
 There continues to be a slew of publications coming out on a near daily basis in regard to COVID-19. Some publications will deserve their own posts and others can really be summarized in one or two paragraphs. In this post I will summarize 5 papers published in the past week, that I found interesting and each has a unique, but important message. None of these papers are very long, but there are some important aspects of each I felt tied into each other from a cardiovascular standpoint.
There continues to be a slew of publications coming out on a near daily basis in regard to COVID-19. Some publications will deserve their own posts and others can really be summarized in one or two paragraphs. In this post I will summarize 5 papers published in the past week, that I found interesting and each has a unique, but important message. None of these papers are very long, but there are some important aspects of each I felt tied into each other from a cardiovascular standpoint.
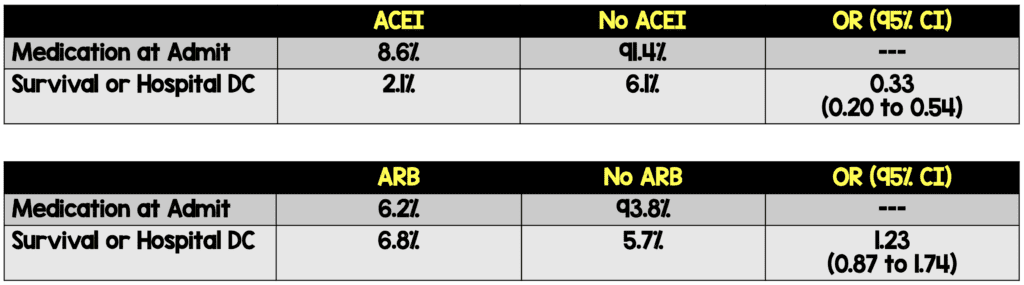
Mehra MR et al. Cardiovascular Disease, Drug Therapy, and Mortality in COVID-19. NEJM 2020 [1]:
- Evaluated the relationship between:
- Underlying cardiovascular disease and COVID-19 outcomes
- Cardiovascular drug therapy and mortality in COVID-19
- Data from 169 hospitals located in 11 countries across Asia, Europe, and North America were evaluated
- Only included data from patients who either died or were discharged alive (i.e. did not include patients still in the hospital receiving treatment)
- 8,910 patients completed their hospital course
- North America: 1536 patients (17.2%)
- Europe: 5755 patients (64.6%)
- Asia: 1619 patients (18.9%)
- Mortality (In patients with completed outcomes):
- Overall: 515/8910 (5.8%)
- ICU: 24.7%
- Non-ICU: 4.0%
- Independent predictors of in-hospital death:
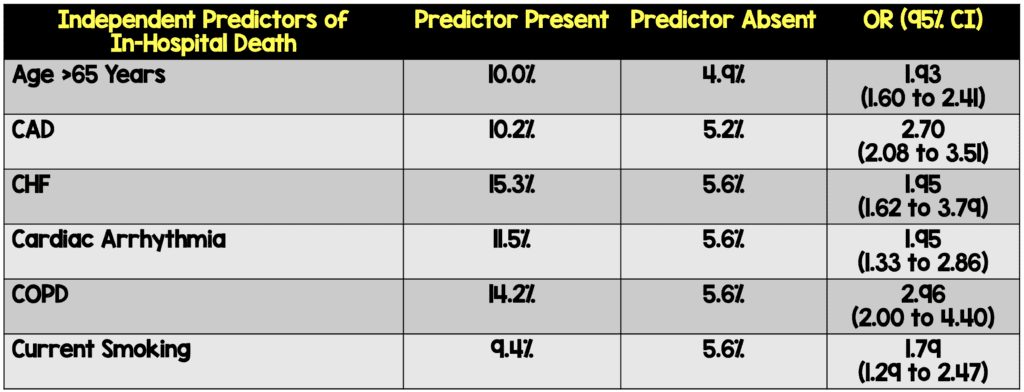
- Female sex, use of ACEI, and use of statins were associated with better chance of survival to hospital discharge
-
Bottom Line:
- Patients admitted to the hospital with a diagnosis of COVID-19 and underlying cardiovascular disease have an association with increased risk of in-hospital death. These patients will need close monitoring when admitted
- There was no association between patients being admitted with COVID-19 and taking ACEI or ARBs prior to admission with in-hospital death. This study also does not offer information on starting patients on ACEIs or statins who do not have an appropriate indication for these medications
