
 Background Information: Sepsis is a complex syndrome frequently encountered in the ED. This infection-triggered, multifaceted disorder of life-threatening organ dysfunction is due to the body’s dysregulated response to pathologic and biochemical abnormalities.2-4 There has been significant debate regarding the use of clinical decision tools such as Systemic Inflammatory Response Syndrome (SIRS) and quick Sepsis-related Organ Failure Assessment (qSOFA) in the early recognition of sepsis.2,5-7 Multiple studies have shown SIRS to not be specific enough for the early detection of sepsis as many non-infectious processes, including exercise, can often meet many of its criteria.8-10 On the other hand, qSOFA has been criticized as having poor sensitivity and moderate specificity for short-term mortality.11,12 Furthermore, qSOFA has been described as clinically valuable but an imperfect marker of sepsis as some forms of organ dysfunction, such as hypoxemia and renal failure, are not assessed using qSOFA.5 Another severity score known as the National Early Warning Score (NEWS) focuses on inpatient deterioration in detecting patients with increased risk of early cardiac arrest, unanticipated ICU admission and death.13 One study showed that utilization of NEWS in the emergency department (ED) has been shown to be effective in recognizing patients with sepsis who are at a higher risk of adverse outcomes.14 The authors of this study sought to review the use of NEWS as an early sepsis screening score, a predictor of severe sepsis/septic shock, and compare it to SIRS and qSOFA in an ED triage setting.
Background Information: Sepsis is a complex syndrome frequently encountered in the ED. This infection-triggered, multifaceted disorder of life-threatening organ dysfunction is due to the body’s dysregulated response to pathologic and biochemical abnormalities.2-4 There has been significant debate regarding the use of clinical decision tools such as Systemic Inflammatory Response Syndrome (SIRS) and quick Sepsis-related Organ Failure Assessment (qSOFA) in the early recognition of sepsis.2,5-7 Multiple studies have shown SIRS to not be specific enough for the early detection of sepsis as many non-infectious processes, including exercise, can often meet many of its criteria.8-10 On the other hand, qSOFA has been criticized as having poor sensitivity and moderate specificity for short-term mortality.11,12 Furthermore, qSOFA has been described as clinically valuable but an imperfect marker of sepsis as some forms of organ dysfunction, such as hypoxemia and renal failure, are not assessed using qSOFA.5 Another severity score known as the National Early Warning Score (NEWS) focuses on inpatient deterioration in detecting patients with increased risk of early cardiac arrest, unanticipated ICU admission and death.13 One study showed that utilization of NEWS in the emergency department (ED) has been shown to be effective in recognizing patients with sepsis who are at a higher risk of adverse outcomes.14 The authors of this study sought to review the use of NEWS as an early sepsis screening score, a predictor of severe sepsis/septic shock, and compare it to SIRS and qSOFA in an ED triage setting.
Clinical Question:
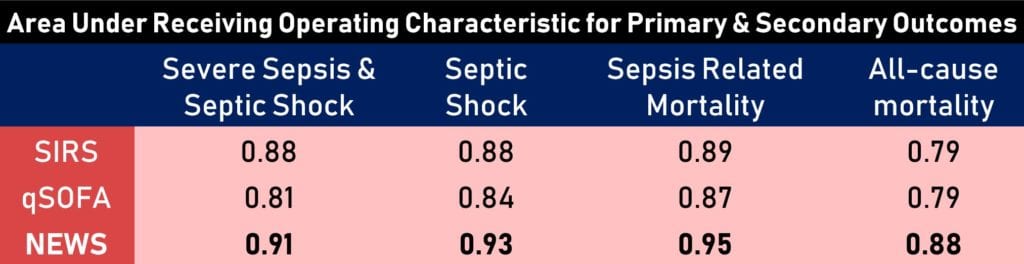
Which of the following severity scores: SIRS, NEWS or qSOFA, was the most accurate for the identification of severe sepsis and septic shock during ED triage? It is important to remember that accuracy here is how close the measured value is to the actual true value and the authors use an area under receiving operating characteristic (AUROC) curve which represents a measure of separability between different groups. The higher the AUROC the more accurate a value is.
