
 Background: Typical medical treatment of ACS patients include dual antiplatelet therapy (DAPT) and revascularization with primary percutaneous coronary intervention (PPCI). Nitroglycerin is first line therapy in the treatment of pain in ACS with morphine as a common adjunct. Morphine helps relieve pain which decreases catecholamines and oxygen demand. We have written about the use of Morphine in ACS before on REBEL EM and advocated for fentanyl over morphine for pain control in patients with refractory pain to IV nitroglycerin. However, two new trials have been published in the past month: An observational trial in 300 patients with STEMI receiving morphine and a randomized trial using fentanyl which requires us to revisit the use of opioids in ACS.
Background: Typical medical treatment of ACS patients include dual antiplatelet therapy (DAPT) and revascularization with primary percutaneous coronary intervention (PPCI). Nitroglycerin is first line therapy in the treatment of pain in ACS with morphine as a common adjunct. Morphine helps relieve pain which decreases catecholamines and oxygen demand. We have written about the use of Morphine in ACS before on REBEL EM and advocated for fentanyl over morphine for pain control in patients with refractory pain to IV nitroglycerin. However, two new trials have been published in the past month: An observational trial in 300 patients with STEMI receiving morphine and a randomized trial using fentanyl which requires us to revisit the use of opioids in ACS.
Morphine Analgesia in STEMI Patients Undergoing PCI [1]:
What They Did:
- Prospective, single center, observational trial of 300 patients with STEMI requiring primary percutaneous coronary intervention (PPCI)
- Morphine given in non-randomized fashion as needed for pain control
- All patients received dual-antiplatelet therapy (DAPT) and PPCI
Outcomes:
- ST segment resolution
- Coronary flow
- Thrombotic status
- Peak troponin
- Mortality at 30d
- Recurrent MI or Stroke at 30d
- Major and Minor Bleeding
Inclusion:
- Adult patients ≥18 years
- Presumed diagnosis of STEMI
- Given aspirin 300mg
- Given either clopidogrel 600mg or ticagrelor 180mg
Exclusion:
- Vomiting following DAPT loading pre-PPCI
- Intubated and ventilated
- Unable to swallow
- On oral anticoagulation
- Known coagulation disorders
- Platelet count <100k/L
- Hb < 80g/L
- Known active malignancy
- Inability to take DAPT
Results:
- 300 patients presenting for PPCI
- 218 patients (72.7%) received morphine
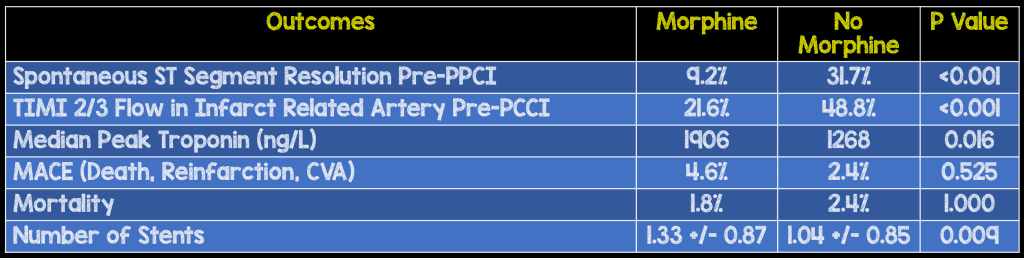
- No difference in major bleeding in patients receiving morphine vs no morphine
- Enhanced platelet reactivity and impaired endogenous fibrinolysis in patients receiving morphine vs no morphine
Strengths:
- Largest prospective study evaluating morphine vs no morphine in STEMI patients
- Measurement of thrombotic status was performed blinded to opiate use
- ECG and angiographic analyses were performed by investigators blinded to morphine use and thrombotic status results
- Two clinicians blinded to medication and thrombotic status confirmed all diagnoses
Limitations:
- Not a randomized controlled trial
- Single center study
- Authors did not specify what the primary vs secondary outcomes were. This may lead to reporting bias
- Potential confounder is that patients without spontaneous reperfusion may have more pain and a greater analgesia requirement (unclear which was the cause and which was the effect)
- Without randomization, two groups were not well balanced for all predictors (i.e. the group that got morphine appears sicker than the group that did not)
- Morphine appeared to be the standard care in this setting (>70% received it) which is not generalizable as other settings may not use as much morphine
- Majority of patients received clopidogrel pre-PPCI, but prasugrel and ticagrelor have a faster onset of action, and greater potency and superiority compared to clopidogrel
Discussion:
- Although listed as not statistically significant one factor worth mentioning is the morphine group had quite a bit more cardiogenic shock: 6.9 vs 3.7%; p = 0.41
- Subgroup analysis of patients receiving GPI showed no difference in pre-PPCI coronary flow or peak troponin according to morphine use
- Troponin elevation is considered a surrogate for infarct size. Therefore a higher troponin level would correlate to a larger infarct size, however in this study that did not translate into statistically significant short-term adverse events (This could simply be due to the small sample size)
- This is the largest prospective trial looking at the use of morphine in STEMI patients to date. Although there was an increase in surrogate outcomes (enhanced platelet reactivity, impaired endogenous fibrinolysis, reduced occurrence of spontaneous reperfusion pre-PPCI, and larger infarct size) this did not seem to affect 30 day clinical outcomes (Death, recurrent MI, or CVA).
