 Background: The most feared complication in the clinical course of children with diabetic ketoacidosis (DKA) is the development of cerebral edema. Cerebral edema is rare (<1%) but is the leading cause of death in pediatric DKA. Many of the details about the risk factors as well as the mechanisms leading to DKA related cerebral edema are not well understood. Before we review the recent, groundbreaking study by Kupperman et al (1), examining the relationship between intravenous fluid content and rate of fluid administration in the development of DKA related cerebral edema, it’s important that we review the associated risk factors as well as the proposed mechanisms. It is important to know that the available data we are about to review comes from retrospective studies as well as case reports and case series and not from randomized control trials.
Background: The most feared complication in the clinical course of children with diabetic ketoacidosis (DKA) is the development of cerebral edema. Cerebral edema is rare (<1%) but is the leading cause of death in pediatric DKA. Many of the details about the risk factors as well as the mechanisms leading to DKA related cerebral edema are not well understood. Before we review the recent, groundbreaking study by Kupperman et al (1), examining the relationship between intravenous fluid content and rate of fluid administration in the development of DKA related cerebral edema, it’s important that we review the associated risk factors as well as the proposed mechanisms. It is important to know that the available data we are about to review comes from retrospective studies as well as case reports and case series and not from randomized control trials.
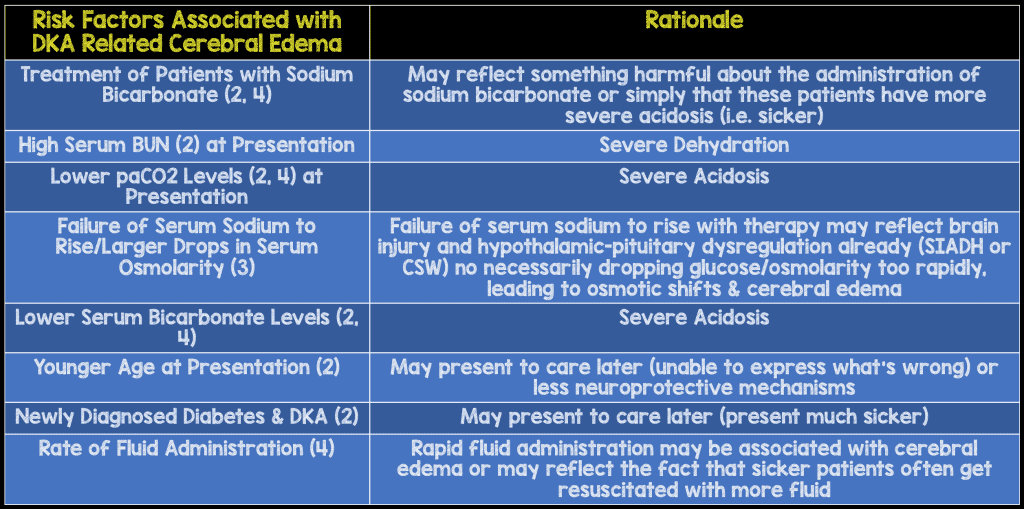
Associated Risk Factors:
The above risk factors have been cited in retrospective analysis of children who have developed DKA related cerebral edema. Of the above risk factors, it appears that the severity of acidosis as well as dehydration seemed to be the most important risk factors.
Proposed Mechanisms of Pediatric DKA Related Cerebral Edema:
Osmotic Theory: Patients with DKA are exposed to high serum osmolarity secondary to elevated glucose levels. As a result, fluid shifts from the intracellular space and into the serum (so out of brain cells) leading to intracellular dehydration. As a protective mechanism, the brain starts to produce osmoles that remain intracellularly to increase cellular osmolarity and protect against further cellular fluid losses.
As patients with DKA are treated with insulin, their serum glucose and therefore their osmolarity begins to decrease. With this decrease in serum osmolarity, fluid can begin to shift from the lower serum osmolarity and into brain cells specifically astrocytes, that now, due to the production of intracellular osmoles, have a higher osmolarity than the serum. This is why many DKA protocols call for a gradual drop in patient’s serum glucose to prevent rapid changes in serum osmolarity. The intracellular osmoles are slow to resolve, so the resuscitation process should also be slow as to not cause rapid fluid shifts intracellularly. Therefore, many protocols also call for gentle hydration over 48 hours to avoid rapid shifts of fluid intracellularly possibility causing cerebral edema.
