
 Background: Management and workup of fever in the neonate has been a long-standing challenge. This unique age group is particularly susceptible to serious bacterial infections (SBI’s) despite their clinical “well” appearance. Newborns, specifically those < 60 days of age are considered high risk for SBI’s (urinary tract infections, bacteremia, bacterial meningitis) primarily due to an underdeveloped immune system. As fragile hosts, simple bacterial infections are easily communicated via hematogenous spread, from one system to another. Once bacteremic, spread of infection through their permeable blood-brain barriers is relatively easy. Through a cascade of cellular events, bacteria are able to easily penetrate the CNS, leading to overwhelming meningitis &/or death.[1] Confounding their vulnerability, is the lack of immunizations in the first month of life. If you recall, at birth, newborns are given just their first hepatitis B vaccine. The remainder of baseline immunizations (Pneumococcal, Haemophilus influenzae type b [Hib], Rotavirus, Diphtheria, tetanus & acellular Pertussis [DTap], and Polio) are traditionally not given until 6 weeks – 2 months of age.[2] Thus infants in the < 60 day age range are dependent on their mothers’ antibodies for protection. Lastly as any clinician who has taken care of a sick newborn can attest, babies at this age rarely manifest an “ill-appearance” until they are critically ill, making their exam in the early stages of bacteremia falsely reassuring. Collectively this makes the workup of fever (38 ℃/100.4 ℉) in this age group particularly challenging.
Background: Management and workup of fever in the neonate has been a long-standing challenge. This unique age group is particularly susceptible to serious bacterial infections (SBI’s) despite their clinical “well” appearance. Newborns, specifically those < 60 days of age are considered high risk for SBI’s (urinary tract infections, bacteremia, bacterial meningitis) primarily due to an underdeveloped immune system. As fragile hosts, simple bacterial infections are easily communicated via hematogenous spread, from one system to another. Once bacteremic, spread of infection through their permeable blood-brain barriers is relatively easy. Through a cascade of cellular events, bacteria are able to easily penetrate the CNS, leading to overwhelming meningitis &/or death.[1] Confounding their vulnerability, is the lack of immunizations in the first month of life. If you recall, at birth, newborns are given just their first hepatitis B vaccine. The remainder of baseline immunizations (Pneumococcal, Haemophilus influenzae type b [Hib], Rotavirus, Diphtheria, tetanus & acellular Pertussis [DTap], and Polio) are traditionally not given until 6 weeks – 2 months of age.[2] Thus infants in the < 60 day age range are dependent on their mothers’ antibodies for protection. Lastly as any clinician who has taken care of a sick newborn can attest, babies at this age rarely manifest an “ill-appearance” until they are critically ill, making their exam in the early stages of bacteremia falsely reassuring. Collectively this makes the workup of fever (38 ℃/100.4 ℉) in this age group particularly challenging.
REBEL Cast Episode 64: A Clinical Prediction Rule for Febrile Infants ≤60 Days at Low Risk for Serious Bacterial Infections
For the last few decades we have relied on not just one, but a combination of clinical tools to help us risk stratify patients and determine what workup is needed. Boston, Rochester, Philadelphia criteria to name a few. However many of these rules were not statistically derived and therefore lack a balance of test sensitivity (avoiding missed SBIs) and specificity (preventing overcasting and over treating patients without SBIs). The Step-by-Step approach published in 2016 [3], was a step forward in an algorithmic approach of delineating low risk patients for SBI with higher sensitivity than Rochester, however it also had its limitations. Thus most clinicians remain appropriately conservative particularly in the <60 day age group, and continue to perform comprehensive workups. Being mindful however of potential unnecessary invasive testing (i.e. lumbar punctures) in addition to high costs associated with testing, treatment and hospitalizations, it is a worthy ongoing investigation to find a better approach.
In February 2019, significant strides were made for this neonatal age group in a study published by Nathan Kuppermann and his colleagues in the Febrile Infant Working Group of the Pediatric Emergency Care Applied Research Network (PECARN) group. They published an observational study in JAMA Pediatrics, “A Clinical Prediction Rule to Identify Febrile Infants 60 Days and Younger at Low Risk for Serious Bacterial Infections”. This is perhaps the most exciting study to have been published in the last decade, as they set out to derive and validate a clinical prediction rule to identify febrile infants 0- 60 days who are at low risk for SBIs.