What They Did:
- Retrospective data analysis collected from a single urban tertiary-care academic center with approximately 60,000 ED visits per year
- Secondary analysis of data collected from January 2014 to April 2015 and February 2016 to December 2016 as part of a quality improvement initiative. Data identifying positive sepsis cases was not available between these dates and was thus not included in analysis.
- Collected the following data points:
- Vital Signs (Blood pressure, heart rate, respiratory rate, pulse oximetry and temperature)
- Glasgow Coma Scale (GCS)
- Oxygen supplementation
- Demographics
- Leukocyte count
- Bands
- Disposition
- In-hospital mortality
- Evaluated entire study population for the presence of severe sepsis or septic shock within 8 hours
- Each flagged chart was reviewed by an emergency medicine physician using a standardized process to determine whether suspected infection related to organ dysfunction occurred within 8 hours of ED arrival.
- Defined severe sepsis as: two or more SIRS criteria, concern for infection and any of the following:
- Lactic acid > 2.0 mmol/L
- Systolic blood pressure (SBP) < 90 mmHg
- Mean arterial pressure (MAP) < 65 mmHg
- Creatinine 0.5 mg/dL above baseline
- INR > 1.5 (for patients not on anticoagulation)
- Platelets < 100,000/L
- Total bilirubin > 2mg/dL (that was not a previous baseline)
- Defined septic shock as having severe sepsis plus one of the following:
- Persistent hypotension (SBP < 90mmHg or MAP < 65 mmHg) despite a one-liter fluid challenge
- Lactic acid > 3.9 mmol/L
- Need for vasopressor within eight hours of ED arrival
- They assessed predictive ability using the area under the receiver-operating characteristic (AUROC) curves.
Inclusion Criteria:
- All ED patients over the age of 18 years old with the following:
- ICD-9 or ICD-10 billing codes for sepsis.
- Clinical concern for sepsis who had blood cultures, urine or antibiotics ordered within 12 hours of arrival
- Organ dysfunction within 8 hours of ED arrival
Exclusion Criteria:
- ED dispositions that did not allow for full calculation of scores or adequate clinician evaluation which included the following:
- Left without being seen
- Arrived in error
- Eloped
- Left against medical advice
- Left before triage
- Sent to labor and delivery
- Incomplete documentation
- Patients with left ventricular assist devices (unless lactic acid was greater than 2.0 mmol/L)
Outcomes:
- Primary endpoint was:
- Diagnosis of severe sepsis inclusive of septic shock within eight hours of ED arrival
- Secondary endpoints were:
- Severe sepsis
- Septic shock
- Sepsis-related (in-hospital mortality)
Results:
- Of the 130,595 ED visits, 115,734 (89%) met inclusion criteria.
- “Left without being seen” comprised 10,657 (71.7%) of the total 14,861 excluded dispositions
- 29,658 (25.6%) of the 115,734 patients were admitted to the hospital. 72.5% of patients were discharged. No disposition data was available for the remaining 1.9% of patients.
