
 Background/Introduction: The use of Sodium Bicarbonate (SB) in cardiac arrest has had a complicated history with strong and varied opinions on its effectiveness. SB was recommended in earlier ACLS guidelines, mostly stemming from the notion that severe metabolic acidosis due to hypoxia and hypoperfusion during cardiac arrest led to impaired myocardial contractility, decreased effectiveness of vasopressors, and increased risk of dysrhythmias. Subsequent data called into question the benefits of SB in cardiac arrest and highlighted potential harms such as hypernatremia, hyperosmolarity, metabolic alkalosis, as well as reduction in ionized calcium, vascular resistance, and extracellular fluid volume expansion. This led to the 2010 ACLS guidelines stating that routine use of SB is not recommended (Class IIIB) and that it may be considered in special circumstances (preexisting metabolic acidosis, Hyperkalemia, or TCA overdose).
Background/Introduction: The use of Sodium Bicarbonate (SB) in cardiac arrest has had a complicated history with strong and varied opinions on its effectiveness. SB was recommended in earlier ACLS guidelines, mostly stemming from the notion that severe metabolic acidosis due to hypoxia and hypoperfusion during cardiac arrest led to impaired myocardial contractility, decreased effectiveness of vasopressors, and increased risk of dysrhythmias. Subsequent data called into question the benefits of SB in cardiac arrest and highlighted potential harms such as hypernatremia, hyperosmolarity, metabolic alkalosis, as well as reduction in ionized calcium, vascular resistance, and extracellular fluid volume expansion. This led to the 2010 ACLS guidelines stating that routine use of SB is not recommended (Class IIIB) and that it may be considered in special circumstances (preexisting metabolic acidosis, Hyperkalemia, or TCA overdose).
Despite this, the use of SB during cardiac arrest is still common in emergency departments with varying opinions on its effectiveness. In fact, recently published data from the National Emergency Medicine Services Information System (NEMSIS) noted that besides epinephrine and normal saline, sodium bicarbonate was the third most commonly used medication in out of hospital cardiac arrest (Chan 2020). This study aimed to consolidate the state of evidence behind the use of SB in cardiac arrest.
Paper: Wu KH et al. Effectiveness of Sodium Bicarbonate Administration on Mortality in Cardiac Arrest Patients: A Systematic Review and Meta-analysis. J Emerg Med. 2020. PMID: 32978028
Clinical Question: In adult patients with non-traumatic cardiac arrest, does the administration of sodium bicarbonate improve return of spontaneous circulation (ROSC) and survival to discharge rates?
What They Did:
- Systematic Review and Meta-Analysis
- Search of three databases (Medline, Scopus, Cochrane Central Register of Controlled Trials) from inception to December 2019
- Inclusion of observational (retrospective and prospective) and randomized controlled trials (RCTs).
- Two reviewers assessed methodological quality and bias risk of enrolled studies using the Newcastle-Ottawa Scale (NOS)
- Two reviewers performed data abstraction of key variables
- Odds Ratios (OR) and Confidence Intervals (CI) were collected for ROSC with administration of sodium bicarbonate as well as for survival to discharge with administration of sodium bicarbonate when compared to a control group
- Subgroup analysis was also done considering year of study (due to changing ACLS guidelines over time) and continent where study was performed
- Meta-analysis was performed using a random-effect model
Outcomes:
-
Primary Outcomes:
- ROSC
- Survival to Discharge
