
 Background: In critically ill patients needing IV access, ultrasound has helped improve gaining access to a set of peripheral veins, located deeper in the arm. The time it takes to do this however is not insignificant but even more importantly is that once you achieve success, the line can fail due to a short catheter length. Central venous catheters, often seen as a solution to this latter issue, are not without their own risks and complications. Therefore, a nice alternative option may be a midline catheter. These catheters are not meant for fast, large volume resuscitations because they also take time to place, but also have a longer catheter length which slows down infusion rates. Midline catheters are really about having safe access that is unlikely to be dislodged. This is a great option when you have medications you want to give but not have extravasation occur (i.e. vasopressors, hypertonic saline, calcium chloride, etc.).
Background: In critically ill patients needing IV access, ultrasound has helped improve gaining access to a set of peripheral veins, located deeper in the arm. The time it takes to do this however is not insignificant but even more importantly is that once you achieve success, the line can fail due to a short catheter length. Central venous catheters, often seen as a solution to this latter issue, are not without their own risks and complications. Therefore, a nice alternative option may be a midline catheter. These catheters are not meant for fast, large volume resuscitations because they also take time to place, but also have a longer catheter length which slows down infusion rates. Midline catheters are really about having safe access that is unlikely to be dislodged. This is a great option when you have medications you want to give but not have extravasation occur (i.e. vasopressors, hypertonic saline, calcium chloride, etc.).
Midline Catheters:
- The midline catheter (i.e. long peripheral catheter) is an IV catheter placed into a peripheral vein, with the distal tip located just proximal to the axilla. Midline catheters can range from 10 to 25cm in length, have a single or double lumen, and placed with Seldinger’s technique and ultrasonography.
Bard PowerGlide 20g x10cm Midline Catheter

Medcomp Dual-Lumen 5F x 20cm Midline Catheter
What They Did:
- Single center, prospective observational case series of all patients who had attempted midline catheter insertion in the ED
Observations:
-
Midline insertion: Indication, technique, location, catheter type, number of attempts, overall success or failure, vasoactive use, any immediate complications
- Insertion attempt = skin puncture
- Insertion-related complication = failed insertion, arterial puncture, infiltrations, and hematoma
-
Catheter dwell-time: catheter patency, flow, site appearance, and any potential complications
- Dwell time = total time midline catheter in place and functioning
- Dwell-time complications = inability to flush, catheter dislodgement, leakage from around the catheter site, insertion-site erythema, insertion-site pain, insertion site drainage, edema, ecchymosis, superficial thrombosis, deep venous thrombosis, line-associated bloodstream infections, vesicant extravasation, skin necrosis, and neurovascular injury
- Severe complications = Arterial injury, vesicant necrosis, skin necrosis, or neurovascular injury
- Line associated bloodstream infections = any positive blood-culture results in the presence of clinical signs of infection, without another source
Inclusion:
- Difficult IV access
- Need for reliable access during an active resuscitation
- Need for vasopressor or inotropic therapy
Exclusion:
- NA
Results:
- 403 midline catheters placed
- 187 (46%) were single lumen catheters
- 213 (53%) were double-lumen catheters
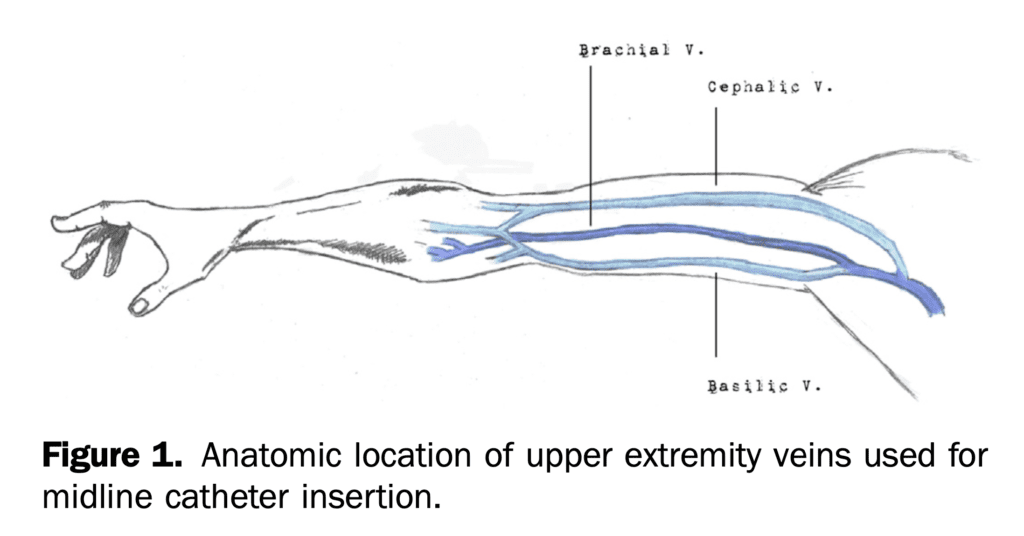
- Location of Insertion:
- Basilic Vein: 188 catheters (47%)
- Brachial Vein: 128 catheters (32%)
- Cephalic Vein: 59 catheters (15%)
-
Indications for Midline Catheters:
- IV Access/Medication Administration: 39%
- Need for IV Access Alone: 26%
- Need for IV Access, Medication Administration, and Ongoing Resuscitation: 17%
- Catheter insertion success: 99%
- Median number of attempts: 1 (Range 1 – 3)
