The Novel Coronavirus 2019, was first reported on in Wuhan, China in late December 2019. The outbreak was declared a public health emergency of international concern in January 2020 and on March 11th, 2020, the outbreak was declared a global pandemic. The spread of this virus is now global with lots of media attention. The virus has been named SARS-CoV-2 and the disease it causes has become known as coronavirus disease 2019 (COVID-19). This new outbreak has been producing lots of hysteria and false truths being spread, however the data surrounding the biology, epidemiology, and clinical characteristics are growing daily, making this a moving target. This post will serve as a summary of protecting our families and patient disposition for COVID-19.
The Novel Coronavirus 2019, was first reported on in Wuhan, China in late December 2019. The outbreak was declared a public health emergency of international concern in January 2020 and on March 11th, 2020, the outbreak was declared a global pandemic. The spread of this virus is now global with lots of media attention. The virus has been named SARS-CoV-2 and the disease it causes has become known as coronavirus disease 2019 (COVID-19). This new outbreak has been producing lots of hysteria and false truths being spread, however the data surrounding the biology, epidemiology, and clinical characteristics are growing daily, making this a moving target. This post will serve as a summary of protecting our families and patient disposition for COVID-19.
To go back to the main post, click on the image below…
Protecting Our Families
While we all accept increased risks as part of our chosen profession, we all worry about family transmission. Caring for infected patients represents substantial exposure for all healthcare providers. Some conversations to start having with your hospital system and family:
- Priority testing, vaccination and treatment when available for you and your family
- Have discussions at home about separating living spaces and bathrooms to hopefully minimize risk
- Having one entrance of arrival where clothing is removed immediately before entering the house
- Leave work shoes outside of house (i.e. in garage)
- Another option would be going to work in personal clothing and switching to scrubs at work and showering and changing back to personal clothing on the return home