- 930 cases of severe sepsis and septic shock
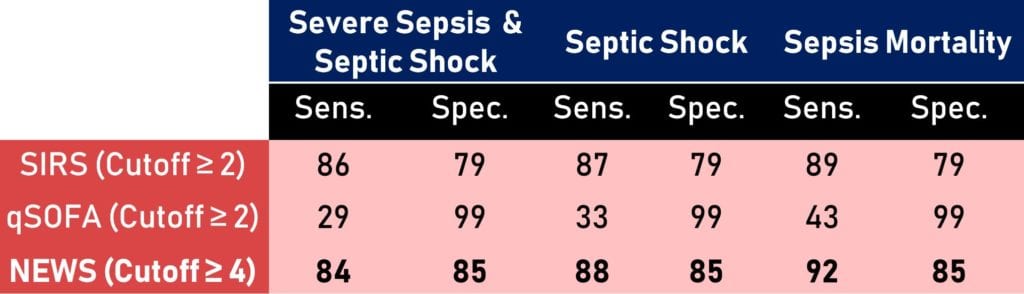
- AUROCs for the detection of severe sepsis or septic shock for each severity score was as follows:
- SIRS = 0.88
- qSOFA = 0.81
- NEWS = 0.91
- AUROCs for the detection of secondary endpoints included the following
- Septic shock
- SIRS = 0.88
- qSOFA = 0.84
- NEWS = 0.93
- Sepsis related mortality
- SIRS = 0.89
- qSOFA = 0.87
- NEWS = 0.95
- All-cause mortality
- SIRS = 0.79
- qSOFA = 0.79
- NEWS = 0.88
- Septic shock
Critical Results:
- NEWS showed no statistically significant difference compared to SIRS in predicting severe sepsis exclusive of septic shock yet was more predictive of severe illness and death
- In this retrospective cohort, NEWS was superior to qSOFA in predicting outcomes across all illness severity
Strengths:
- Attempted to eliminate subjectivity of “suspected infection” by confirming with treating providers and a multidisciplinary quality improvement group
- Data abstractors were blinded to input variable for sepsis scores and clinical end-points
- Used consistent and widely-accepted definition of organ dysfunction in severe sepsis and septic shock as noted above
- Calculated scores for unselected patients vs only those with suspicion for infection.
- Set a defined endpoint timeline of eight hours of ED arrival time which is clinically relevant to the ED physician.
- Minimal inclusion criteria focused on all patients rather than just sick patients allowed for generally larger mortality AUROC thus added to accuracy of results however also it also raises concern for selection bias.
Limitations:
- Single center study with predominantly African-American population making generalizability to other EDs more difficult
- Retrospective analysis increases risk for misclassification biases and confounding
- No conclusions regarding prospective performance can be drawn
- Endpoint determination was subject to reviewer bias as it was established retrospectively and unblinded
- Determination of severe sepsis was based on Sepsis-2 guidelines which may have resulted in an incorporation bias favoring SIRS
- “Physiologically impossible or implausible values were removed” from data collection, authors did not specify what these values were
- Non-blinded physician reviewing flagged charts using standardized process was the author, creating the potential for expectancy bias
- Standardized process of flagged chart review was not elaborated on
Discussion:
-
The authors found NEWS to be more accurate when compared with both SIRS and qSOFA for the early detection of severe sepsis and septic shock, septic shock alone and sepsis-related mortality.
- NEWS accuracy driven largely by superior specificity over SIRS at the cost of minimal decrease in sensitivity
- The authors note that NEWS outperforms SIRS is likely due to the inclusion of mental status, blood pressure and oxygenation, which are all readily available indicators of end-organ dysfunction
- Unlike SIRS, NEWS is immediately available at triage and does not require any laboratory testing and may allow quicker recognition and treatment of sepsis.
- The authors acknowledge that NEWS was developed for the clinical deterioration of inpatients and not the detection of sepsis in the ED. Therefore, they hypothesize the adjustment of some variables may make it more relevant to sepsis and lead to its improved use.
- SIRS was found to be superior to qSOFA for the prediction of severe sepsis and septic shock as well as the prediction of septic shock alone, however it showed no significant difference for predicting sepsis-related mortality.
- The authors further state that the low sensitivity of qSOFA compared to NEWS and SIRS makes it a poor choice as a screening tool
- Their results are consistent with previous studies showing qSOFA favors specificity over sensitivity. 6,11,12,15
- They go on to state that the qSOFA fails to achieve higher sensitivity because it omits important physiologic variables, such as heart rate and temperature, which precede clinical deterioration.14,17
- The authors of this study stated that they have adopted NEWS as initial screen for sepsis using a two-tier system
- Any score greater than 6 automatically flags the patient as potential severe sepsis
- Any score greater than 3 flags the patient as potential severe sepsis if deemed to be a high-risk for infection, including reported fever, history of immunocompromise, indwelling catheter or triage nurse concern for infection
Authors’ Conclusions:
- While SIRS, qSOFA and NEWS all have the ability to detect all sepsis endpoints, NEWS was the most accurate of the three. Furthermore, NEWS was more specific with similar sensitivity relative to SIRS, improves with disease severity and is immediately available without the need for laboratory evaluation. NEWS may be better for automated computation. Lastly, qSOFA had the lowest sensitivity and is a poor tool for ED sepsis screening.