- 1st Attempt: 259 catheters (64%)
- 2nd Attempt: 53 catheters (13%)
- 3rd Attempt: 7 catheters (3%)
- Median number of days catheter remained in place: 5 (Range 2 – 8)
- Median dwell time: 6.7 days (Range 1 – 48)
- Insertion related complications: 14 pts (3.5%; 95% CI 2.0% to 5.9%)
- Dwell-time related complications: 60 pts (12%; 95% CI 9% to 16%)

- Severe complications: 3 pts (0.7%)
- 1 arterial cannulation
- 2 vesicant extravasations
- NONE of these complications resulted in clinical consequences to the patient
- No difference in number of insertion attempts, catheter days, or complications based on anatomic insertion site (basilic, brachial, or cephalic veins) and anatomic side (right or left)
Strengths:
- This is the first study to describe midline catheter insertion in the ED in a general group of critically ill ED patients as opposed to patients with difficult access only
- One of the largest cohorts of patients undergoing midline catheter placement in the ED
- Of the 9 patients (2.2%) of patients missing insertion related complications data, charts were reviewed, and no obvious complications caused by midline catheter insertion were identified
Limitations:
- Formal depth or diameter thresholds were not established in this study
- Although a prospective trial, physicians performing the procedure inputted the outcomes into an online EMR making the results only as good as the data entered
- Reviewers extracting data from EMR were not blinded to the study
- 8% of patients had missing information on number of attempts and 2.2% were missing insertion related complications. It is possible these numbers were excluded due to a higher number of attempts and thus could bias results to favor a lower number of insertion attempts and possibly complications than what is reported
- Systematic screening for DVTs was not performed and therefore some extremity DVTs may have been missed
Discussion:
- Physicians were trained in patient and vessel selection, insertion techniques, took part in a 1- to 2-hour didactic session, and performed one supervised midline catheter to achieve certification
- Patients requiring vasopressors or inotropic agents had the 20g x 10cm single lumen midline used
- None of the midlines were heparin bonded or impregnated with antibiotics
- All lines placed with full sterile precautions
- Hospital policy required catheters be assessed 2 times per day for the duration of the dwell time
- Midline catheters were not considered potential sources for central-line-associated bloodstream infections (CLABSI). Investigations into midline catheters as potential sources of fever or positive blood culture results only pursued if there were clinical indications to do so. Therefore, it is possible that midline-catheter-associated blood stream infections were not documented and could overestimate the safety of the catheters
- Vasopressors used in 29.5% of midline catheters in this cohort of patients. 1 patient had an extravasation event with norepinephrine resulting in administration of phentolamine. The patient experienced no negative consequences otherwise
- The authors state a detailed analysis concerning the subset of patients receiving vasopressors is being conducted and will be published separately
Author Conclusion: “Midline catheters may present a feasible alternative to central venous access in certain critically ill ED patients.”
Clinical Take Home Point: Midline catheter placement is feasible in the ED as an alternate approach to central lines or standard US guided lines. Further research is needed to look at generalizability of placement at other institutions, time to placement and complication rates in comparison to central venous catheters.
References:
- Spiegel RJ et al. The Utility of Midline Intravenous Catheters in Critically Ill Emergency Department Patients. Ann Emerg Med 2019. [Epub Ahead of Print]
For More Thoughts on This Topic Checkout:
- EMCrit: Midlines – Part 1
- EMNerd: The Adventure of the Sussex Vampire
- EMNerd: The Case of the Sussex Vampire Continues…
- EMCrit: Midlines – Part 2 – Explosion with Rory Spiegel
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)
The post Midline IV Catheters appeared first on REBEL EM - Emergency Medicine Blog.