-
Inclusion Criteria:
- Adult, Non-Traumatic Cardiac Arrest Patients
- Intravenous Sodium Bicarbonate Administration During Cardiac Arrest
- Studies contained at least two treatment arms, one with sodium bicarbonate administration and one without
-
Exclusion Criteria:
- Specific Population Subgroups: Pre-Existing Acidosis, Intoxication, Drug Abuse
- Animal Studies
- Case Reports and Case Series
- Non-English and Non-Chinese Manuscripts
Results:
-
Search Results:
- 849 citations identified during literature search
- 714 studies reviewed after removal of duplicates
- 15 studies were assessed for eligibility
- 6 studies were included with 18,406 patients
- 6 Included Studies:
- 50% from North America (United States, Canada), 50% from East Asia (Korea, Taiwan, Hong Kong)
- Study design was retrospective in 4 studies and prospective in 2 studies
- Mean Age: 65-71.8
- Risk of bias
- NOS quality assessment showed 5 high quality observational studies and 1 moderate quality observational study
- 849 citations identified during literature search
-
Primary Outcome:
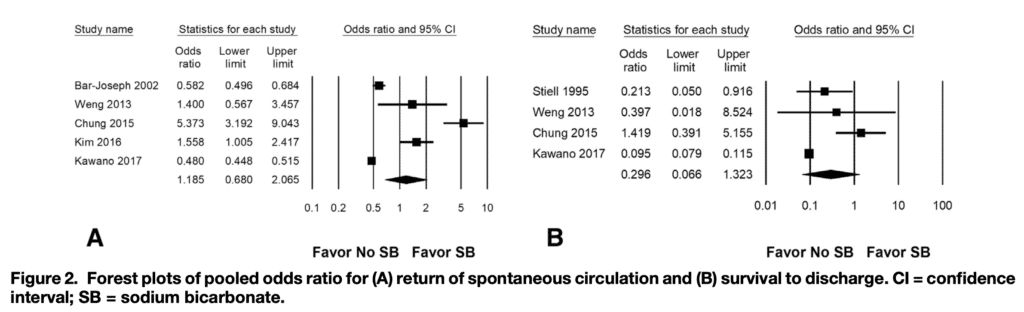
- ROSC: Administration of Sodium Bicarbonate had overall OR of 1.185 (95% CI: 0.680-2.065)
- Survival to Discharge: Administration of Sodium Bicarbonate had overall OR of 0.296 (95% CI: 0.666-1.323)
-
Subgroup Analysis (ROSC):
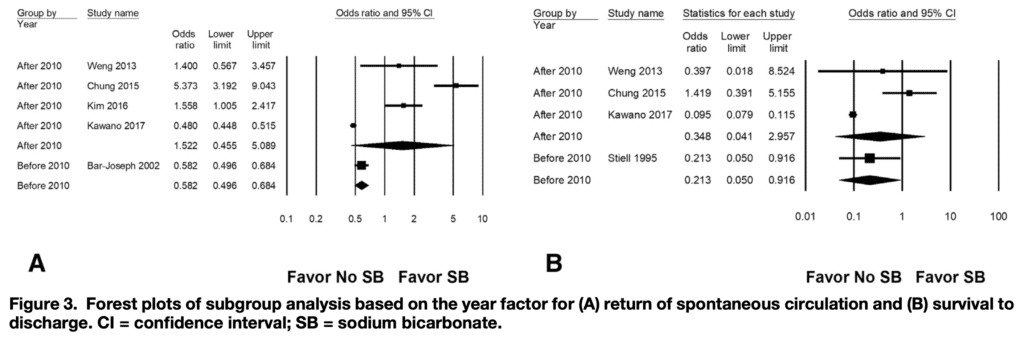
- Year (after 2010): Administration of Sodium Bicarbonate had overall OR of 1.522 (95% CI: 0.455-5.089)
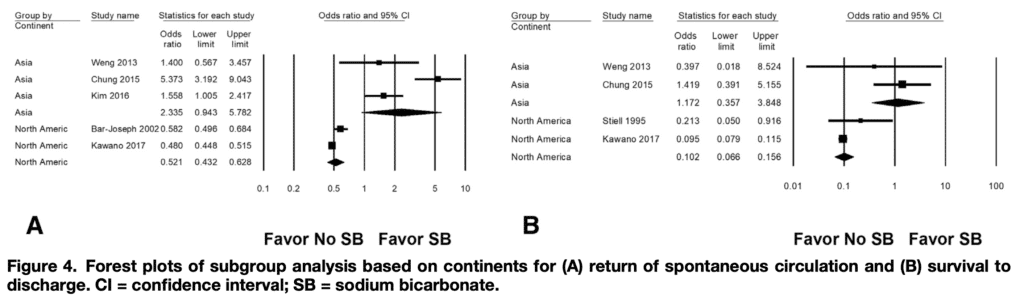
- North American Continent: Administration of Sodium Bicarbonate had overall OR of 0.521 (95% CI: 0.432-0.628)
- East Asian Continent: Administration of Sodium Bicarbonate had overall OR of 2.335 (95% CI: 0.943-5.782)
-
Subgroup Analysis (Survival to Discharge):
- Year (after 2010): Administration of Sodium Bicarbonate had overall OR of 0.348 (95% CI: 0.041-2.957)
- North American Continent: Administration of Sodium Bicarbonate had overall OR of 0.102 (95% CI: 0.066-0.156)
- East Asian Continent: Administration of Sodium Bicarbonate had overall OR of 1.172 (95% CI: 0.357-3.848)
Strengths:
- 1st systematic review/meta-analysis on the use of sodium bicarbonates effect in cardiac arrest
- Adds information to a question with limited and inconsistent previous research
- Multiple databases searched resulting in a high number of included patients
- Adherence to guideline recommendations for systematic reviews/meta-analyses
- Used the Newcastle-Ottawa Scale (NOS) to evaluate the risk of bias in each of the studies included
Limitations:
- Largest limitation was that only 6 studies were included
- Of the included studies, all were observational in nature and majority were retrospective
- Confounders such as downtime, initial rhythm, bystander CPR, witnessed or unwitnessed cardiac arrest, cardiac arrest location, use of other medications during cardiac arrest, time to first sodium bicarbonate administration and overall dose were not completely reported in the included studies
- Pre-existing co-morbid conditions, septicemia, pre-existing hyperkalemia, or metabolic acidosis and post-ROSC management were not reported
- Post-ROSC management including TTM and coronary angiography poorly reported in most studies
- Studies in the Asian group were conducted in the ED and the North American group varied from EMS, ED, ward, and ICU
- High heterogeneity was reported for the primary outcomes
- Primary outcomes were not patient-centered such as good neurological outcome
Discussion:
- The authors note that Sodium Bicarbonate administration during resuscitation showed no significant difference in their primary outcomes of ROSC or Survival to Discharge.
