
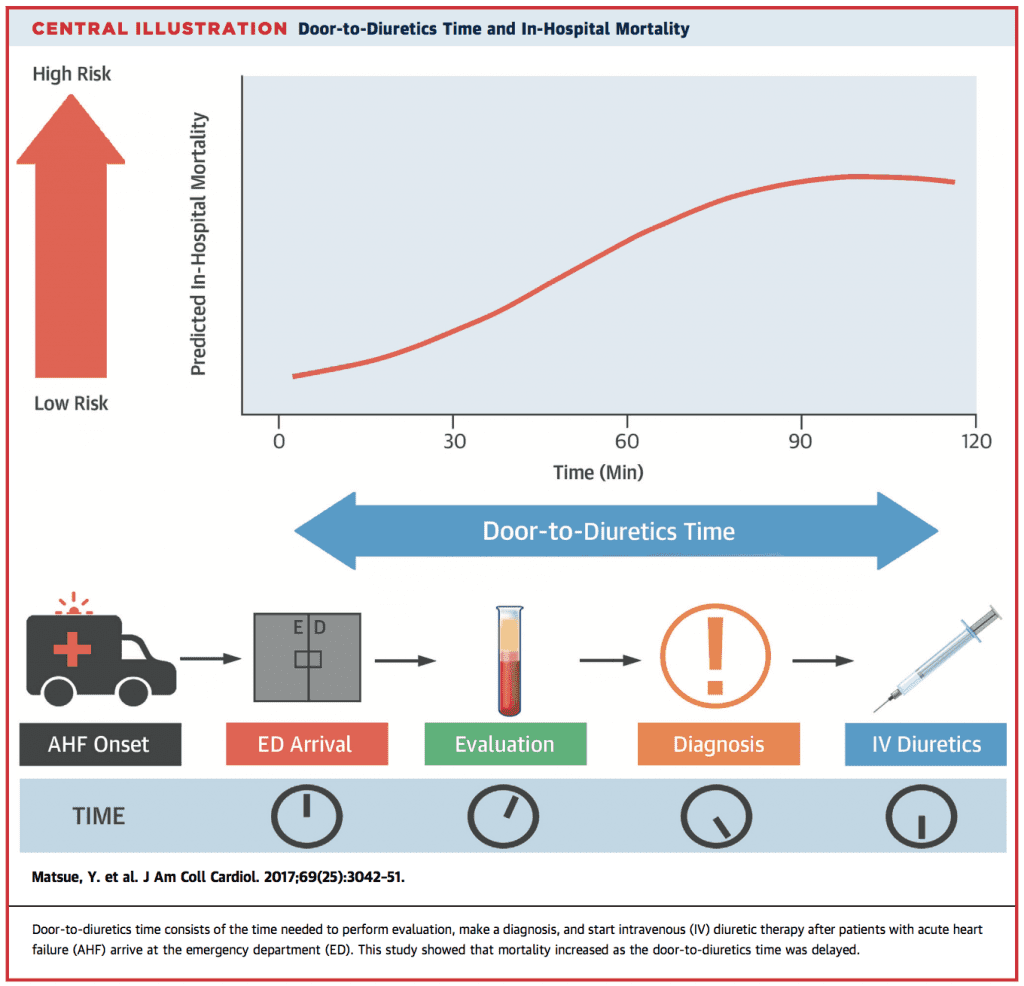
 Background: Acute congestive heart failure (AHF) is a common complaint seen in the ED and associated with a high morbidity, mortality, cost, and resources. Many patients with AHF, ultimately end up being admitted and interventions in the ED can make a huge difference in the outcomes of these patients. The REALITY-AHF (Registry Focused on Very Early Presentation and Treatment in Emergency Department of Acute Heart Failure) was a prospective, multicenter, observational study with the primary goal of evaluating the door to furosemide time in the treatment of AHF and clinical outcomes.
Background: Acute congestive heart failure (AHF) is a common complaint seen in the ED and associated with a high morbidity, mortality, cost, and resources. Many patients with AHF, ultimately end up being admitted and interventions in the ED can make a huge difference in the outcomes of these patients. The REALITY-AHF (Registry Focused on Very Early Presentation and Treatment in Emergency Department of Acute Heart Failure) was a prospective, multicenter, observational study with the primary goal of evaluating the door to furosemide time in the treatment of AHF and clinical outcomes.
