
 Background: The provision of safe and judicious analgesia is an important task for the emergency physician. Recent literature has demonstrated the effectiveness of sub-dissociative ketamine (SDK) in the emergency department (ED) setting (Motov 2015), however concerns regarding increased rates of hemodynamic and psychoperceptual adverse effects have limited application of this analgesic strategy in older populations. As awareness of geriatric oligo-analgesia has risen along with efforts to limit opioid utilization, interest in identifying a data set specific to this population has grown. The authors of this study sought to distinguish the performance and shortcomings of SDK in this unique patient group.
Background: The provision of safe and judicious analgesia is an important task for the emergency physician. Recent literature has demonstrated the effectiveness of sub-dissociative ketamine (SDK) in the emergency department (ED) setting (Motov 2015), however concerns regarding increased rates of hemodynamic and psychoperceptual adverse effects have limited application of this analgesic strategy in older populations. As awareness of geriatric oligo-analgesia has risen along with efforts to limit opioid utilization, interest in identifying a data set specific to this population has grown. The authors of this study sought to distinguish the performance and shortcomings of SDK in this unique patient group.
REBEL Cast Episode 53 – GeriKet – Ketamine Analgesia in Older Adults
Click here for Direct Download of Podcast
The Article: Motov, Sergey, et al. “Intravenous subdissociative-dose ketamine versus morphine for acute geriatric pain in the Emergency Department: A randomized controlled trial.” The American Journal of Emergency Medicine (2018). [Epub Ahead of Print]
What They Did:
- Single-center, randomized double-blind trial of geriatric patients requiring opioid analgesia for acute abdominal, flank, back, or musculoskeletal pain.
- ≥ 65 years old
- Randomized to 0.1mg/kg IV Morphine or 0.3mg/kg IV Ketamine given as 15-minute infusion.
- Rescue analgesia was offered for pain scores ≥ 5 and given as IV fentanyl, 0.5 mcg/kg.
- Patients were evaluated at 15, 30, 60, 90, and 120 minutes.
- Excluded for weight <40kg or >115kg, unstable vital signs, certain comorbid conditions including: acute head or eye injury, seizure, intracranial hypertension, severe COPD, chronic pain, renal or hepatic insufficiency, alcohol or drug abuse, or psychiatric illness.
Outcomes:
- Primary: Pain reduction at 30 minutes.
-
Secondary:
- Need for rescue analgesia (fentanyl 0.5 mcg/kg) at 30 or 60 minutes
- Adverse events in each group
- Adverse events specific to ketamine recorded with Side Effect Rating Scale for Dissociative Anesthetics (SERSDA).
Results:
- 60 total patients recruited (30 patients per group).
-
NO DIFFERENCE in pain score at 30 minutes.
- Pain decreased by 4.8 in SDK group vs 4.0 in Morphine group (not statistically significant).
- Ketamine demonstrated superior pain reduction at 15 minutes.
- NO DIFFERENCE in patients requiring rescue analgesia at 30 or 60 minutes.
-
HIGHER adverse events in SDK group:
- Any adverse effect
- 15 minutes: 86.7% SDK vs 46.7% Morphine (40% difference, 95% CI 18.4-61.6)
- 30 minutes: 73.3% SDK vs 36.7% Morphine (36.7% difference, 95% CI 13.3-60.1)
- Select SDK adverse effects:
- 18/30 (60%) reported dizziness
- 15/30 (50%) reported “feelings of unreality”
- 2/30 (6.7%) reported hallucinations
- Any adverse effect
Strengths:
- Narrowly defined clinical question applied pragmatically.
- All randomized patients available for pre-specified outcome data.
- Thorough adverse effect observation and reporting.
- Medications were given as a 15-minute infusion due to previous evidence demonstrating a reduction in psychoperceptual adverse effects with slow infusion (Motov 2017).
- Preparing pharmacist, research manager and statistician were the only members of the team with knowledge of the study arm to which the participant was randomized, leaving providers, participants, and data collecting research team blinded to the medication received.
Limitations:
- Single-center study at an institution well versed in the use of SDK for analgesia, limiting generalizability of results.
