/confirmed cases by increasing its beds from 24 to 48.
- On 02/21, following the Italian outbreak, we created the first 8 COVID beds for critically ill patients in the ICU
- We gradually opened new wards and new intensive care beds dedicated to COVID positive patients
- After the 02/29 Bergamo outbreak we now have 80 ICU beds dedicated to mechanically ventilated COVID patients, 12 beds dedicated to non-invasive ventilated patients managed by pulmonologists, and about 400 regular ward beds dedicated to COVID patients needing oxygen or Helmet CPAP (coordinated by pulmonologists or anesthesiologists)
Patient Population:
We had a sudden increase in patients suspected of having COVID infection from 8 patients on 02/22 to a maximum of 80 patients on 03/06.
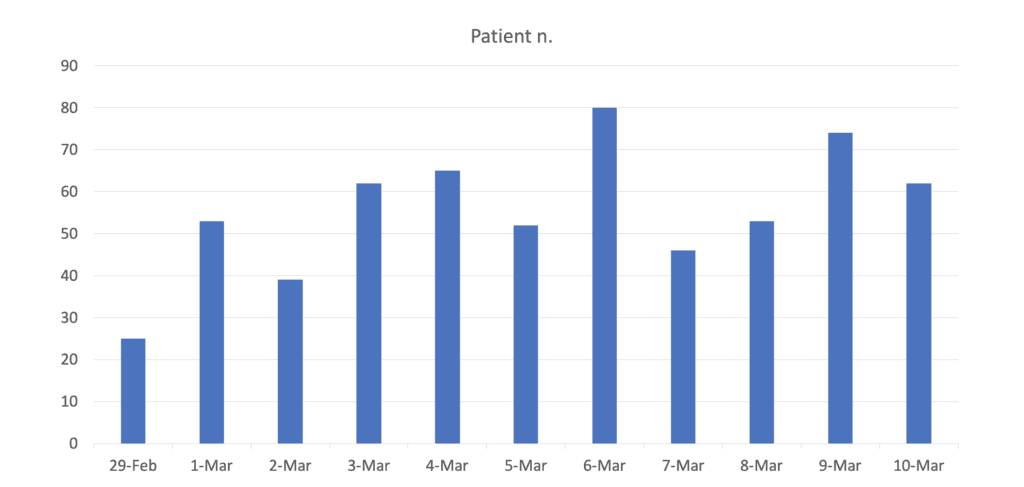
Graph 1: Number of Patients Presenting with Any Symptoms Suspected for COVID Infection
We observed 4 phases of ED presentation. The first patients presented with high airway symptoms, most of the time not needing admission, while in the next few days we started to see patients with persisting fever, followed by lower airway symptoms, needing oxygen and, in many cases, ventilatory support, while in the last days we are observing mainly pneumonia patients with a shift of age under 60 years of age.
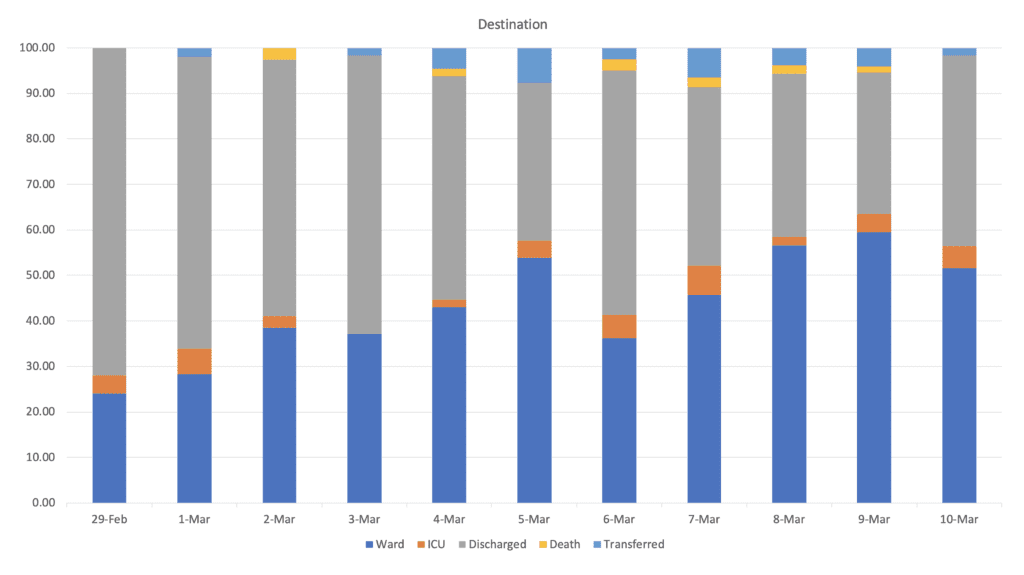
Graph 2. Number of Patients Admitted and Discharged from the ED per Day
During the first peak of the COVID presentations (March 6) we ended up with 105 patients in the ED, most with high O2 demand, as the ICU’s were always full, but new beds were being created every day. We used helmet CPAP on all patients with a pO2 <60 mmHg or a respiratory rate >30/min on 15 L/min non-rebreather masks, then shifted to non-invasive ventilation in patients with persistent respiratory distress and finally intubated patients non-responsive to non-invasive ventilation.
Based on our data, from 02/29 to 03/10, 31% of the patients being admitted needed some form of ventilatory support (helmet CPAP 81%, NIV 7%, IMV 12%). Within them 18% had mild ARDS, 51% moderate ARDS and 31% with severe ARDS.
The last key factors are logistics and supply. The risk of running out of PPE, oxygen tanks and CPAP equipment is very high. For instance, the maximum O2 supply at our hospital is around 8,000 L/min Currently, we are using more than 7,000 L/min.