Author Conclusion: “Our hypothesis-generating data suggest that morphine use in STEMI is associated with enhanced platelet reactivity, reduced spontaneous myocardial reperfusion (pre-PPCI) and larger infarct size, and these adverse effects may be influenced by glycoprotein IIb/IIIa inhibitor (GPI) use.”
Clinical Take Home Point: This is yet another hypothesis generating study showing increased surrogate outcomes in STEMI patients with the use of morphine for pain. Until further stronger evidence is available it is probably worth erring on the side of safety and reserving morphine in an individualized manner and using only when truly necessary in patients with refractory pain to IV nitroglycerin.
The PACIFY Trial: Fentanyl in Patients with ACS Undergoing PCI [2]
What They Did:
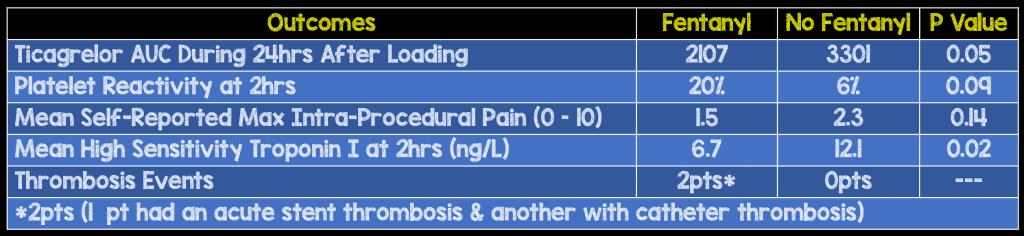
- Platelet Aggregation with tiCagrelor Inhibition and FentanYl (PACIFY)
- Single center randomized controlled trial
- Fentanyl vs no fentanyl in patients requiring PCI
- All patients requiring PCI received an oral dose of 180mg of ticagrelor at the completion of diagnostic angiography
Outcomes:
- Primary: Ticagrelor concentration during the 24hrs after loading
- Secondary:
- Platelet function at 2hrs
- Platelet inhibition at 2hrs
- Self-reported max pain from 0 – 10
Inclusion:
- Adults Age ≥18years
- Not receiving P2Y12 inhibitors for 14 days prior to enrollment
Exclusion:
- Pre-procedural treatment with oral anticoagulants or opiates
- Platelet count <100k
- Impaired renal or hepatic function
Results:
- 212 patients randomized:
- 70 required PCI and represented the intention to treat analysis
Strengths:
- Randomized clinical trial
- Patients and outcomes assessors blinded to treatment
- No baseline differences between groups
Limitations:
- Single Center Trial
- Non-patient centered outcomes
- Providers were not blinded to treatment
- Study was not powered for pain outcomes
Discussion:
- In the paper the authors state: “The practice of prophylactic fentanyl at the start of catheterization and PCI procedures may require reconsideration; though we cannot advocate for withholding this opiate where necessary for the treatment of pain.”
Author Conclusion: “This trial demonstrates that fentanyl administration lowers plasma concentrations of ticagrelor and delays its antiplatelet effects.”
Clinical Take Home Point: Another trial showing worsened surrogate outcomes (ie. Platelet reactivity), but no real clinically oriented outcomes shown
Clinical Bottom Line:
- The use of morphine with p2y12 inhibitor trials have reported worse surrogate outcomes such as platelet reactivity, but these surrogate outcomes have never translated into clinically important outcomes in trials to date
- Morphine and Fentanyl (Opioid Class) decrease gut motility and thus, absorption of P2y12 inhibitors. However, none of the trials reviewed above, or prior articles, have demonstrated a change in patient centered/clinically meaningful outcomes
- The use of opiates to treat refractory pain in ACS may still be reasonable. However, the resolution of pain with an opiate should not delay interventions as the cause of pain has been masked, and not treated.
- Have we have seen the death of MONA in ACS…Maybe. In a previous post we have discussed the acronym FAN (Fentanyl, Aspirin, Nitroglycerin), which is my current, preferred regimen in ACS, but its not because morphine is causing harm, but instead fentanyl’s cleaner pharmacodynamic profile.
References:
- Farag M et al. Morphine Analgesia Pre-PPCI Is Associated with Prothrombotic State, Reduced Spontaneous Reperfusion, and Greater Infarct Size. Thromb Haemost 2018. PMID: 29444530
- Mcevoy JW et al. Effect of Intravenous Fentanyl on Ticagrelor Absorption and Platelet Inhibition Among Patients Undergoing Percutaneous Coronary Intervention: The PACIFY Randomized Clinical Trial. Circulation 2018. PMID: 29046319
For More Thoughts on This Topic Checkout:
- REBEL EM: The Death of MONA Part 1 – Morphine
- Vince Digiulio at EMS12Lead: In Defense of Morphine (Part 1)
- Vince Digiulio at EMS12Lead: In Defense of Morphine (Part 2)
- Rory Spiegel at EMNerd(EMCrit): The Case of the Inconsequential Truth
Post Peer Reviewed By: Anand Swaminathan (Twitter: @EMSwami)
The post More Trials Showing Harm of Opioids in ACS…or do They? appeared first on REBEL EM - Emergency Medicine Blog.