What they did:
-
- A large, prospective observational, multi-center study, using RNA microarray analysis to detect bacteria of SBIs, on data collected from 2011-2013.
-
- SBI was defined as: bacterial meningitis, bacteremia, &/or urinary tract infection.
-
- Fever was defined by rectal temperature of at least 38 ℃ in the ED, in a prior health care setting, or at home within 24 hours.
-
- All patients had blood and urine cultures obtained.
-
- Cerebrospinal fluid (CSF) testing was performed only at the discretion of the treating clinician. To verify that patients whom did not undergo CSF testing, did not ultimately develop bacterial meningitis, families were contacted 8-14 days after discharge for follow-up data collection.
- Data was then divided into a derivation set and a validation set in attempt to create a clinical prediction rule that could predict the presence of a SBI.
Outcomes:
-
Primary: Serious bacterial infection (SBI) defined as:
-
- UTI: catheterized specimen with growth of a single pathogen (50,000 cfu/ml or 10,000-50,000 cfu/ml + abnormal UA); suprapubic catheterized specimen (with > 1000 cfu/ml).
-
- Bacteremia: defined by growth of a single bacterial pathogen in the blood.
- Bacterial meningitis: defined by growth of a single bacterial pathogen in CSF.
-
Inclusion:
-
1896 febrile infants were initially enrolled (1821 with procalcitonin data analyzable and complete assessments for SBI) were included.
-
- 908 randomly allocated into a derivation set
- 913 randomly allocated into a validation set
-
Exclusion:
Any infant who:
-
- Appeared critically ill (determined by the treating clinician)
-
- Who received antibiotics in the preceding 48 hours
-
- Premature birth history (<36 weeks gestation)
-
- Had pre-existing medical conditions
-
- Had indwelling devices
- Had soft tissue infections
Results:
-
- 1896 febrile infants were enrolled (1821 with procalcitonin data analyzable and complete assessments for SBI)
- 1399 (76.8%) of infants had a lumbar puncture (LP) performed (including 871/1266 infants aged 29 – 60 days [68.8%])
-
Serious bacterial infections were diagnosed in 170 infants (9.3%)*
-
- 151 (8.3%) with UTIs
-
- 26 (1.4%) with bacteremia
-
- 10 (0.5%) with bacterial meningitis
-
-
16 (0.9%) had concurrent bacterial infections
-
- 10 of these had UTI + bacteremia
-
- 5 of these had meningitis + bacteremia
- 1 of these had bacteremia + meningitis + UTI
-
-
16 (0.9%) had concurrent bacterial infections
-
- 4 patients had HSV infections, of which 3 were younger than 28 days and had HSV in their CSF
-
- No patients who did not have CSF cultures obtained were later found to have bacterial meningitis.
- *Remainder of patients were excluded as procalcitonin was not obtained.
-
Strengths:
-
- Procalcitonin results were not available to the treating clinicians, which minimizes potential bias of clinician assessment.
-
- Patients who had procalcitonin levels measured were randomly divided into derivation and validation sets, strengthening their overall results.
-
- Authors also performed a sub-cohort analysis of patients ≤ 28 days vs >28 days, allowing them to look at how their rule applied within age-specific parameters.
-
- Given the fact that bacteremia and bacterial meningitis are more invasive SBI’s than UTIs, the authors also performed a sub-analysis to evaluate the rule accuracy, to identify patients with infections (including patients with concurrent UTI and bacteremia or meningitis).
-
- The prediction rule is simple and requires only: Urinalysis (UA), Absolute neutrophil count (ANC), and serum procalcitonin making it easy to use in clinical practice.
-
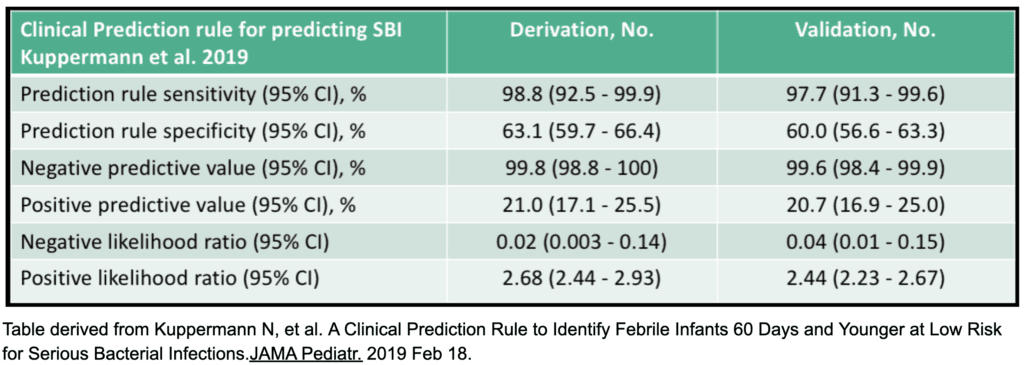
- The prediction rule had high sensitivity for identifying SBI’s and high negative predictive value, while maintaining high specificity.