Our Conclusion:
- This single-center retrospective analysis shows promising results with NEWS as a screening tool primarily because it can be done at triage and does not require any laboratory evaluation
- This study adds to the current knowledge that qSOFA should not be used as a sepsis screening tool as it has poor sensitivity and moderate specificity for short-term mortality. 7,11
- While the methodology of this study is extensively detailed, it is important to note some significant flaws. The author serving as the non-blinded physician reviewing charts through an undescribed standardized process questions its internal validity.
- This study highlights the accuracy of NEWS and its potential to serve as a useful screening tool for sepsis, however it coincidentally also emphasizes the need for an adjustment of its variables to be more “sepsis appropriate”.
- The NEWS score was developed to detect inpatients with increased risk of unplanned ICU admission, cardiac arrest and in-hospital death within 24 hours.13 Although not validated for utility in other settings, this study joins several others advocating for its validation and use in the ED.14,17,18
- Further prospective studies comparing the automated computation of NEWS, or a simplified sepsis-appropriate version, to SIRS are needed to validate the widespread use of these severity scores in the early detection of sepsis.
Potential to Impact Current Practice:
- While SIRS has been traditionally used as a sepsis screening tool, other severity scores such as NEWS have shown promising results in the early detection of sepsis and sepsis-related mortality. Furthermore, given its low sensitivity, qSOFA should not be used as a screening tool and has limited utility in detecting sepsis in the ED setting. Prospective studies comparing NEWS to SIRS may drive change in early evaluation of septic patients in the ED.
Clinical Bottom Line:
- In this limited retrospective study, NEWS was more accurate than both SIRS and qSOFA for the early detection of severe sepsis and septic shock. This severity score is calculable at triage, improves in prediction with increasing illness severity, and may better allow for risk stratification, however until prospective performance of the score in the ED can be determined, SIRS remains the most sensitive algorithm for predicting patients at risk for severe sepsis and septic shock.
REFERENCES:
- Usman O, et al. Comparison of SIRS, qSOFA, and NEWS for the early identification of sepsis in the Emergency Department. Am J Emerg Med. 2018. PMID: 30470600
- Singer M et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016. PMID: 26903338
- Vincent JL, Opal S, Marshall JC, Tracey KJ. Sepsis definitions: time for change. Lancet. 2013. PMID: 23472921
- Rhodes A, et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Crit Care Med 2017 PMID: 28098591
- Vincent J-L, et al. qSOFA does not replace SIRS in the definition of sepsis. Crit Care 2016. PMID: 27423462
- Williams JM, et al. Systemic Inflammatory Response Syndrome, Quick Sequential Organ Function Assessment, and Organ Dysfunction: Insights From a Prospective Database of ED Patients With Infection. Chest 2017. PMID: 27876592
- Rezaie S. The SIRS & qSOFA Confusion in Sepsis – REBEL EM – Emergency Medicine Blog. REBEL EM – Emergency Medicine Blog. Published 2018. Link is HERE
- Sprung CL, et al. An evaluation of systemic inflammatory response syndrome signs in the Sepsis Occurrence in Acutely Ill Patients (SOAP) study. Intensive Care Med. 2006. PMID: 16479382
- Dulhunty JM, et al. Does severe non-infectious SIRS differ from severe sepsis? Results from a multi-centre Australian and New Zealand intensive care unit study. Intensive Care Med. 2008. PMID: 18504549
- Churpek MM, et al. Incidence and prognostic value of the systemic inflammatory response syndrome and organ dysfunctions in ward patients. Am J Respir Crit Care Med. 2015 PMID: 26158402
- Fernando SM et al. Prognostic Accuracy of the Quick Sequential Organ Failure Assessment for Mortality in Patients With Suspected Infection: A Systematic Review and Meta-Analysis. Ann Intern Med 2018. PMID: 29404582
- Askim Å, et al. Poor performance of quick-SOFA (qSOFA) score in predicting severe sepsis and mortality – a prospective study of patients admitted with infection to the emergency department. Scand J Trauma Resusc Emerg Med 2017. PMID: 28599661
- Smith GB, et al. The ability of the National Early Warning Score (NEWS) to discriminate patients at risk of early cardiac arrest, unanticipated intensive care unit admission, and death. 2013 PMID: 23295778
- Corfield AR, et al. Utility of a single early warning score in patients with sepsis in the emergency department. Emerg Med J 2014. PMID: 23475607.