- Convenience sample compounds selection bias, suggested by time for recruitment of nearly two years.
- There were more patients with cancer-related pain in the morphine group (16.7% vs 6.7%), which can be a more difficult pain to manage with opioids alone (i.e. neuropathic pain, pain borne from bony metastases).
- Small sample size (nearly 32% patient refusal) lacks statistical power to detect clinically impactful differences in analgesic efficacy and low-incidence adverse events.
- Power analysis required sample size of 90 (or 45 in each group) to have 83% power to detect a difference in pain score of at least 1.3 at 30min, which was not reached.
- Interestingly, 35.7% of patient refusals were due to patients not wanting to receive morphine. The hesitancy of older individuals to accept opioid analgesics is multifactorial, and has been described previously (Rupp 2004)
- Potential for unblinding due to ketamine-specific reactions including nystagmus and feelings of unreality.
- As nearly 90% of patients in the SDK group experienced any adverse effect, such consistency may have further exacerbated accidental unblinding.
Author Conclusion:
- “SDK administered at 0.3 mg/kg over 15 minutes provides analgesic efficacy comparable to intravenous morphine for short-term treatment of acute moderate-to-severe pain in geriatric ED patients but results in higher rates of psychoperceptual adverse effects.”
REBEL Commentary:
- Ketamine is thought to exert its effects in a dose-dependent manner, providing analgesia at lower doses, sedation at its highest doses, and neuropsychiatric disturbances and dysphoria in the interim range.
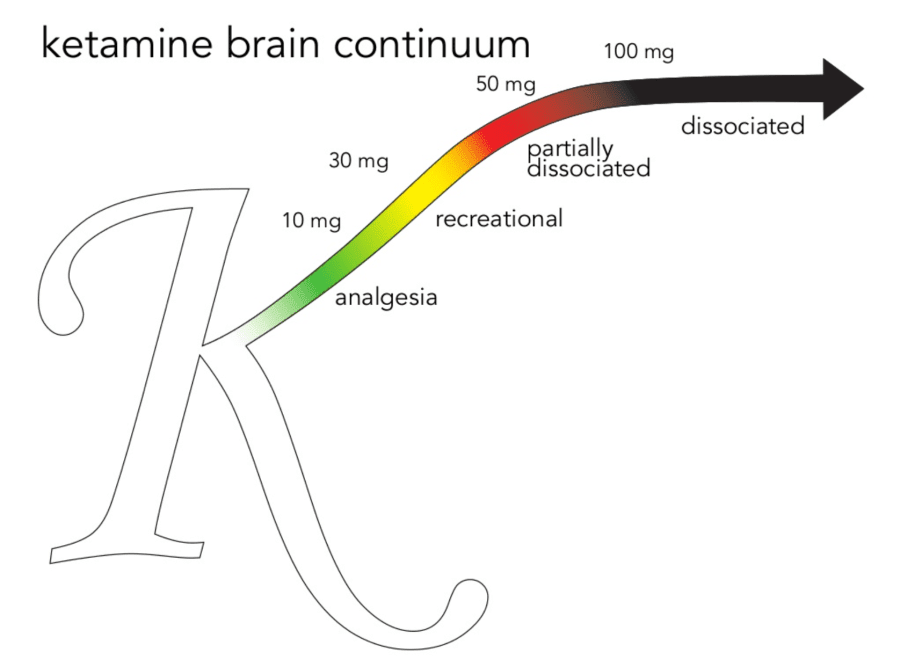
- The shape and relative size of this curve—and thus patient response to SDK—may be influenced by patient-specific factors, including advanced age. Thus, geriatric patients (who in this cohort experienced a high rate of neuropsychiatric disturbance) may respond more appropriately to lower doses of ketamine, or have a narrower window of therapeutic value.
Clinical Take Home Point:
- Ketamine is an effective non-opioid analgesic in the geriatric population, with the tradeoff of markedly increased (minor) adverse events, limiting its application.
- Additional research examining analgesic efficacy and rates of psychoperceptual disturbance at lower ketamine dosing may be useful to further define the role of SDK in the geriatric population.
