 You have just secured the endotracheal tube following an uneventful intubation of a moderately ill patient in your emergency department. They had a normal pre-intubation blood pressure. As you are calling the admit in to the ICU the patient’s nurse tells you that the BP is now in the 70’s.
You have just secured the endotracheal tube following an uneventful intubation of a moderately ill patient in your emergency department. They had a normal pre-intubation blood pressure. As you are calling the admit in to the ICU the patient’s nurse tells you that the BP is now in the 70’s.
NOW WHAT?
- Blindly give a half gallon of saline and stay in your seat.
- Get up, walk to the patient’s room, and consider the possible causes of post intubation hypotension.
There is a laundry list of potential pathologies in play, some of which require time critical interventions. Option 2 is the only acceptable option for evaluating a patient with post intubation hypotension.
Here is a crowd sourced approach that will allow most etiologies of post intubation hypotension to be identified: The AH SHITE mnemonic is something that you can quickly run through en route to the patient’s room, or at the bedside. This is intended as a starting point to the evaluation of the patient with post intubation hypotension.
Treatment of these issues will not be discussed in detail. Thanks to @precordialthump and @pbsherren for helping me fine tune the list and force the mnemonic.
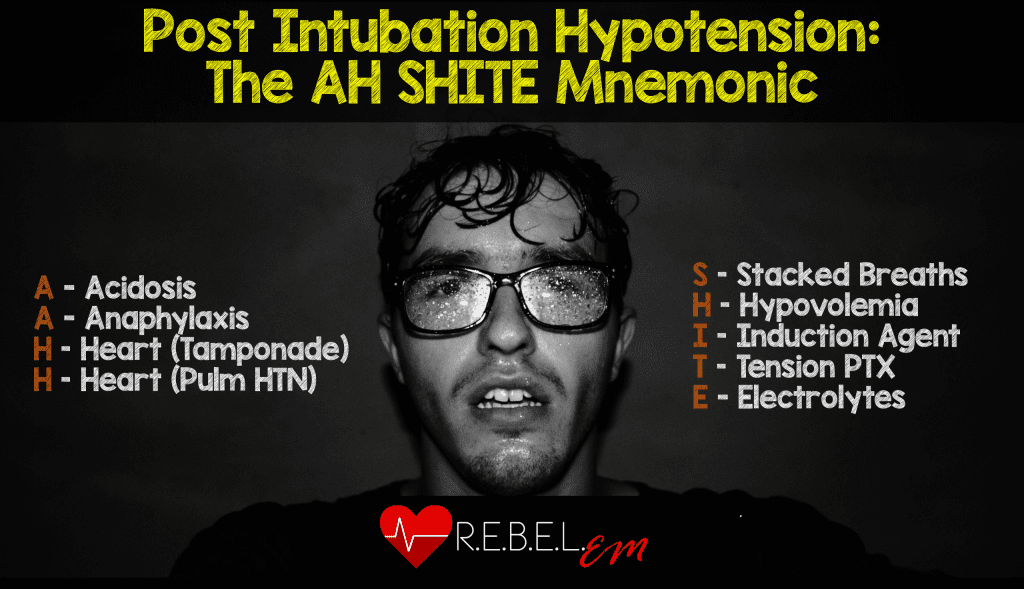
A Acidosis
Patients with profound metabolic acidosis typically have a high minute ventilation, until they become fatigued and then their pH can drop. Post intubation ventilator settings need to provide minute ventilation that approximates pre-intubation levels. One way of ensuring this is to check a pre-intubation ETCO2 and to then aim for this number with a well planned post intubation ventilation strategy. 8cc/kg tidal volume (upper range of ARDSNET vent strategy) and a high RR (30’s) with close attention to post intubation gases is a good start.
Does giving bicarb to profoundly acidotic patients on the vent help?
Henderson Hasselbalch equation:
H+ + HCO3- <—> H2O + CO2
This equation is an equilibrium, any increase in H+ concentration will tip the equation to the right, and generate more CO2. This will typically cause tachypnea, unless the patient is profoundly fatigued. Adding bicarb will produce more CO2, if the patient is already being ventilated at a maximum minute ventilation this will not be able to be increased, and without removing the CO2 from the system, the pH will not change.
Sodium bicarbonate in the treatment of subtypes of acute lactic acidosis: physiologic considerations.
- Anesthesiology. 1990 Jun;72(6):1064-76. PMID: 2161621
- When isotonic sodium bicarbonate was added to whole blood in a (closed) system where generated C02 could not escape, PCO2 increased and pH was unchanged. pH only rises when CO2 is eliminated.
- If C02 elimination cannot keep pace with increased C02 generation, administration of bicarbonate during acidemia produces hypercarbia (respiratory acidosis) with little net improvement in pH.
Sodium Bicarbonate for the treatment of Lactic Acidosis.
- Chest 2000; 117(1): 260 – 7. PMID: 10631227
- 18 animal studies: no improvement with bicarb
- 2 human studies, average lactates 7-8mmol/l
- pH improved by 0.14, and 0.05
- No improvement in hemodynamic parameters / response to pressors.
Giving bicarb does pose a risk of impaired oxygen delivery via an increased hemoglobin affinity for oxygen. This is seen in studies on healthy volunteers. A downstream effect from this is that lactate concentrations can increase. This has been seen in studies on animals with hypoxic lactic acidosis.
A Anaphylaxis
Anaphylaxis to ketamine and etomidate is extremely rare. There are only sporadic case reports of anaphylactoid reactions to each of these agents. Neuromuscular blocking agents are divalent molecules that make it easier for anaphylaxis to occur, even in the setting of no previous exposure. (See REBEL EM post in Anaphylaxis to NMB agents)
Anaphylaxis is more common with rocuronium and succinylcholine than with atracurium.