- Churpek MM, et al. Quick Sepsis-related Organ Failure Assessment, Systemic Inflammatory Response Syndrome, and Early Warning Scores for Detecting Clinical Deterioration in Infected Patients outside the Intensive Care Unit. Am J Respir Crit Care Med 2017. PMID: 27649072
- Barriere SL, et al. An overview of mortality risk prediction in sepsis. Crit Care Med 1995. PMID: 7867363
- Abbott TE, et al. A single-centre observational cohort study of admission National Early Warning Score (NEWS) 2015. PMID: 25943011
- Goulden R, et al. qSOFA, SIRS and NEWS for predicting inhospital mortality and ICU admission in emergency admissions treated as sepsis. Emergency Medicine Journal. 2018. PMID: 29467173
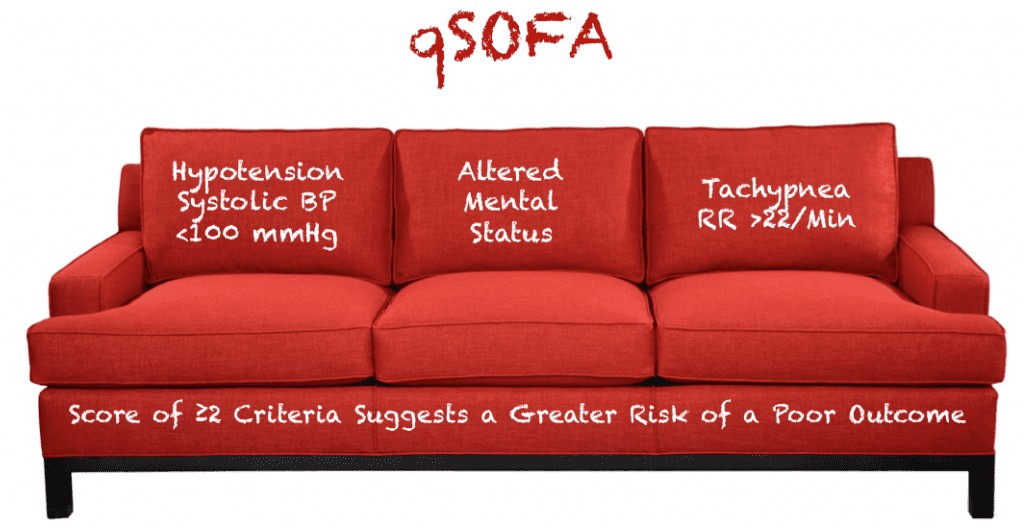
Figure 1: Quick Sepsis-related Organ Failure Assessment breakdown of parameters
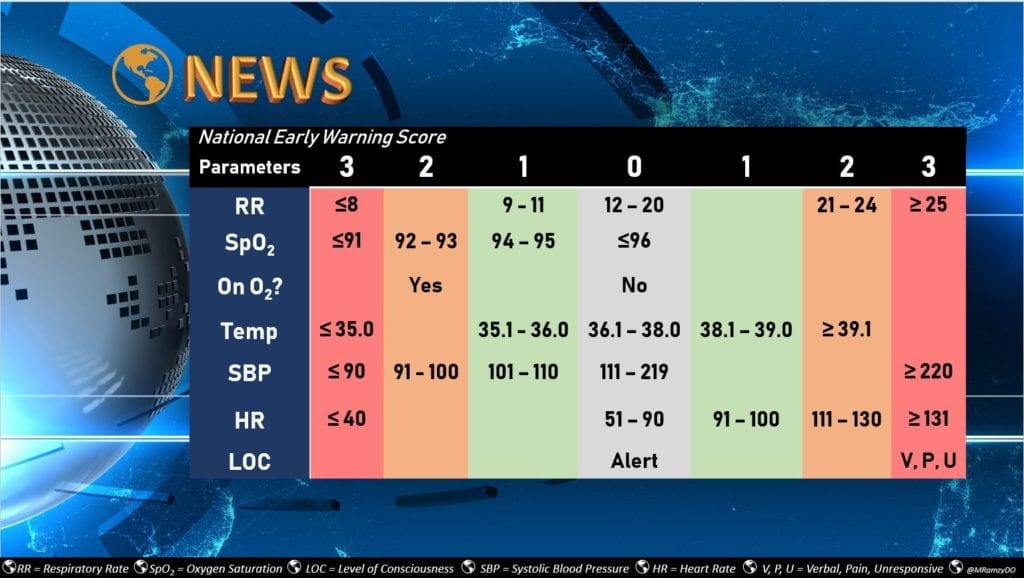
Figure 2: National Early Warning Score breakdown of parameters with labeled scoring
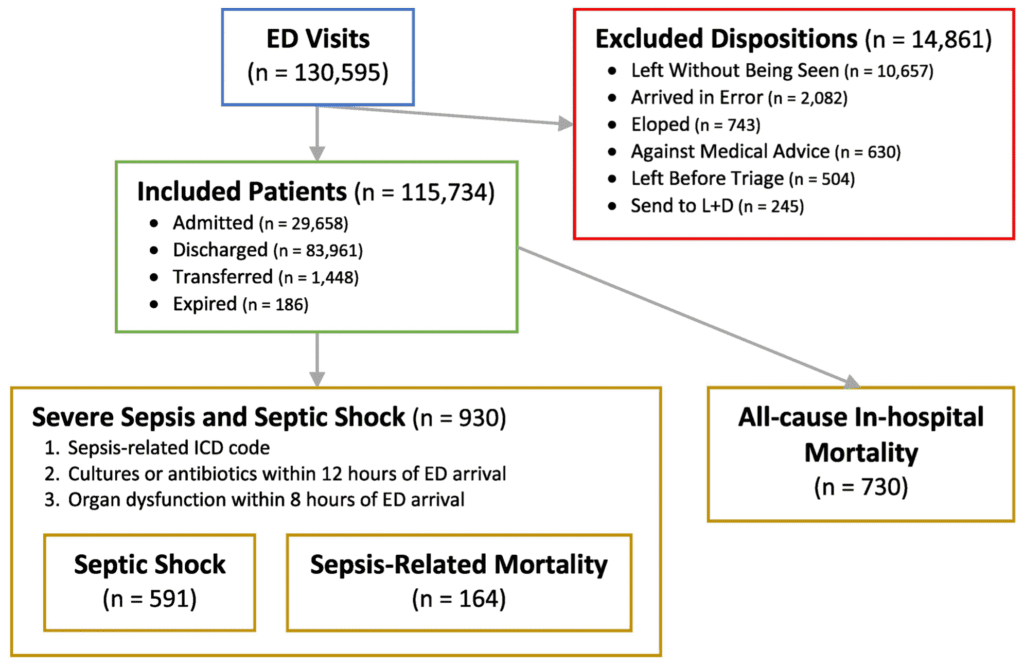
Figure 3: Study population, exclusions, inclusion and endpoints created by the study authors
Post Peer Reviewed By: Rick Pescatore, DO (Twitter: @Rick_Pescatore)
The post Early Sepsis Screening in the Emergency Department appeared first on REBEL EM - Emergency Medicine Blog.
