
 Background: Patients with COVID-19 are at a high risk for the development of venous thromboembolic disease [Link is HERE]. Alveolar capillary microthrombi appear to be 9x more prevalent in patients with COVID-19 compared to H1N1. As a result, enhanced-dose anticoagulation has been recommended and practiced by many caring for these patients. However, the effectiveness and safety of therapeutic-dose anticoagulation in patient-oriented outcomes in COVID-19 have remained uncertain. Additionally, it is unclear which group of COVID patients (critically ill, admitted but not critically ill, stable for discharge home) stands to benefit from higher anticoagulation doses if any.
Background: Patients with COVID-19 are at a high risk for the development of venous thromboembolic disease [Link is HERE]. Alveolar capillary microthrombi appear to be 9x more prevalent in patients with COVID-19 compared to H1N1. As a result, enhanced-dose anticoagulation has been recommended and practiced by many caring for these patients. However, the effectiveness and safety of therapeutic-dose anticoagulation in patient-oriented outcomes in COVID-19 have remained uncertain. Additionally, it is unclear which group of COVID patients (critically ill, admitted but not critically ill, stable for discharge home) stands to benefit from higher anticoagulation doses if any.
Paper #1: The REMAP-CAP, ACTIV-4a, and ATTACC Investigators. Therapeutic Anticoagulation in Critically Ill Patients with COVID-19. NEJM 2021. [Epub Ahead of Print]
Paper #2: The ATTACC, ACTIV-4a, and REMAP-CAP Investigators. Therapeutic Anticoagulation in Noncritically Ill Patients with COVID-19. NEJM 2021. [Epub Ahead of Print]