- Wipe down your cell phone before going home
- Hospital housing provided when working a run of shifts
My family is my wellness (also, logistically, I need to see them and
the baby) and during #COVID19 I need to keep them safe.
Here's my method to decontaminating myself after a shift pic.twitter.com/FvwH8wZSQS— Lauren Westafer, DO MPH MS (@LWestafer) March 14, 2020
New pre/post shift DECON routine:
-change of scrubs
-BYOPPE
– lose the(gets in the way anyway)
-Saran wrap
-plastic bag all hospital garments
– bleach shoes once home
-hot shower
Who knew my car would become the the Ghostbusters
#Covid_19 #EmergencyMedicine pic.twitter.com/ubBTfVdyJl
— Mizuho M. Morrison (@mizuhomorrison) March 21, 2020
Healthcare workers worry about keeping our families safe. #Covid_19 #DontBringItHome info sheet for #Anesthesiology staff.
Adapted for our dept by @morganckelly #Covid_19nz #Anaesthesia pic.twitter.com/pK3lS3aeBH
— Dr Nav Sidhu (@DrNavSidhu) March 24, 2020
Patient Disposition
- Not all persons under investigation require admission.
- The decision to admit vs discharge home for home isolation should be made on a case-by-case basis with your local health department (This is a multifactorial decision depending first on the severity of the patients clinical presentation)
- If mild symptoms a patient may qualify for home isolation depending on their ability to 1) comply with health department monitoring, and 2) remain home to minimize any risk of transmission to the general public
[embedyt] https://www.youtube.com/watch?v=CcnT2q4locU[/embedyt]
COVID-19 Discharge Video via Sketchy EBM (Video Time: 8:36)
-
Two Discharge Algorithms (Both Non-Validated)
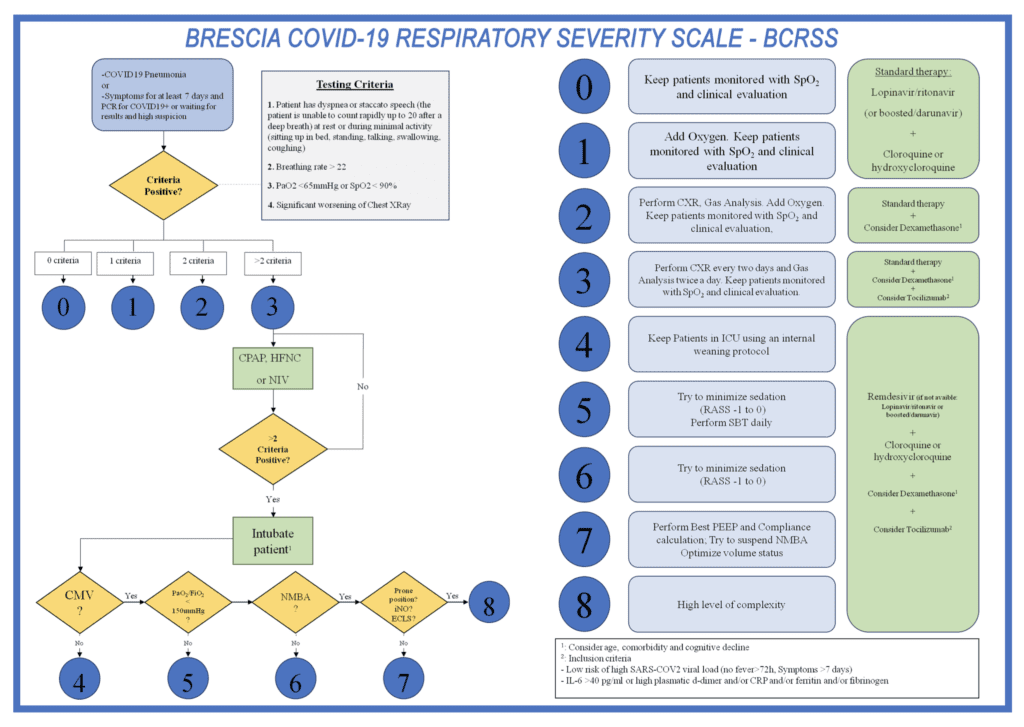
- Brescia-COVID Respiratory Severity Scale (BCRSS) Algorithm – Italy [Link is HERE]
-
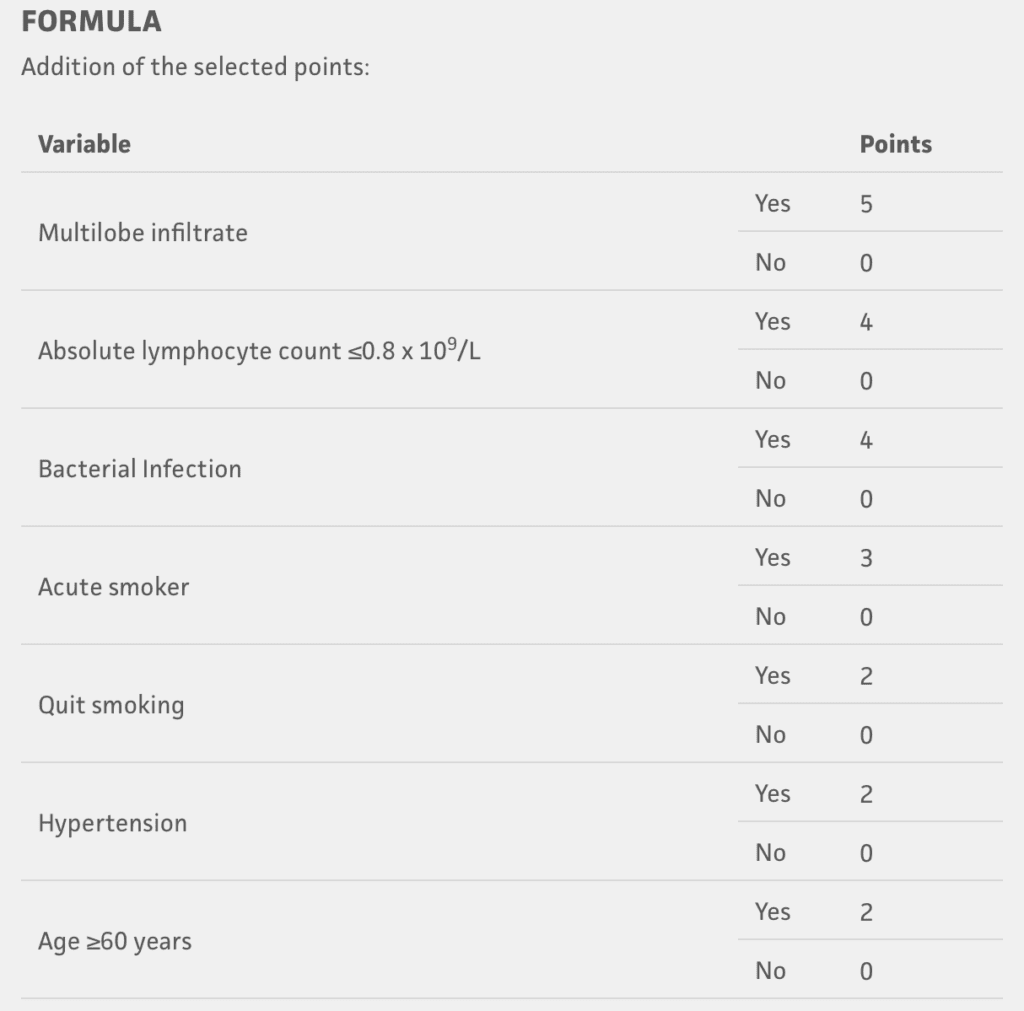
- MuLBSTA Score – China [Link is HERE]
For More Thoughts on This Topic Checkout:
- REBEL EM: COVID-19 – The Novel Coronavirus 2019
- First10EM: COVID Ethics: Should Clinicians see Patients Without Appropriate PPE?
- ALiEM: Healthcare Providers in the COVID-19 Era – Keeping Clean When Coming Home
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami) and Mizuho Morrison, DO (Twitter: mizuhomorrison)
The post COVID-19: Protecting Our Families and Patient Disposition appeared first on REBEL EM - Emergency Medicine Blog.