The impressive number of patients with pneumonia, the high proportion of severe cases and the long recovery phase poses a unique challenge to our health system.
Our experience suggests that with preparation, reorganization of both the ED and the hospital, the massive COVID19 outbreak is manageable, but the most important aspect is staff health, in terms of physical protection (PPE) but especially emotional assistance, since the burden is very high and prolonged.
If you remember nothing else from this post…
- The COVID-19 epidemic led to a massive amount of severely ill patients presenting to the ED in a short period of time
- The needs of the patients are disproportionate to the resources of any unprepared health system, thus, preparedness of health systems are fundamental
- Continuous assessment of patient flow and the ability to quickly change the organization of the hospital/ED accordingly is a key element to face this epidemic surge
Guest Post By:

Andrea Duca
Attending Emergency Physician
Emergency Department, Ospedale papa Giovanni XXIII of Bergamo
Living in Milano
Twitter: @andreaduca00
Roberto Cosentini
Centro EAS Director – ASST Papa Giovanni XXIII – Bergamo, Italy
ASST Papa Giovanni XXIII – Bergamo, Italy
Milan, Italy
Twitter: @rob_cosentini
Additional REBEL EM Content – Critical Care Utilization for COVID-19 Outbreak in Lombardy, Italy [1]
[embedyt] https://www.youtube.com/watch?v=TKS1pahoPRU[/embedyt]
Coronavirus in Italy – A Report from the Front Lines from March 13th, 2020 (Video Time 36:49)
On Feb 20th, 2020 the 1st patient with COVID-19 was admitted to the ICU in Lombardy Italy. In the next 24 hours the number of reported positive cases increased to 36. This is important because this meant two things: the illness was present in the community and the number of patients requiring ICU level care was only going to increase. In Lombardy, the total ICU capacity was ≈720 ICU beds (2.9% of total hospital beds at a total of 74 hospitals). Most of their ICUs function at 85 to 90% capacity in the winter months. They needed to increase their surge ICU capacity and achieved this by (Assuming a 5% ICU admission rate, it would not be feasible to care for all critically ill patients in the ICU) creating 15 first-responder hub hospitals that had infectious disease expertise or had ECMO available. These hospitals were tasked with:
- Creating ICUs for COVID-19 patients (areas separated from the rest of the ICU beds to minimize risk of in-hospital transmission)
- Having a triage area where patients could receive mechanical ventilation if necessary in every hospital with suspected COVID-19, pending the final result of diagnostic tests
- Establishing local protocols for triage of patients with respiratory symptoms to have rapid testing
- Ensure adequate PPE for health care personnel
- All non-urgent/elective procedures were cancelled
Overall in the first 18 days the network created 482 additional ICU beds. As predicted, there was an increase in ICU admissions from day 1 to 14 (ICU admissions with COVID-19 was 12% and 16% of all hospitalized patients with COVID-19). These rates of admission and ICU useage are far higher than what was seen in China (i.e. 5%). A forecast using a linear model predicted that 829 ICU admissions could occur by March 20th, 2020, which means there may potentially not be enough ICU beds.
The Numbers in Italy Up to March 15th, 2020
This Infographic shows the most recent statistics emerging from #Italy regarding the country’s experience with #COVID19 https://t.co/QTwrRgFoRE
— JAMA (@JAMA_current) March 17, 2020
Lets Learn from the Tragedy in Lombardy:
- Strong containment measures are the only realistic option to avoid the total collapse of health systems. This includes social distancing including cancelling gatherings and travel. This is the only way to contain the spread of infection and allow resources to be developed for this time-dependent disease (Flattening the curve of infection)
- Outbreaks can lead to significant increases in the need for ED/ICU beds and simultaneously reduce available beds in a hospital system. Hospital administration should have a surge plan and the ability to augment ED/ICU bed capacity, which can be as simple as transforming general wards into ICUs
- Increase laboratory capacity to test for SARS-CoV-2. In Italy the laboratory capacity reached saturation very early which can have other downstream effects in making timely accurate diagnoses and allocating patients appropriately
- Protect healthcare personnel with education and having adequate personal protective equipment and training in DONning/DOFFing procedures through mandatory simulation training
Retrospective case series of 1591 consecutive patients with COVID-19 requiring ICU level of care in Lombardy region of Italy [2]
- HTN most common comorbidity 509/1043 (49%)
- 2nd most common comorbidity was cardiovascular dz 223/1063 (21%)
- 1287/1300 (99%) of patients required respiratory support
- 1150/1591 (88%) required endotracheal intubation
- 137/1591 (11%) required NIV
- ICU mortality = 405/1581 (26%)
- Higher rate of intubation may be due to severity of hypoxia (Median PaO2/FiO2 = 160) requiring high levels PEEP
- Many patients managed with NIV were able to be managed outside the ICU and were not included in this report
References:
- Grasselli G et al. Critical Care Utilization for the COVID-19 Outbreak in Lombardy, Italy: Early Experience and Forecast During an Emergency Response. JAMA 2020. [Epub Ahead of Print]
- Grasselli G et al. Baseline Characteristics of 1591 Patients Infected with SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA 2020. PMID: 32250385
For More on This Topic Checkout:
- REBEL EM: COVID-19 – The Novel Coronavirus 2019
- St. Emlyn’s: Podcast from Italy with Roberto Cosentini, MD
- EMplify: COVID-19 Update – An Interview with Andrea Duca, MD
- St. Emlyn’s: COVID 19 Preparations in Virchester
- The Atlantic: The Extraordinary Decisions Facing Italian Doctors
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami) and Mizuho Morrison, DO (Twitter: mizuhomorrison)
The post COVID-19: A Powerful Message from Italy appeared first on REBEL EM - Emergency Medicine Blog.

