Doug and Dennis talk austere management of COVID19 patients with an emphasis on strategies for oxygenation and ventilatory support. The remainder of the post is an massive amalgamation of resources I have been collecting for over a year for my own respiratory refresher. Its alot to take in but if you are looking for something related to airway, oxygenation or ventilation, scroll down and you should have some great rabbit holes to dive down.
On to the Podcast!
We have been trying to get more vent training with the Advanced Special Operations Medical Sergeant Course, Regional Support Medic program and prolonged field care training for a while recognizing that this is a universal weakness for the majority of us SOF Medics. We just don’t do it enough. I had the 6 students go through over 7 hours of vent training in 4 blocks over the course of 9 weeks and we were just getting comfortable with the basics. Most go back to their day jobs and won’t likely touch it again for a long time.
While getting ready for an upcoming class I was invited to take, I wanted to review everything I had found useful for airway and ventilation. There is a lot here but contains all the resources I found most useful…
COVID19 Airway and Vent
Disclaimer: I am not currently taking caring for any COVID19 patients,or any others for that matter, but these resources seem to be helpful to those who are. Recommendations are evolving daily so be sure to check the date on everything in this section…
Infection Control
Use an exhalation filter no matter what airway or vent you are using!
https://vimeo.com/403343413
10th SFG(A) SOCRATES Training:
EMCrit always has some great resources like this 4 Apr webinar…
https://emcrit.org/emcrit/avoiding-intubation-and-initial-ventilation-of-covid19-patients/
This deals with other, non-invasive positive pressure solutions such as COVID19 CPAP: https://emcrit.org/pulmcrit/cpap-covid/
This is the comprehensive PulmCrit/EMCrit Internet Book of Critical Care post if you have the time: https://emcrit.org/ibcc/COVID19/
Bill Cantrell also has some great resources on ResusMed: http://www.resusmed.com/2020/03/30/protected-airway-management/
You could try awake proning
CPAP machines (and some kind of viral exhaust filter) could buy time or prevent getting them on a vent. Most of the stuff I have read says that COVID19 Patients on vents have anywhere from a 50% to 90% mortality even with properly trained and equipped ICU teams. A SOF medic probably shouldn’t intentionally be trying to do any of this without very close oversight or in extremis. Like I said, it would be a bad day for the best of us.

PEEP valve with viral exhalation filter for COVID19 patients from Bob Hesse

BVM with PEEP valve with viral exhalation filter for crashing COVID19 Patients from Bob Hesse
Visit the Society of Critical Care Medicine for some great resources
including this
Current Airway Guidelines
Current Role 2/3 JTS Clinical Practice Guideline on Airway Management
Original PFC WG Airway recommendations (April, 14)
Original PFC Airway Video:
PFC Airway Presentation Slides
SPO2
Next Generation Combat Medic Embrace the Full Power of your SPO2
PulmCrit-Top 10 Reasons Pulse Oximetry Beats ABG for Assessing Oxygenation
Airway Prep
MSMAID Acronym with Minimum, Better, Best Packing List
EMCRit Airway Positioning and Bougie
Manual Bag Valve Mask
ProlongedFieldCare.org Optimizing Manual Ventilation
PEEP Valves
ProlongedFieldCar.org PEEP Valves
EMCrit Awake Proning
https://emcrit.org/wp-content/uploads/2020/04/COVID-CARP-Protocol-postable.pdf
Cric
Intubation
RSI technique and checklist 2016
EMCrit-Dissociated Awake Intubation
EMCrit Ketamine Facilitated Intubation
ETCO2
Post Intubation
Tube Depth
Cuff Pressure
ProlongedFieldCare.org Cuff manometer
PulmCrit-Liberating the Patient with no Cuff Leak Extubation
SAVent
No.
It has no PEEP or adjustability. If you do end up using it, do it for no more than 20 minutes at a time and then take them off in order to use a BVM with a PEEP valve.
The only time I would use this is for the extreme emergency where you need to bag a patient but must also do something else like drive and really need more hands.
SAVeII
The SAVE2 is underpowered for most situations. Patients would almost certainly need to be paralyzed (especially if ketamine were used which would maintain the patient’s own drive) as it is not a smart vent and they would constantly be breathing over it causing dyssynchrony, stacked breaths, agitation, pop-offs and more. It may work for the initial managemwnt of compliant COVID19 patients but as they descend into classic ARDS, they would need to be switched over to a fully capable vent.
Ragged Edge Blog Post by RT Wayne Trainer: SAVEII Save Who?
MOVE Vent Patient Assessment Tool
SAVe II Ventilator Easy Set Up Guide
Quote from a well respected intensivist..
“I spoke with the SAVE folks themselves at MHSRS. They said it was never designed to provide mechanical ventilation support and never intended as a ventilator for SOF. “If you need a ventilator,” their guy said, “buy a ventilator.” Both SAVE 1 and 2 are mechanical bagging devices. They do not supply enough flow to generate meaningful tidal volumes for adult trauma patients. This results in a) under ventilating and under oxygenating a sedated, PARALYZED patient (because, as you’ll see, spontaneous breaths on the SAVE are bad) or b) when the patient breathes spontaneously, their natural tidal volume exceeds the flow the machine can provide, triggering a pop-off valve that entraps ROOM AIR, to provide the missing flow/volume demanded by the patient. So, if you are lucky enough to have supplemental O2, a spontaneously breathing patient on a SAVE 1 or 2 will regularly dilute that with 21 % FIO2… A bag mask with a PEEP valve provides FAR greater respiratory therapy than any SAVE machine.”
We eventually need a better vent.
Zoll/Impact Eagle 731 Vent
Great YouTube Playlist for 731 training: https://www.youtube.com/playlist?list=PL6mgSPXJ-4is0NRTMC5ecXvUKdjEMvwYK
Zoll Impact Eagle 731 Vent Easy Set Up Guide
Zoll/Impact 731 ventilator Cheat Sheet
Old Impact Eagle 752 Vent
Old Eagle Impact 752 Ventilator Cheat Sheet (Rule of 5s
Next Generation Combat Medic 5 part Ventilator Series
Next Generation Combat Medic Intro to Vents
Next Generation Combat Medic Applied Ventilator Theory
Next Generation Combat Medic Ventilatory and Respiratory Control
Next Generation Combat Medic Ventilator Theory
Next Generation Combat Medic Vent Practicalities
Even More Vent Stuff!
ARDSNet Protocol for ideal bodyweight calculation
Scott Weingart,s EMCrit Dominating the Ventilator Handout
EMCrit-RACC Vent And PREVENT Episodes
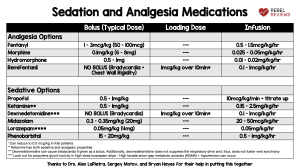
Analgesia and Sedation