What They Did (The protocols, outcomes, exclusion criteria, and dosing regimens used were the same in both trials of severe and moderate COVID-19 patients)
- International, open-label, adaptive, multiplatform, randomized clinical trial of critically ill patients with severe and moderate COVID-19
- Three platforms combined efforts:
- Randomized, Embedded, Multifactorial Adaptive Platform Trial for Community-Acquired Pneumonia (REMAP-CAP)
- Adaptive, Randomized Controlled Platform Trial of the Safety and Efficacy of Antithrombotic Strategies in Hospitalized Adults with COVID-19 (ACTIV-4a)
- Antithrombotic Therapy to Ameliorate Complications of COVID-19 (ATTACC)
- Patients were randomized to one of two arms (unfractionated or low molecular weight heparin):
- Therapeutic Anticoagulation (TA): Full dose anticoagulation
- Prophylactic Anticoagulation (PA): Prophylactic or intermediate dose anticoagulation
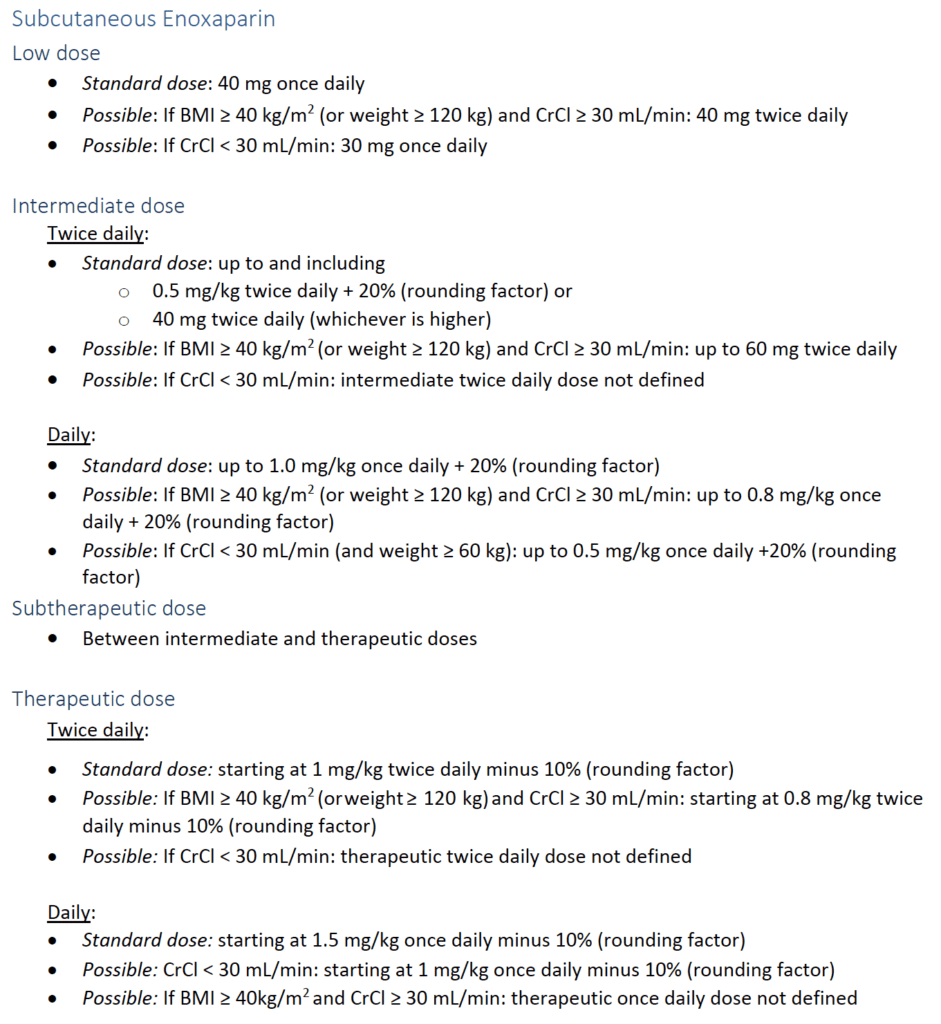
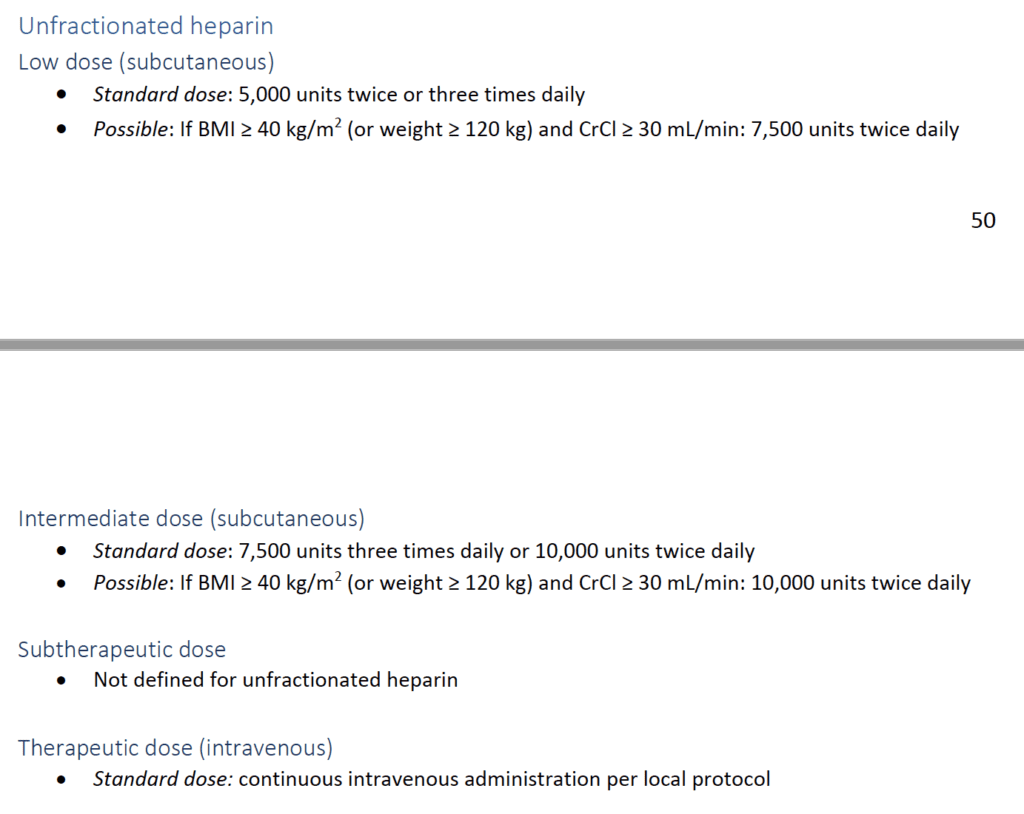
Dosing Regimens Used
Outcomes:
-
Primary: Organ support-free days at 21 days
- Evaluated on an ordinal scale that combined in hospital death (assigned a value of -1) and the number of days free of cardiovascular (vasopressors and inotropes) or respiratory organ support (HFNC, NIV, invasive mechanical ventilation, ECMO) in patients who survived to hospital discharge
- A higher number of organ support-free days indicates a better outcome
-
Secondary:
- Survival to hospital discharge
- Major thrombotic events or death (composite of MI, PE, ischemic stroke, systemic arteria embolism, or in-hospital death)
-
Safety:
- Major bleeding
Exclusion:
- Admitted to ICU with COVID-19 for ≥48hrs (REMAP-CAP) or for ≥72hrs (ACTIV-4a and ATTACC) before randomization
