
 Background: Despite continued focus on equity in healthcare, it has yet to be realized in the United States. Healthcare can be considered a microcosm of society where resources are not allocated fairly among the population. A recent editorial in the NEJM demonstrates that even equipment designed to give objective information can harbor important biases. Pulse oximetry is a diagnostic tool that is ubiquitous in hospitals. Triage and oxygen therapy administration decisions are made based on the readings from pulse oximetry. The development and validation of this tool was not performed in racially diverse populations but how this impacts the obtained information is unknown.
Background: Despite continued focus on equity in healthcare, it has yet to be realized in the United States. Healthcare can be considered a microcosm of society where resources are not allocated fairly among the population. A recent editorial in the NEJM demonstrates that even equipment designed to give objective information can harbor important biases. Pulse oximetry is a diagnostic tool that is ubiquitous in hospitals. Triage and oxygen therapy administration decisions are made based on the readings from pulse oximetry. The development and validation of this tool was not performed in racially diverse populations but how this impacts the obtained information is unknown.
Paper: Sjoding MW et al. Racial Bias in Pulse Oximetry Measurement. NEJM 2020. PMID: 33326721
Clinical Question: How well do pulse oximetry readings correlate with arterial oxygen saturation readings on blood gas across white and black patients?
What They Did:
- Analyzed paired pulse oximetry readings of oxygen saturation and arterial oxygen saturation from ABGs
- All evaluations were performed within 10 minutes of each other
- Limited analyses to measures of ABGs that included carboxyhemoglobin and methemoglobin
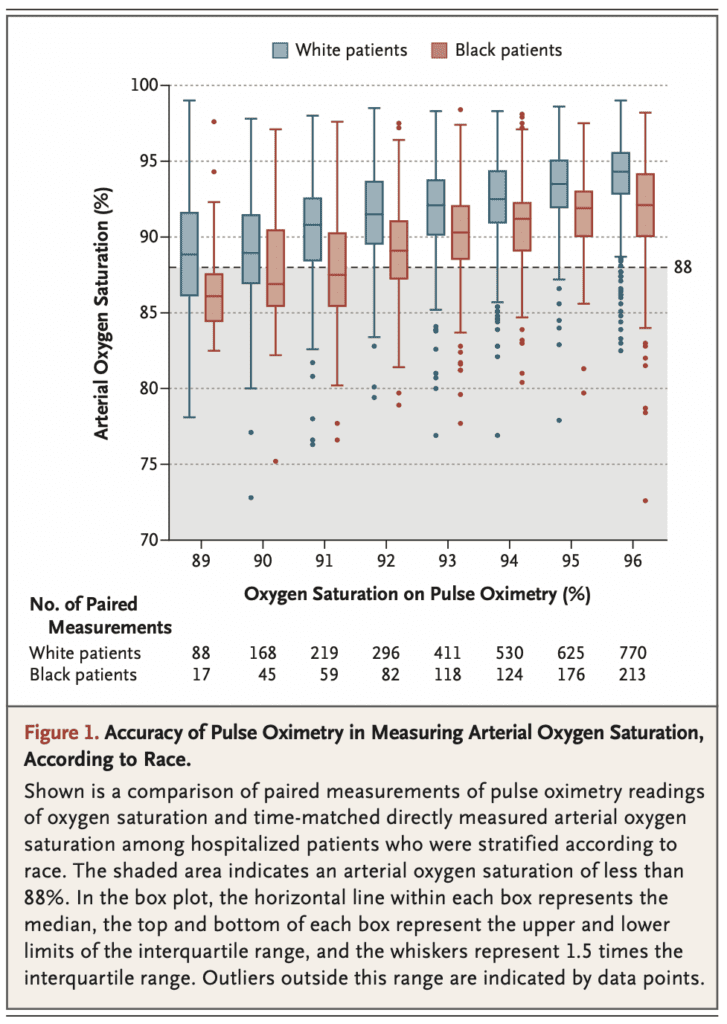
Outcomes: Occult hypoxemia (ABG O2 sat <88% despite an O2 sat of 92 to 96% on pulse oximetry)
Inclusion:
- Adult inpatients receiving supplemental oxygen at the University of Michigan and patients in the ICU wards at 178 hospitals
Results:
-
University of Michigan Cohort
- Analyzed 10,789 pairs of oxygen saturation by pulse oximetry and arterial oxygen saturation in ABGs
- 1333 white patients
- 276 black patients
- Occult Hypoxemia:
- White patients: 99/2778 (3.6%; 95% CI 2.7 to 4.7)
- Black patients: 88/749 (11.7%; 95% CI 8.5 to 16.0)
-
Multicenter Cohort
- Analyzed 37,308 pairs of oxygen saturation by pulse oximetry and arterial oxygen saturations in ABGs
- 7342 white patients
- 1050 black patients
- Occult Hypoxemia:
- White patients: 546/8795 (6.2%; 95% CI 5.4 to 7.1)
- Black patients: 160/939 (17.0%; 95% CI 12.2 to 23.3)
Discussion:
- Peripheral perfusion could lower accuracy of oxygen saturation values, so the authors adjusted for age, sex, cardiovascular score on SOFA score in the University of Michigan cohort
- Black patients had ≈3x the amount of occult hypoxemia not detected by pulse oximetry compared to white patients
- The authors appropriately note that not all black patient who have a pulse oximetry value of 92 to 95% have occult hypoxemia
- Pulse oximetry technology, and more broadly, medications and any medical technology, must be tested in multiple racial/ethnic groups is critically important in developing medical technologies
- IMPORTANT TO NOTE: University of Michigan cohort all on supplemental oxygen and the multicenter cohort were all in the ICU which could limit generalizability to the ED
- FOOD FOR THOUGHT: We don’t want to do unnecessary ABGs on patients, but we also don’t want to miss occult hypoxemia. Looking at the figure from above, when pulse oximetry reads 92 to 93% or less in black patients consider either watching patients in the hospital for observation (instead of discharging home) OR shared decision-making strategy in getting ABGs to ensure we are not missing occult hypoxemia (All patients will not need ABGs as this is a painful procedure and does have some risk associated with it). Additionally as brought up in the discussion below, looking at the figure we can see that pulse oximetry has a +2% higher reading in black patients vs white patients across all readings.
-
ADDENDUM (12/21/2020): More thoughts on this topic as I have had discussions online with others…
-
I am unclear which pulse oximeters were being used in this study
-
Across the board there was a +2% higher reading in dark skin compared to light skin patients
-
This won’t impact clinical care until we get down to 92 – 93% or lower readings
-
Author Conclusion: “Our findings highlight an ongoing need to understand and correct racial bias in pulse oximetry and other forms of medical technology.”
Clinical Take Home Point: Pulse oximeters are used every day, but pulse oximetry may be less reliable in people of color by overestimating oxygen saturation in black patients when compared to white patients, especially when pulse oximetry reads 92 to 93% or less in black patients.
References:
- Sjoding MW et al. Racial Bias in Pulse Oximetry Measurement. NEJM 2020. PMID: 33326721
For More Thoughts on This Checkout:
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)
The post Racial Bias with Pulse Oximetry? appeared first on REBEL EM - Emergency Medicine Blog.