- The authors note that in the subgroup analysis, which was done to account for high heterogeneity, there was no significant difference in mortality after the 2010 change in ACLS sodium bicarbonate guidelines.
- The authors note that in the subgroup analysis, significantly lower rates of ROSC and Survival to Discharge were noted in the North American group.
- The authors note that in subgroup analysis, Sodium Bicarbonate administration had a trend towards a higher rate of ROSC in the East Asian group.
- Cause of this was unclear and was mostly driven by the Chung 2015 study where 74 patients received Sodium Bicarbonate and noted an OR of 5.37, which was much higher than all the other studies included in this systematic review and meta-analysis.
- To date, this is the first systematic review and meta-analysis published that has looked into this question. There have been two randomized controlled trials that have looked at the use of Sodium Bicarbonate in the setting of cardiac arrest.
- Dybvik et al concluded that the use of Sodium Bicarbonate was not associated with improved survival (Dybvik 1995).
- Vukmir et al concluded that there was no difference in overall survival with administration of Sodium Bicarbonate. They noted a trend for improved survival in prolonged arrest (> 15 minutes) with the use of Sodium Bicarbonate, but this conclusion has been called into question due to being based on subgroup analysis and statistical misapplication (Vukmir 2006).
- Currently, a second systematic review and meta-analysis is being published with preliminary data that suggests lower rates of sustained ROSC and good neurological outcomes with the use of Sodium Bicarbonate (Alshahrani 2020).
Author Conclusion: “In this review, SB use was not associated with improvement in ROSC or survival-to-discharge rates in cardiac resuscitation.”
Clinical Take Home Point:
In this systematic review and meta-analysis, the use of Sodium Bicarbonate in cardiac arrest was not associated with improvements in the rates of ROSC or Survival to Discharge. The findings need to be interpreted in the context of inadequate number of included studies, poor statistical quality with high heterogeneity, and risk of bias/confounders. This is however, an important study that is attempting to clarify the evidence based nature of a routinely used medication during cardiac arrest, and hopefully will serve as a jumping off point for further research into identifying the role of Sodium Bicarbonate in cardiac arrest with special attention to patient oriented outcomes.
The bottom line is that the scales are being tipped towards refuting the use of sodium bicarbonate in cardiac arrest at this time and this is supported by ACLS guidelines except in special circumstances.
References:
- Chan H et al. Characteristics of adult out-of-hospital cardiac arrest in the National Emergency Medical Services Information System. J Am Coll Emerg Physicians Open. 2020. PMID: 33000069
- Dybvik T et al. PA. Buffer therapy during out-of-hospital cardiopulmonary resuscitation. Resuscitation. 1995. PMID: 7659873
- Vukmir R et al. Sodium Bicarbonate Study Group. Sodium bicarbonate improves outcome in prolonged prehospital cardiac arrest. Am J Emerg Med. 2006. PMID: 16490643
- Alshahrani M et al. Use of sodium bicarbonate in out-of-hospital cardiac arrest: A systematic review and meta-analysis. Critical care medicine. 2020. Link Here
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post Effectiveness of Sodium Bicarbonate Administration on Mortality in Cardiac Arrest Patients: A Systematic Review and Meta-Analysis appeared first on REBEL EM - Emergency Medicine Blog.