- Imminent risk for death
- Comfort care
- High risk for bleeding
- Receiving dual antiplatelet therapy
- Separate clinical indication for therapeutic dose anticoagulation
- History of heparin sensitivity (including heparin induced thrombocytopenia)
Strengths:
- Asks a clinically important question
- Combined 3 platforms across 5 continents to answer the question
- Baseline characteristics of the patients were similar between groups
Limitations:
- Open-label design can introduce some bias in evaluation of thrombotic events
- No consecutive enrollment could create a selection bias
- Majority of patients enrolled with severe disease were from the UK which may be a different population than seen in other hospital systems
- No separation of prophylactic dose vs intermediate dose anticoagulation to further guide care
- In the non-critically ill patients there were protocol violations where those randomized to full dose anticoagulation actually got intermediate dose anticoagulation
- Definition of non-critically ill is subjective. For 2 of the platforms this essentially meant not in the ICU. This completely depends on available resources. This was done correctly in ACTIV-4a, in which the investigators found that ICU-level care was challenging to define during the pandemic. They chose to define critically ill as patients who required refeipt of organ support, regardless of hospital setting
Critically Ill COVID-19 Patients
Clinical Question: Does therapeutic anticoagulation improve organ support-free days compared to prophylactic anticoagulation in adult patients admitted to the hospital with severe (Critically Ill) COVID-19?
Inclusion:
- Adult patients hospitalized for severe COVID-19