Lead Author Commentary:

Sergey Motov, MD
Emergency Medicine
Maimonides Medical Center
Brooklyn, NY
Twitter: @painfreeED
I would like to thank REBEL EM and Drs. Pescatore, Swaminathan and Rezaie for an amazing clinical review of our GERIKET trial that compared analgesic efficacy and safety of Sub-dissociative dose ketamine (SDK) to morphine in geriatric patients presenting to the ED with a variety of predominantly acute painful conditions. Their in-depth analysis of limitations of this trial leaves no doubt about the necessity to take them into consideration while interpreting the results of this trial. I would like to add extensive exclusion criteria to the list of limitations as the majority of them are not supported by the current evidence, thus making the study groups even less generalizable to the population seen in the ED on a daily basis.
The very practically crafted conclusion of this review creates a platform for an interesting discussion about the overall utility of SDK in geriatric patients.
The most striking finding of the trial for me was the fact that administration of SDK via a short infusion (over 15 min) resulted in incredibly higher rates of very bothersome adverse effects at 15 and 30 minutes (87% and 73%) that somewhat contradicts to the results from our prior study (Motov 2017) where rates of adverse effects were at about 55%. This is a huge limiting factor to a widespread use of SDK in the ED in geriatric and, frankly, younger patient population despite being comparable (to morphine) analgesic efficacy for short-term analgesia in the ED. There is certainly a possibility that due to age-related changes in drug metabolism, drug-drug interactions and associated co-morbidities, geriatric patients might have a heightened and longer lasting response to SDK with respect to development of adverse effects than their younger counterparts. But, I am starting to believe that 0.3 mg/kg initial loading dose is a rather large dose and 15 minutes infusion time is too short. There is no true dose-finding studies in the EM literature when it comes to managing painful conditions with SDK, but I would strongly suggest to our readers and listeners to start with 0.1-0.2 mg/kg loading dose that is given at least over 30 min. While I am not a big proponent of “start low and go slow” concept when it comes to analgesia in the ED, the severities of unpleasant psycho-perceptual side effects that are associated with the use of SDK in geriatric patients outweigh the analgesic benefits of any degree. Thus, I cannot recommend SDK analgesia in its current and widely acceptable dosing regimen (0.3 mg/kg over 15min) to widespread use in elderly patients in the ED.
And as the authors of this review stated, it is time for a research on a larger scale to find an optimum dose and duration of infusion of SDK for managing pain in the ED.
Sergey Motov, MD
For More on This Topic Checkout:
- Bryan Hayes at The PharmERToxGuy: Ketamine for Acute Geriatric Pain in the ED
- Christina Shenvi at GEMCast: Subdissociative Dose Ketamine in Older Adults? – Maybe
- David Cisewski at EMDocs: Pain Profiles – The GERIKET Trial and Geriatric Analgesia
- Ken Milne at The SGEM: SGEM#233 – Larry in the Den with Kiwis (LDK) – Low dose Ketamine vs. Opioids for Acute Pain
References:
- Motov, Sergey, et al. “Intravenous subdissociative-dose ketamine versus morphine for analgesia in the emergency department: a randomized controlled trial.” Annals of emergency medicine3 (2015): 222-229. PMID: 25817884
- Motov, Sergey, et al. “Intravenous subdissociative-dose ketamine versus morphine for acute geriatric pain in the Emergency Department: A randomized controlled trial.” The American Journal of Emergency Medicine (2018). [Epub Ahead of Print]
- Rupp, Timothy, and Kathleen A. Delaney. “Inadequate analgesia in emergency medicine.” Annals of emergency medicine4 (2004): 494-503. PMID: 15039693
- Motov, Sergey, et al. “A prospective randomized, double-dummy trial comparing IV push low dose ketamine to short infusion of low dose ketamine for treatment of pain in the ED.” The American journal of emergency medicine8 (2017): 1095-1100. PMID: 28283340
Post Peer Reviewed By: Anand Swaminthan, MD (Twitter: @EMSwami) and Salim R. Rezaie, MD (Twitter: @srrezaie)
The post REBEL Cast Ep53 – GeriKet – Ketamine Analgesia in Older Adults appeared first on REBEL EM - Emergency Medicine Blog.