Arguments against this theory have been that children have developed DKA related cerebral edema even prior to treatment and fluid administration, and despite protocols focused on slower fluid resuscitation the incidence of cerebral edema has remained the same.
Cytotoxic Edema: Cytotoxic edema is due to ischemia from hypoperfusion and the classic example is in ischemic strokes. Patients with DKA are at risk for decreased cerebral perfusion and therefore decreased cerebral blood flow from severe dehydration as well as cerebral vasoconstriction as a result of severe metabolic acidosis with respiratory compensation (lower CO2 levels cause cerebral vasoconstriction). Both dehydration (elevated BUN) and severe acidosis have been shown repeatedly in retrospective studies, as risk factors making this theory more plausible.
Vasogenic Edema: Vasogenic edema, as the name implies, is caused by a disruption of the vascular endothelial tight junctions leading to increased vascular permeability and the breakdown of the blood brain barrier (BBB). As a result of the increased vascular permeability and disruption of the BBB, serum fluids and protein leak out the blood vessels and collect in the extracellular compartments leading to cerebral edema. Cerebral hypoperfusion leading to hypoxia and ischemia as described above in the cytotoxic edema theory may lead to disruption of the blood brain barrier and vasogenic edema. But additionally, other factors such as inflammation as well as metabolic factors due to ketone bodies and toxic metabolites may also lead to disruption of the vascular permeability and vasogenic edema.
It is very hard to distinguish between both cytotoxic and vasogenic edema as they often occur together and a combination of both may be responsible for the cerebral edema seen in children with DKA. Perhaps if a patient is also over resuscitated as well, this fluid can lead to further worsening of cerebral edema.
Article: Kuppermann et al. Clinical Trial of Fluid Infusion Rates for Pediatric Diabetic Ketoacidosis. N Engl J Med 2018. PMID: 29897851
Clinical Question: Does composition or rate of IV fluid resuscitation in pediatric DKA have a clinically significant impact on neurocognitive function after recovery from ketoacidosis?
Study Design: this was a prospective, multi center, randomized control trial. Children were randomly assigned to one of four treatment groups in a 2×2 factorial design of 0.9% or 0.45% NaCl crystalloid at rapid or slow rates of administration
Pediatric DKA Treatment Groups:
- Fast 0.45% NaCl = Half the fluid deficit replaced with 0.45% NaCl in initial 12 hours + maintenance fluids. The remainder of the deficit + maintenance fluids replaced during the subsequent 24hrs
-
Fast 0.9% NaCl = Half the fluid deficit replaced with 0.9% NaCl in initial 12 hours + maintenance fluids. The remainder of the deficit + maintenance fluids replaced during the subsequent 24hrs
- Both fast groups assumed a 10% deficit and both received a 10mL/kg 0.9% NS bolus x2
- Slow 0.45% NaCl = Fluid deficit plus maintenance fluids replaced evenly during 48hrs with 0.45% NaCl
-
Slow 0.9% NaCl = Fluid deficit plus maintenance fluids replaced evenly during 48hrs with 0.9% NaCl
- Both slow groups assumed a 5% deficit and both received a 10mL/kg 0.9% NS bolus x1
Population: Children from 13 emergency departments in the Pediatric Emergency Care Applied Research Network (PECARN) from ages 0 – 18 who had the diagnosis of DKA confirmed were polled. After an exclusion procedure and consent, 1,255 patients underwent randomization and were placed in to 4 broad categories (fast rate ½ NS, fast rate isotonic saline, slow rate ½ NS and slow rate isotonic saline) with roughly equal distribution.