Baldi E et al. Out-of-Hospital Cardiac Arrest During the COVID-19 Outbreak in Italy. NEJM 2020 [2]:
- Used the Lombardia Cardiac Arrest Registry (Lombardia CARe) to compare OHCA that occurred in 4 provinces in Italy during the 1st 40d of the COVID-19 outbreak and compared it to the OHCA cases that occurred during the same time period in 2019
- Observations:
- 58% increase in cardiac arrest cases (229 cases in 2019 and 362 cases in 2020)
- Sex and age of patients similar between 2019 and 2020, but in 2020…
- OHCA due to medical cause increased by 6.5%
- OHCA at home increased by 7.3%
- Unwitnessed OHCA increased by 11.3%
- Median time of EMS arrival 3min longer
- CPR from bystanders decreased by 15.6%
- Among patients in whom resuscitation was attempted by EMS, incidence of OHCA death increased by 14.9%
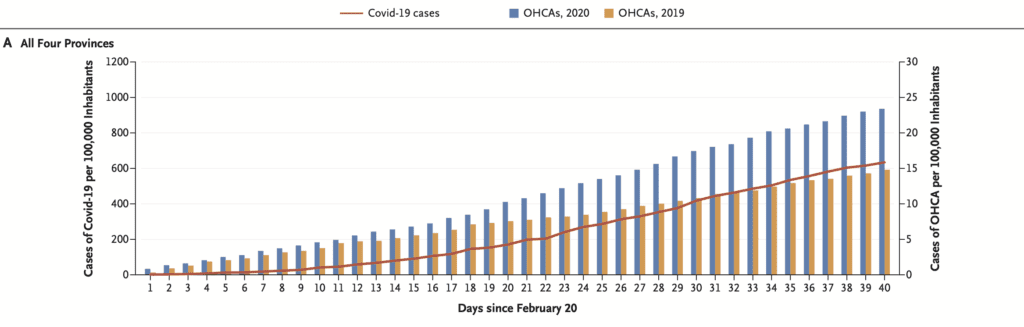
- 77% increase in OHCA cases were or suspected COVID-19 positive
- Bottom Line: There appears to be a correlation between increase in COVID-19 cases and OHCA. The increase in mortality may or may not be from COVID-19 itself, but from patients avoiding hospitals, fear of infection from COVID-19 and lower rates of bystander CPR.
De Filippo O et al. Reduced Rate of Hospital Admissions for ACS During COVID-19 Outbreak in Northern Italy. NEJM 2020 [5]:
- Multicenter, observational, retrospective study involving 15 centers in Northern Italy
- Evaluated the rate of hospital admissions for ACS during early days of the COVID-19 outbreak
- 2202 ACS patients included in the study
- During Lockdown: 547 patients
- Intra-Year Control Period (Dates from earlier in the same year): 899 patients
- Inter-Year Control Period (Same dates from previous year): 756 patients
- Primary Outcome: Overall rate of Hospital Admissions for ACS
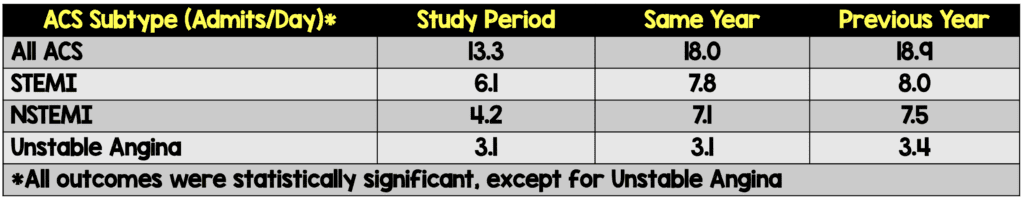
- Bottom Line: A significant decrease in ACS-related hospitalizations rates across several PCI capable centers in northern Italy was observed during the initial COVID-19 outbreak compared to two control periods. This also may explain the observation of increased mortality not explained by COVID-19 as some patients may have died from ACS without seeking medical attention. We need to drastically change our public health messaging and inform patient that if they think they are having an emergency, they should not delay care.