- Anesthesiology. 2015 Jan;122(1):39-45. PMID:25405395
- This was a retrospective, observational cohort study of intraoperative anaphylaxis to NMBDs at two Auckland, NZ hospitals between 2006 and 2012.
- All cases of suspected perioperative anaphylaxis were referred to the same allergy clinic. These were high grade anaphylaxis events, including profound hypotension, and intraoperative cardiac arrest.
- 92,858 anesthetic cases involving new exposures to NMB’s. 21 patients with anaphylaxis were confirmed out of 89 patients referred to the allergy clinic.
- Rates:
- Sux: 1:2080
- Roc: 1:2499
- Atracurium: 1:22451
H Heart:Tamponade
Consider cardiac tamponade in both traumatic and medical presentations. Penetrating chest trauma should be an obvious trigger to perform bedside cardiac ultrasound. Elderly patients on anticoagulants with minor falls, and end stage renal disease patients may have occult / borderline tamponade that only declares itself after a change to positive pressure ventilation.
Timing of tracheal intubation in traumatic cardiac tamponade: a word of caution.
- Resuscitation 2009 Feb;80(2):272-4 PMID: 19059695
- Authors suggest raising the threshold for intubation, and preparing for immediate relief of tamponade after intubation. Consider awake intubation strategy without interrupting spontaneous ventilation.
H Heart: Pulmonary Hypertension
Patients with known severe pulmonary hypertension are a nightmare to intubate. Hypervolemia, hypoxia, and hypercarbia are known to worsen their right heart function. Fluid boluses are unlikely to help an overloaded, distended right ventricle, and may worsen LV impingement.
Pulmonary Hypertension and right ventricular failure in emergency medicine.
- Annals of Emergency Medicine Dec 2015; 66(6):619-28 PMID:26342901
- Give norepinephrine, and treating whatever worsened the Pulmonary Hypertension may help.
S Stacked breaths / Autopeep
Patients with obstructive lung pathology who are not completely exhaling prior to the next breath being initiated can progressively develop air trapping, this can lead to increased intrathoracic pressure that can decrease venous return overtime, and cause hypotension, and eventual arrest.
Occult positive end-expiratory pressure in mechanically ventilated patients with airflow obstruction: the auto-PEEP effect.
- Am Rev Respir Dis. 1982 Jul;126(1):166-70. PMID: 7046541
- Alveolar pressure can remain positive throughout the ventilatory cycle of intubated patients with airflow obstruction. Abnormally compliant lungs transmit a high fraction of alveolar pressure to intrathoracic vessels so these effects may be exaggerated in patients with chronic obstructive pulmonary disease.
- Failure to recognize the hemodynamic consequences of auto-PEEP may lead to inappropriate fluid restriction or unnecessary vasopressor therapy.
H Hypovolemia
Hypovolemia from profound shock states such as hemorrhage, sepsis, and anaphylaxis should be reasonably easy to identify. Occult hypovolemia can be unmasked by the physiologic insult that occurs when patients are switched from spontaneous ventilation to positive pressure ventilation. With the increase in intrathoracic pressure that accompanies positive pressure ventilation any patient with low venous pressures / low pre-load may develop hypotension. Adjusting PEEP settings, and giving a bolus of an appropriate resuscitative fluid will help.
I Induction Agent
Propofol gets a bad rap for being blamed as the only agent capable of causing post intubation collapse. Any sedative agent that takes away an individual’s conscious drive to survive could potentially result in post intubation collapse; Weingart has described this as the ‘nine inch nails to Bob Marley transformation’. (See intubating the patient in shock from SMACC 2013). Decreasing the dose of sedative, and having pressors / push dose pressors ready could help to mitigate this.
T Tension Pneumothorax
Consider tension pneumo in any patient with obstructive lung disease that has increased airway pressures. Rather that blindly needling the chest of these patients, use ultrasound to confirm whether a pneumothorax is present. This will avoid inadvertently causing a pneumothorax in a patient with normal lungs that may have an alternative explanation for their hypotension.
E Electrolytes
Succinylcholine has a well known set of contraindications due to the risk of succinylcholine associated hyperkalemia. Major burns, crush injuries, and end stage renal disease patients are typically rather obvious. Occult contraindications include those patients with histories of malignant hyperthermia, previous stroke / spinal cord injuries, or those with prolonged ICU stays. Several case reports exist of patients who have had profound hyperkalemia without obvious risk factors. In the absence of an alternative explanation for hypotension, and especially in the setting of any rhythm change consider checking a potassium level, or empirically treating with Calcium.
Cardiac Arrest From Succinylcholine-Induced Hyperkalemia
- Am J Health Syst Pharm. 2003;60(7) PMID: 12701553
Summary:
Anticipate that intubation can worsen underlying physiologic parameters, and can cause some intubation specific causes of hypotension. Anticipating post intubation hypotension and being ready to correct specific causes is an essential part of any intubation.
Transform your mantra for post intubation hypotension evaluation from Resuscitate, Intubate, Panic like #$@#, to Resuscitate, Intubate, Anticipate.
Remember this sage advice from Louis Pasteur: ‘Fortune favors the prepared mind’. The better you plan your intubation (see Salim’s HOP killer series) the less likely you will be dealing with post intubation hypotension.
Post Peer Reviewed By: Salim Rezaie (Twitter: @srrezaie)
The post Post Intubation Hypotension: The AH SHITE mnemonic appeared first on REBEL EM - Emergency Medicine Blog.