- Severe = ICU level respiratory or cardiovascular organ support (oxygen through HFNC, NIV, invasive mechanical ventilation, ECMO, vasopressors or inotropes)
Results:
- Data available for 1098 patients for the primary outcome
- Majority of patients (929 of 1103) were enrolled through REMAP-CAP
- In the PA arm:
- 41% received prophylactic dose anticoagulation
- 51% received intermediate dose anticoagulation
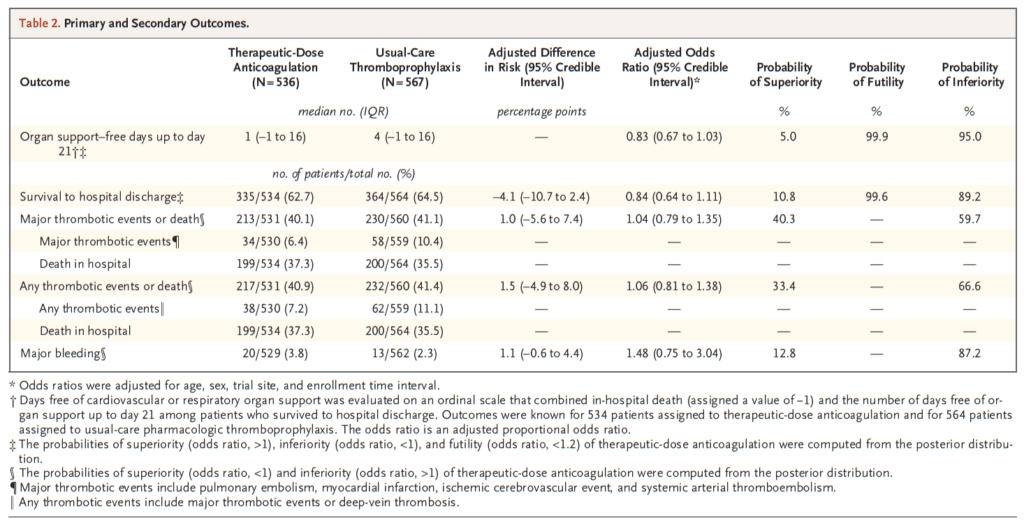
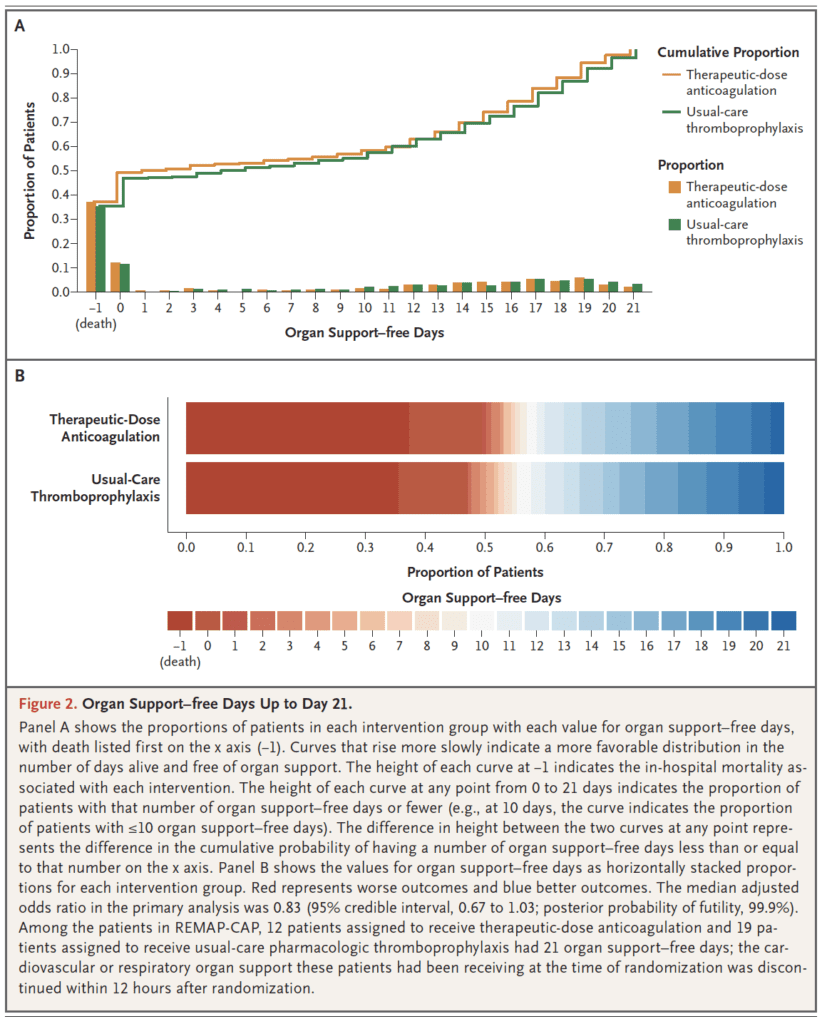
- Major Bleeding:
- TA: 3.8%
- PA: 2.3%
Discussion:
- In critically ill patients with confirmed COVID-19 therapeutic-dose anticoagulation did not increase the probability of survival to hospital discharge or the number of days free of cardiovascular or respiratory organ support compared to usual-care pharmacologic thromboprophylaxis
- The anticoagulation regimen used may be dependent on the timing of the initiation in relation to the disease course. For example, it is possible that initiation of therapeutic-dose anticoagulation after severe COVID-19 has developed may be too late to alter the consequences of the disease
- It is important to also point out, that although major bleeding was more likely with therapeutic-dose anticoagulation compared to usual-care thromboprophylaxis, the numbers were still low (3.8%). However with no benefit shown, there is no reason to risk this harm, no matter how low the incidence
Author Conclusion: “In critically ill patients with COVID-19, an initial strategy of therapeutic-dose anticoagulation with heparin did not result in a greater probability of survival to hospital discharge or a greater number of days free of cardiovascular or respiratory organ support than did usual-care pharmacologic thromboprophylaxis.”