Blood Gas
PulmCrit-Converting a VBG into an ABG
Misc Airway
EMCrit How do you know you are actually good at airway management
PulmCrit-Mastering the Dark Arts of BiPAP & HFNC
PulmCrit-Fighting Refractory ARDS with Physiologic Jiu Jitsu
Proning
Our PFC Proning Podcast Episode 53
Early Prolonged Patient Proning nejmoa1214103
Splitting Vents Between Patients?!
Shared vent for mult pts_2006.05.009
Joint-Statement-Patients-Single-Ventilator
Don’t try and split a SAVE2. Here is my SAVE2 Math if thinking about splitting it between 2 patients:
Let’s pretend we have a 60y/o 5’9″ 230lb male as our first patient.
Push the button corresponding with the height of our height of our imaginary patient of 5’9″ which calculates the ideal body weight and gives us a tidal volume of 420mL if we use the lower 6mL/Kg of the ARDSNet recommendations.
Now we have to set rate. Our patient presumably needed the ventilator due to COVID19 and his inability to satisfy his oxygenation and ventilation and is now in respiratory distress on the verge of failure. He is breathing fast and shallow with fits of coughing so we pick a slightly higher rate of 16 to begin with.
420Vt x 16RR = 6,720Ve
The max minute minute ventilation for a SAVE2 is 8000mL. No more. Patient number 2 would have less than 1300 minute volume left at the lowest settings for the first.
If you are having issues with oxygenation and low sats we traditionally can adjust PEEP and/or oxygen if we have it. COVID Patients seem to be hypoxemic need more O2.
For issues with high ETCO2 we can adjust volume and rate.
Increasing any of those variables would use even more of the limited minute volume.
It just wouldn’t work.
Documentation
MOVE Vent Patient Assessment Tool




What would you add???
Vasopressors
https://emcrit.org/emcrit/push-dose-pressor-update/
https://rebelem.com/one-more-update-on-using-peripheral-intravenous-piv-vasopressors/
Responding as a Medical Volunteer?
Advice on Integrating SOF Medics Into Existing or Developing Civilian Medical Systems During Disasters
Here are some thing I learned during Hurricane Katrina and have refined over the last 15 years of being a Medic…
1. Remember that it is not about you. You are there to provide support, in a supporting role, as a support guy, volunteering to do support things. Defer to expertise. Read about HROs while you’re thinking about it.
2. Watch out for yourself and know when to tap out. It is easy to get sucked in to working 24 hours straight… and then be worthless for the next 2 days. This is a marathon. Pick a predetermined stopping point and stick to it.
3. Watch out for those around you. If you notice a fellow volunteer trying to muscle through a triple shift making bad decisions, take them with you when you get a break and talk to them. They will get really tired and crash. Night night. Soft power win.
4. Constantly ask yourself if you are making it better. The situation, the patient, the family, the process…
5. There are laws and protocols but often there is an unofficial process hindering everyone in the background. What can you fix right now? Tomorrow? Next disaster? Step back and observe when you can. Write down what you observe and make sure the right decision maker gets it.
6. Don’t bang your head against an immovable object. Go around it. If you can’t do something because of legal ramifications or logistical constraints, what can you do?
7. Nothing is beneath you. Everything needs to get done so look for work, especially that which no one else wants to do. Bottlenecks can be caused by the most mundane things so clean up, move things and do the dirty jobs.
8. No one wins an argument in public in the heat of the moment. Pick your battles and the ground which fought on. Do you really want to influence a change in behavior or just prove to everyone you are an asshole?
9. Know what you can do, what you can’t and what you shouldn’t. Your scope of practice changed the minute you left the gates of a military installation. Who is your medical director? Who’s license you are working under? What protocols are they using? Who is liable? Are you willing to lose your house over it?
10. Know when to take charge. Is a patient crashing or in imminent danger? How can you temporize the situation and get them out of the weeds?
-Paul Loos, 18D