Exclusion Criteria:
- Underlying disorders that could affect mentation like concurrent alcohol/narcotic usage, head trauma
- DKA treatment initiated prior to consent for study
- Children with GCS less than 11 at the time of initiation of treatment
Outcomes:
- Primary outcome: Number of episodes of confirmed decline in Glasgow Coma scale to less than 14
-
Secondary outcomes:
- Incidence of clinically apparent brain injury
- Short term memory issues (measured by forward and backward Digit-span scores) during DKA episodes
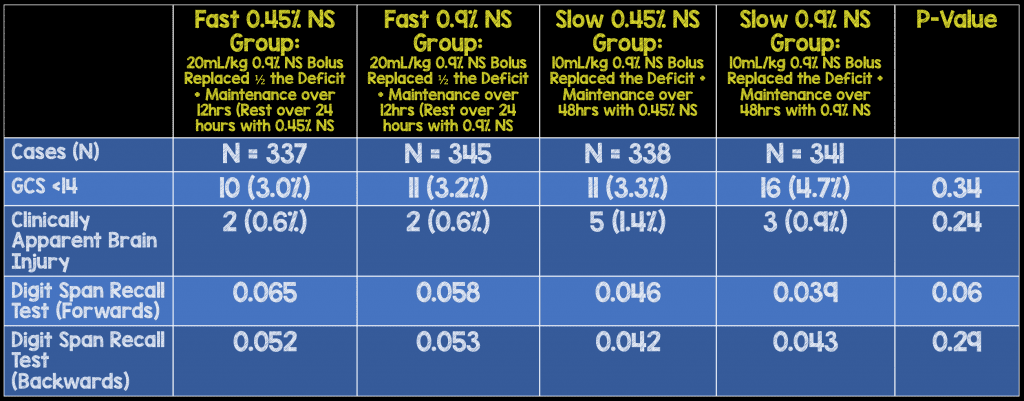
Critical Results:
- 1,389 distinct episodes of DKA were evaluated in 1,255 patients, but only 1361 episodes of DKA were included in the primary analysis. 132 children had a second episode of DKA and underwent randomization as well.
- There were a total of 48 episodes (3.5%) resulting in a GCS <14 with 22 episodes (1.6%) requiring hyperosmolar therapy for cerebral edema, and 12 episodes (0.9%) of clinically apparent brain injury.
- There were no statistically significant differences in the percentage of episodes among the 4 groups where the GSC decreased to less than 14, the magnitude of decline or duration GCS remained less than 14
- Incidence of a GCS decline <14 & clinically apparent brain injury was actually lower in fast rehydration groups (21 vs 27 & 4 vs 8 episodes respectively),cartier replica but both were not statistically significant
- Memory assessed by forward and backward digit-span scoring did not significantly differ between the 4 groups
- Hyperchloremic acidosis was more common among patient receiving 0.9% NaCl vs 0.45% NaCl and more common in patients receiving fluid at a rapid rate vs slow rate
Study Strengths:
- A large multicenter prospective randomized control trial
- A data and safety monitoring board oversaw the conduct of the trial and included experts in emergency medicine, pediatric critical care, pediatric endocrinology, neuropsychology, and biostatistics. This board convened before enrollment, at three scheduled interim efficacy analyses, and at 4 additional scheduled reviews of safety, enrollment, and follow-up data
- Patients and parents were unaware of treatment group assignments
- Brain injury diagnosis adjudicated by a committee that included 2 pediatric EM physicians, who were unaware of treatment group assignments
- Glasgow Coma scale scores of <14 were confirmed by repeat testing 15min later
- Primary analyses performed according to the intention-to-treat principle. This is a more reliable estimate of the true effectiveness of treatment in a real world setting
- Subgroup analysis was pre-specified prior to enrollment of the study
- There are no previous large-scale studies looking in to rates and composition of IV fluids in pediatric DKA patients
- Appropriate randomization in to 4 subgroups with similar demographic and baseline characteristics
Study Limitations:
- Unable to blind clinicians of the treatment group because of the need to know the fluid protocol for clinical decision making
- Clinically apparent brain injury only occurred in <1% of episodes of DKA, making it impossible to statistically analyze this particular outcome
- Repeat episodes in the same patient were not excluded which decreases power of the study, however episodes of DKA were limited to 2 episodes per patient
- The study does not look into other compositions for rehydration (balanced fluids such as plasma lyte or lactated ringers)
- There was a wide spectrum of ages with the average being 11 years old in both the fast and slow groups. Only 10-12 % of children in these groups were less than 6 years old, which may be the group of children most at risk for the development of cerebral edema.
Discussion:
The first few cases of DKA related cerebral edema were described in young boys in the medical literature (NEJM) in 1967 (5). Since then, > 200 additional cases of cerebral edema in DKA patients have been reported and studied (6). Various theories have been proposed for causes for cerebral edema as we have reviewed above, but without any strong evidence to support one mechanism. It has been taught that slow intravenous fluid administration was one of the hallmarks of management in patients with DKA. It is believed that vigorous fluid administration was either associated or was even the cause of DKA related cerebral edema. Much of this data comes from case studies and case reports from children who have developed cerebral edema. This data may be biased, as many of these children were “sicker” and as a result of their underlying critical illness, may have received increased amounts of intravenous fluids. This was the first randomized control trial exploring the association between the rate and content of intravenous fluids and the incidence of DKA related cerebral edema.