Non-Critically Ill COVID-19 Patients
Clinical Question: Does therapeutic anticoagulation improve organ support-free days compared to prophylactic anticoagulation in adult patients admitted to the hospital with moderate (Non-Critically Ill) COVID-19?
Inclusion:
- Adult patients who were not critically ill with COVID-19
- Defined as an absence of critical care-level organ support at enrollment
Results:
- 2219 patients in the final analysis
- Of the patients receiving TA, 94.7% received a LMWH
- In the PA arm:
- 7% received prophylactic dose anticoagulation
- 5% received intermediate dose anticoagulation
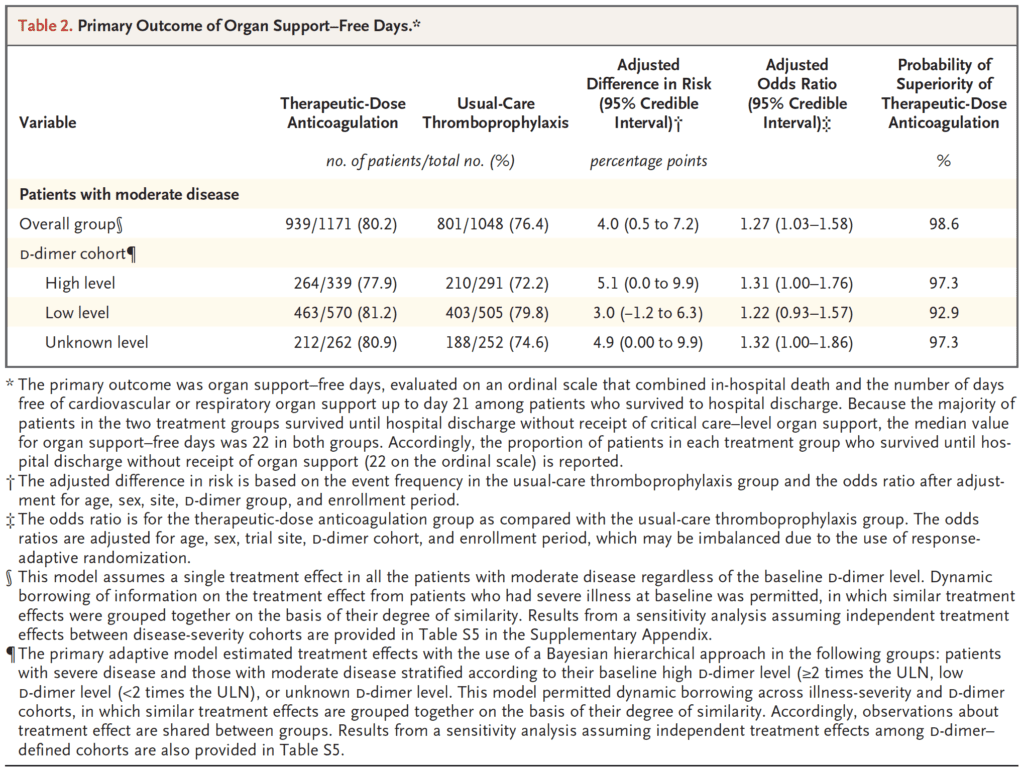
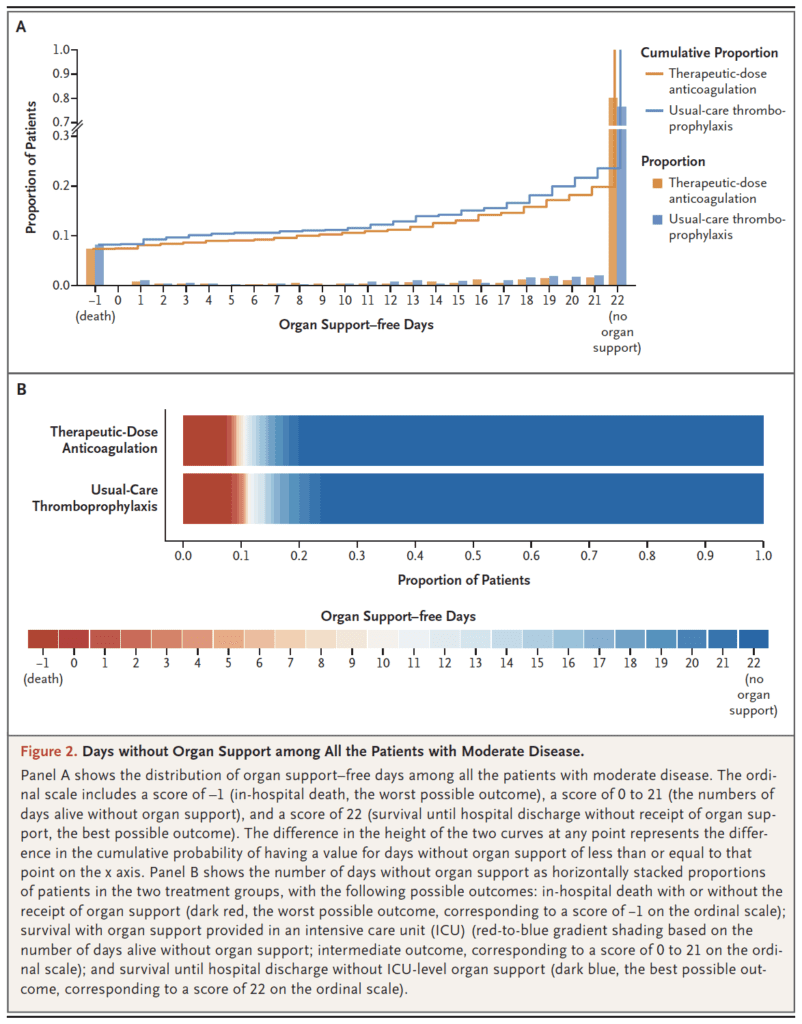
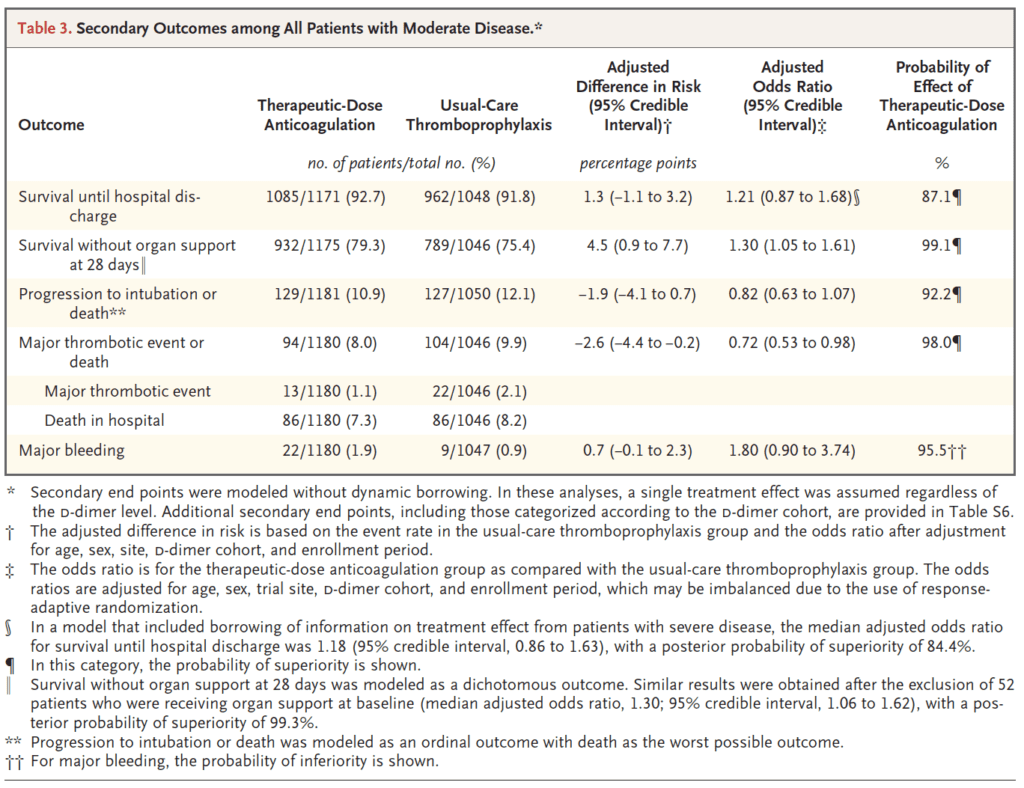
- KEY RESULT: 4% difference in primary outcome, only 1% diff in death
- Major Bleeding:
- TA: 1.9%
- PA: 0.9%
Discussion:
- In non-critically ill hospitalized COVID-19 patients, therapeutic anticoagulation increased the probability of survival until hospital discharge with a reduced need for ICU-level organ support at 21 days compared with usual-care thromboprophylaxis
- Regardless of the d-dimer level, therapeutic anticoagulation was beneficial, although the benefit was more profound in patients with a d-dimer ≥2x the upper limit of normal