Mercuro NJ et al. Risk of QT Interval Prolongation Associated With Use of Hydroxychloroquine With or Without Concomitant Azithromycin Among Hospitalized Patients Testing Positive for Coronavirus Disease 2019 (COVID-19). JAMA Cardiology 2020 [3]:
- Single center, retrospective, observational, cohort study performed in Boston, MA of patients with COVID-19 pneumonia admitted to the hospital with at least 1d of Hydroxychloroquine with or without Azithromycin
- Main Outcome: Change in QT interval after receiving Hydroxychloroquine with or without Azithromycin
- Standard Dose Regimen: Hydroxychloroquine 400mg PO BID on day 1 then 400mg PO qD on days 2 through 5
- Patient Characteristics:
- Critically Ill (ICU admit): 30 patients (33%)
- Mechanically Ventilated 23 patients (26%)
- Acute Cardiac Injury: 25 patients (27.8%)
- Loop Diuretic in Hospital: 39 patients (43.4%)
- Hydroxychloroquine Alone: 90 patients
- Hydroxychloroquine with Azithromycin: 53 patients
- Critical Results:
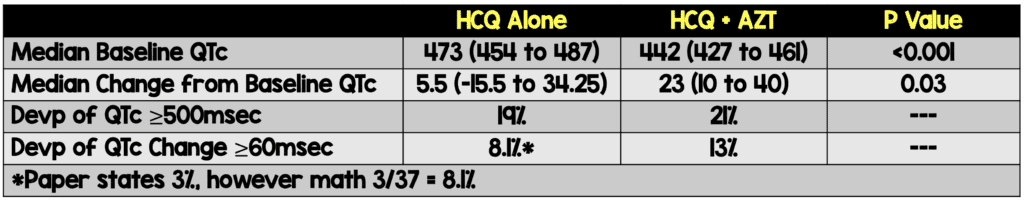
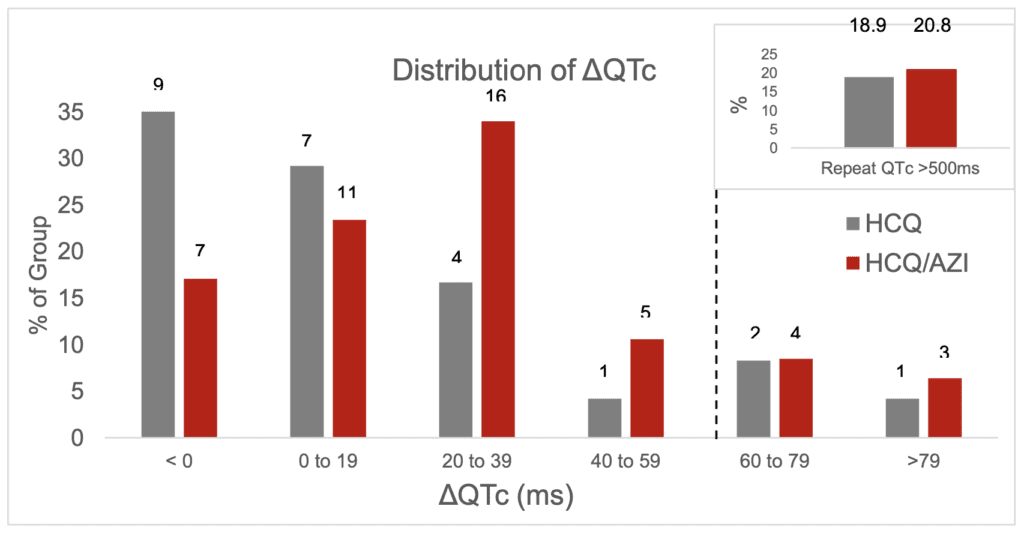
Specific Distribution of QTc Prolongation
- 10 patients had hydroxychloroquine discontinued early because of potential adverse drug events (i.e. intractable nausea, hypoglycemia, and 1 case of torsades de pointes)
- Repeated Nasopharyngeal PCR Testing (21 total patients):
- Median 3 days (1 – 6.5)
- Hydroxychloroquine Alone: 0/8 (0%)
- Hydroxychloroquine with Azithromycin: 1/13 (7.7%)
-
IMPORTANT NOTES:
- True degree of QTc prolongation most likely underestimated, due to short period of follow up, 45 patients still being hospitalized, and 19 patients without follow-up ECGs
- Patients with baseline prolonged QTc intervals were not given hydroxychloroquine
- Bottom Line: In patients with COVID-19 pneumonia admitted at a single hospital in Boston, MA, over a 4-week period, there was a high risk of QTc prolongation and concurrent treatment with azithromycin was associated with an even greater change in QTc. If using these medications baseline risk assessment, with frequent QTc monitoring and strict cutoffs should be applied for therapy cessation.