Author’s conclusion: “In this prospective, randomized trial, neither the rate of administration nor the sodium chloride content of intravenous fluids significantly influenced neurologic outcomes of diabetic ketoacidosis in children.”
Our Conclusions:
- I think based on this study and previous studies, the idea that the content and rate of administration of intravenous fluids, as well as the theory that osmotic shifts are the cause of cerebral edema are not well supported.
- Keep in mind; even the “fast” fluid resuscitation group patients ONLY received a 20cc/kg bolus (a standard pediatric IVF bolus) and then ½ their deficit plus maintenance fluids were replaced over 12 hours. This resuscitation strategy was still a relatively cautious one, so one should not conclude that kids with DKA can be “over” resuscitated and fluids do not contribute to cerebral edema.
- This study shows that it may be safe to resuscitate patients faster than what was previously thought, and it therefore seems appropriate to adequately resuscitate your patient with DKA who have clinical evidence of dehydration.
- Conversely one can still argue that a slower resuscitation, which has been done for years, was still equivalent to faster resuscitation protocols. If there is still hesitancy after only one randomized control trial, then the slower resuscitation group performed equally as well as the faster resuscitation group.
Future Questions?
- There was a trend toward improvement in faster treatment groups: 21 episodes of GCS <14 & only 4 episodes of clinically apparent brain injury vs. slower treatment group: 27 episodes of GCS <14 & 8 cases of clinically apparent brain injury (both not statistically significant). In light of these findings and the evidence showing children at highest risk for development of cerebral edema are those severely dehydrated and acidotic, perhaps faster resuscitation in children with DKA may be even safer? Perhaps by more quickly fluid resuscitating these children (not over resuscitating) and improving there cerebral blood flow we may be actually decreasing the risk of developing vasogenic or cytotoxic edema?
- Perhaps the use of balance fluids for resuscitation may be of benefit in more quickly reversing the metabolic acidosis, which is driving our patients hypocapnea causing cerebral vasoconstriction and cerebral perfusion. A bolus of 0.9 NS often decrease pH even further leading to a worsening metabolic acidosis. Most people talk about using balanced fluids to simply minimize the development of hyperchloremic acidosis later in the patient’s course of illness, which often prevents many children from transitioning to SQ insulin sooner due to persistent non-gap acidosis. However using balanced fluids to initially resuscitate may restore cerebral perfusion by (1) volume expansion, (2) improving acidosis, and (3) perhaps minimizing the inflammatory effects that can be seen with hyperchloremia.
Guest Post Co-Written By
Frank Lodeserto, MD
AND:

References:
- Kuppermann et al. Clinical Trial of Fluid Infusion Rates for Pediatric Diabetic Ketoacidosis. N Engl J Med 2018. PMID: 29897851
- Glaser N, et al. Risk Factors for Cerebral Edema in Children with Diabetic Ketoacidosis. N Engl J Med. 2001. PMID: 11172153
- Hoorn EJ, et al. Preventing a Drop in effective Plasma Osmolality to Minimize the Likelihood of Cerebral Edema During Treatment of Children with Diabetic Ketoacidosis. J Pediatr 2007. PMID: 17452217
- Mahoney CP, et al. Risk factors for developing brain herniation during diabetic ketoacidosis. Pediatr Neurol 1999. PMID: 10580884
- Young E, et al. Cerebral edema with irreversible coma in severe diabetic ketoacidosis. N Engl J Med 1967. PMID: 4959859
- Rosenbloom, A. L. The Management of Diabetic Ketoacidosis in Children. Diabetes Therapy PMID: 22127748
For More on this Topic Checkout:
- Ben Lawton & Damian Roland at Don’t Forget the Bubbles: Sweet and Salty – Fluids in DKA
- Sarah Medeiros & Julia Magana at EM Pulse: DKA – It’s Not About the Fluids!
- Derek Monette & Michelle Lin at Paneraigmt ALiEM: PEM Practice Changing Paper – Clinical Trial of Fluid Infusion Rates for Pediatric DKA
- Simon Carley at St. Emlyn’s: JC – Fluid Resuscitation in Paediatric DKA
- Justin Morgenstern at First10EM: IV Fluids do not Cause Cerebral Edema in Pediatric DKA (Kuppermann 2018)
- Ken Milne at The SGEM: SGEM #255 – It Don’t Matter Now – Fluid Type and Infusion Rate in Paediatric DKA
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post Pediatric DKA: Do Fluids Really Matter? appeared first on REBEL EM - Emergency Medicine Blog.