What They Did:
- REALITY-AHF (Registry Focused on Very Early Presentation and Treatment in Emergency Department of Acute Heart Failure)
- Prospective, multicenter, observational cohort study
- Assessing association between time to loop diuretic treatment and clinical outcomes in patients with AHF
- Door-to-Furosemide (D2F): Time from patient arrival at the ED to 1st IV furosemide injection
- D2F <60min were pre-defined as early treatment group
Outcomes:
- Primary: All-cause in-hospital mortality
Inclusion:
- Age ≥20 years
- AHF diagnosis in the ED within 3hr of their first evaluation
- Patients treated with IV furosemide <24 hrs of ED arrival
Exclusion:
- Treatment with an intravenous drug before ED arrival
- Previous heart transplantation
- On chronic peritoneal dialysis or hemodialysis
- Acute myocarditis
- Acute coronary syndrome requiring emergent or urgent revascularization
- Missing B-type natriuretic peptide (BNP) or N-terminal-proBNP (NT-proBNP) data
- BNP < 100 pg/mL or NT-proBNP < 300 pg/mL at baseline
Results:
- 1,291 AHF patients treated with IV furosemide within 24hrs of ED arrival
- Median D2F time = 90 min
- 481 patients (37.3%) early treatment group (<60 min)
- 810 patients (62.7%) non-early treatment group (>60 min)
- In-Hospital Mortality:
- D2F <60min: 2.3%
- D2F ≥60min: 6.0%
- p value = 0.002
Strengths:
- 20 participating hospitals, with a nice mix of university hospitals and non-university teaching hospitals
- Zero patients lost to follow up
- Attempted to adjust for confounders using a validated risk score
Limitations:
- Observational trial only allowing association not causation of earlier diuretic use
- Lack of randomization, could allow for multiple confounders that are not accounted for (i.e. NIPPV, Nitroglycerin, etc…)
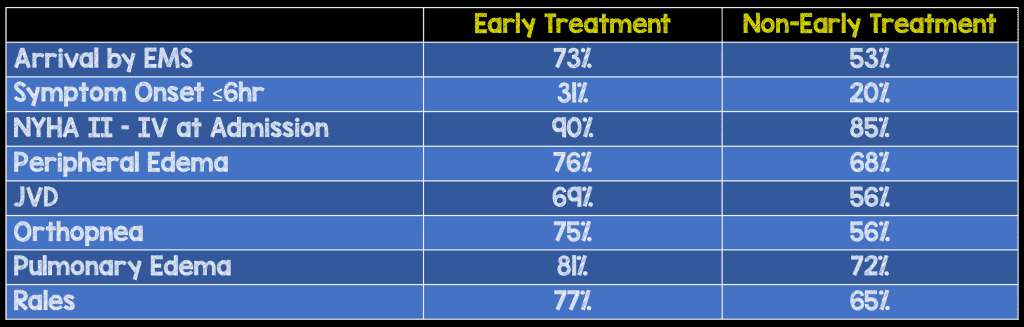
- Significant baseline differences between groups including acuteness of symptoms (≤6hrs), higher blood pressure, higher heart rate, and more signs of congestion were in the early treatment group causing an imbalance of clear cut volume overload in the early treatment group vs diagnostic conundrums in the non-early treatment group
- Patients in the early treatment group were more likely to arrive via ambulance (73% vs 53%) which leads to earlier treatment
- Small number of events
- No information on respiratory rate or cause of HF exacerbation
Discussion:
- Some interesting baseline differences between early and non-early treatment with furosemide:
- It should be noted that the authors state that association, not causality was demonstrated in the present study and that this study is a hypothesis-generating study that needs to be reproduced.
Author Conclusion: “In this prospective multicenter, observational cohort study of patients presenting at the ED for AHF, early treatment with intravenous loop diuretics was associated with lower in-hospital mortality.”
Clinical Take Home Point: We must be careful in making brash conclusions from this study. Although the authors conclude early treatment with IV loop diuretics is associated with lower in-hospital mortality, it is important to remember, patients in the early treatment group were more likely to arrive by ambulance, have an onset of symptoms that was more abrupt, and have more obvious signs of volume overload. All these confounders, would lead to earlier treatment with IV diuretics, meanwhile the quality of care as well as other treatments not accounted for (i.e. NIPPV and/or nitrates) may be the reason why mortality was improved.
References:
- Matsue Y et al. Time-to-Furosemide Treatment and Mortality in Patients Hospitalized With Acute Heart Failure. JACC 2017. PMID: 28641794
Post Peer Reviewed By: Anand Swaminathan (Twitter: @EMSwami)
The post Door to Furosemide (D2F) in Acute CHF…Really? appeared first on REBEL EM - Emergency Medicine Blog.