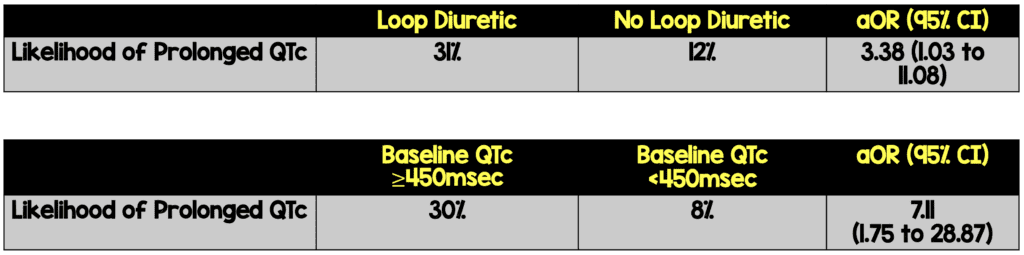
Bessiere F et al. Assessment of QT Intervals in a Case Series of Patients With Coronavirus Disease 2019 (COVID-19) Infection Combination With Azithromycin in an Intensive Care Unit. JAMA Cardiology 2020 [4]:
- Retrospective, observational trial of consecutive patients with COVID-19 pneumonia admitted to the ICU who received Hydroxychloroquine 200mg PO BID x10d with or without Azithromycin 250mg PO qD x5d
- Prolonged QTc was defined as increase in QTc interval of >60msec from baseline OR a QTc ≥500msec
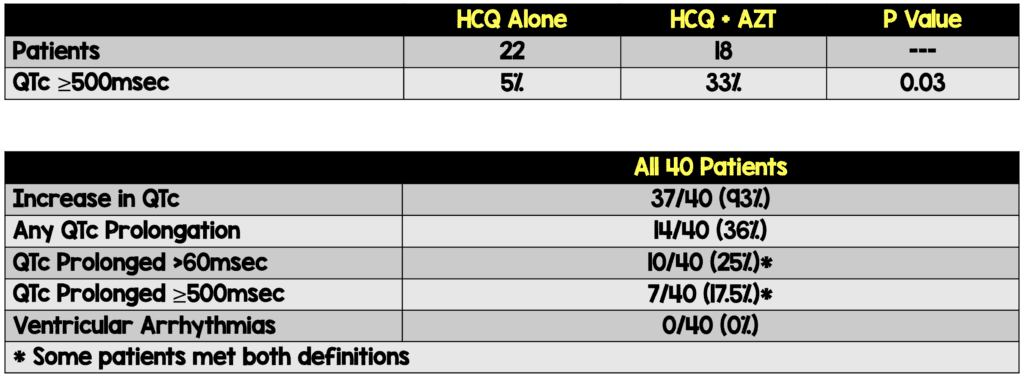
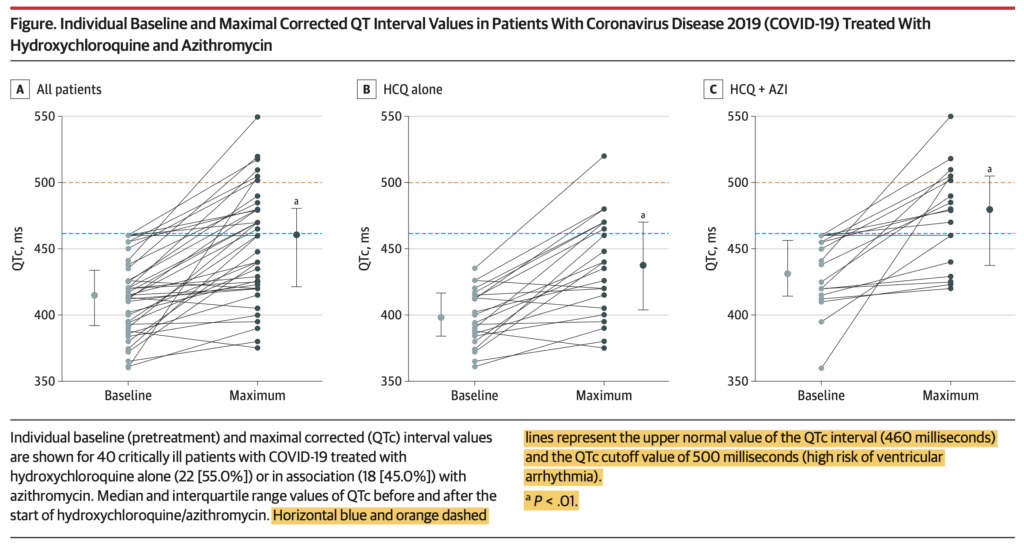
Individual Patient Level QTc Prolongation
-
IMPORTANT NOTE: Treatment was stopped before completion for 7 (17.5%) of patients after ECG abnormalities and in 10 (25% for acute renal failure which is most likely why we didn’t see ventricular arrhythmias in this report
- Close monitoring of patients with daily ECGs and laboratory tests led to an interruption of hydroxychloroquine and azithromycin for 17/40 (42.5%) which may have averted further complications
- Bottom Line: This study confirms the safety concerns already documented about the use of hydroxychloroquine with or without azithromycin for patients with COVID-19.
Clinical Bottom Line:
- Patients admitted to the hospital with a diagnosis of COVID-19 and underlying cardiovascular disease need close monitoring when admitted
- There does NOT appear to be an association between patients being admitted with COVID-19 and taking ACEI or ARBs prior to admission with in-hospital death
- There appears to be a correlation between an increase in COVID-19 cases and OHCA. The increase in mortality may or may not be from COVID-19 itself, but from patients not coming to the hospital, fear of infection from COVID-19 and lower rates of bystander CPR