- For every 1000 hospitalized patients with moderate disease, an initial strategy of therapeutic-dose anticoagulation, compared to usual-care thromboprophylaxis could result in the survival of 40 additional patients until hospital discharge without organ support at the expense of 7 additional major bleeding events
- The major thought behind why we may see benefit in non-critically ill patients hospitalized with COVID-19 vs those who are critically ill is that therapeutic anticoagulation works through antithrombotic, anti-inflammatory, and potentially antiviral mechanisms earlier in the disease process before the cascade of inflammation, thrombosis, and organ injury result in advanced disease
Author Conclusion: “In noncritically ill patients with COVID-19, an initial strategy of therapeutic-dose anticoagulation with heparin increased the probability of survival to hospital discharge with reduced use of cardiovascular or respiratory organ support as compared with usual-care thromboprophylaxis.”
Clinical Take Home Point:
- In CRITICALLY ILL patients with COVID-19, an initial strategy of therapeutic-dose anticoagulation is not associated with a greater probability of survival to hospital discharge or a greater number of days free of cardiovascular or respiratory organ support vs usual-care pharmacologic thromboprophylaxis
- In NON-CRITICALLY ILL patients with COVID-19, an initial strategy of therapeutic-dose anticoagulation is associated with a greater probability of survival to hospital discharge or a greater number of days free of cardiovascular or respiratory organ support vs usual-care pharmacologic thromboprophylaxis
- In NON-CRITICALLY ILL patients with COVID-19, there is a clear signal of benefit, however with all the protocol violations and variable treatment arms it would still be reasonable to discuss with the inpatient team to help guide the decision (Although, in my practice and at my institution most patients who are not critically ill and don’t have contraindications, we have changed our protocols to full dose anticoagulation).
References:
- The REMAP-CAP, ACTIV-4a, and ATTACC Investigators. Therapeutic Anticoagulation in Critically Ill Patients with COVID-19. NEJM 2021. [Epub Ahead of Print]
- The ATTACC, ACTIV-4a, and REMAP-CAP Investigators. Therapeutic Anticoagulation in Noncritically Ill Patients with COVID-19. NEJM 2021. [Epub Ahead of Print]
For More on This Topic Checkout:
- Critical Care Reviews: mpRCT Anticoagulation Trial
- St. Emlyn’s Blog: Thromboprophylaxis for the Non ICU Hospitalised COVID-19 Patient
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)
The post COVID-19 and Anticoagulation: Full Dose or Prophylactic Dose? appeared first on REBEL EM - Emergency Medicine Blog.