- There needs to be a drastic shift in our public health messaging informing patient that if they think they are having an emergency, they should not delay care
- If using hydroxychloroquine with or without azithromycin for treatment of COVID-19 pneumonia, this should be done in the setting of a RCT, baseline risk assessment, with frequent QTc monitoring and strict cutoffs should be applied for therapy cessation
References:
- Mehra MR et al. Cardiovascular Disease, Drug Therapy, and Mortality in COVID-19. NEJM 2020. [Epub Ahead of Print]
- Baldi E et al. Out-of-Hospital Cardiac Arrest During the COVID-19 Outbreak in Italy. NEJM 2020. [Epub Ahead of Print]
- Mercuro NJ et al. Risk of QT Interval Prolongation Associated With Use of Hydroxychloroquine With or Without Concomitant Azithromycin Among Hospitalized Patients Testing Positive for Coronavirus Disease 2019 (COVID-19). JAMA Cardiology 2020. [Epub Ahead of Print]
- Bessiere F et al. Assessment of QT Intervals in a Case Series of Patients With Coronavirus Disease 2019 (COVID-19) Infection Combination With Azithromycin in an Intensive Care Unit. JAMA Cardiology 2020. [Epub Ahead of Print]
- De Filippo O et al. Reduced Rate of Hospital Admissions for ACS During COVID-19 Outbreak in Northern Italy. NEJM 2020. [Epub Ahead of Print]
For More on This Topic Checkout:
- REBEL EM: COVID-19 – Cardiovascular Considerations
- REBEL EM: COVID-19 – Clinical/Therapeutic Staging Proposal and Treatment
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)
The post COVID-19 Cardiovascular Literature Update appeared first on REBEL EM - Emergency Medicine Blog.