- The rule does not require CSF data, potentially obviating the need for routine LPs for many young febrile infants, though further confirmation of this is still needed.
Limitations:
-
- This study focused only on serious bacterial infections and did not include serious viral infections (ie: herpes simplex virus encephalitis, enterovirus). Viral panels or seasonally appropriate viral tests (RSV, influenza) were also not included, hence other potentially serious non-bacterial sources of fever were not considered.
-
- Did not include infants 61-90 days.
-
- Convenience samples were obtained on patients only during times when research staff was available.
-
- CSF testing was performed at the discretion of the treating clinician, however to verify that patients discharged from the ED without CSF testing did not have bacterial meningitis, families were contacted by telephone 8 – 14 days after index ED visit.
-
- The lower end of the confidence interval of the Negative Predictive Value in the validation group was 98.4%, leaving a small potential false-negative rate.
-
- No other biomarkers outside of procalcitonin were evaluated.
- In total, only a very small number of patients actually had bacteremia or bacterial meningitis, therefore validation of these findings on cohorts with greater numbers of invasive infections will be needed before implementation.
Discussion:
The PECARN clinical prediction rule is promising in that it demonstrates high sensitivity and specificity for identifying infants with SBIs, while retaining a high negative predictive value, with only a small potential false-negative rate. The rule is relatively simple and easy to use, mandating only three objective data points: UA, ANC, serum procalcitonin. As compared to previous rules, these investigators rounded the numerical cut-offs of ANC (rounded to 4000/uL) and procalcitonin (to 0.5 ng/mL) to make these variables even easier to apply clinically, while still retaining the same sensitivities and only slightly lower specificities.[4]
The most notable factor in this prediction rule is the fact the rule does not require CSF data. A similar prospective study was done also omitting CSF in 2016, referred to as the “Step-by-step” approach. [3] This approach differentiated low/intermediate/high risk infants 22- 90 days by using both objective data [leukocyturia, procalcitonin (> 0.5 ng/ml) ANC (>10,000 mm3) or CRP (>20 mg/L)] as well as the subjective assessment of “ill appearance” using the Pediatric Assessment triangle.[3] Though this was a well conducted multi-center prospective study, that demonstrated high sensitivities (98.9% to detect all SBIs; 92% to detect invasive infections) and proved to have higher negative predictive values than Rochester criteria and the Lab-score outcomes, this study also had its limitations. Primarily its use of subjective criteria of “abnormal pediatric assessment triangle” makes it less reliable to apply clinically. Together with the age range that it was limited to (22 days – 90 days), leaves the youngest of infants (0-21 days) automatically “high risk”, hence not obviating the need for a full septic workup in this cohort.
Neither the Step-by-step approach or the PECARN Clinical prediction rules addressed serious viral etiologies, and HSV encephalitis and enterovirus are certainly not benign. In the PECARN rule, the fact that 0.2% of patients were noted to be positive for HSV infections, and all 3 infants were <28 days of age highlights the continued need for extreme caution in this very young age group.[4] Although this clinical prediction rule seems to be the most straightforward and promising algorithm yet, the decision to omit lumbar puncture needs further external validation.
Authors Conclusions:
Kupperman et al states “We derived and validated an accurate prediction rule to identify febrile infants 60 days and younger at low risk for SBI’s using urinalysis, ANC, and procalcitonin levels. Once further validated on an independent cohort, clinical application of the rule has the potential to decrease unnecessary lumbar punctures, antibiotics and hospitalizations”. [4]
Rebel Take Home Points:
-
-
The PECARN Clinical Prediction rule shows future promise to help risk stratify low-risk patients for SBI. The following variables in particular (if negative or low valued) were associated with a low risk for SBI.
-
- Urinalysis
-
- Absolute Neutrophil Count
- Serum procalcitonin
-
-
The PECARN Clinical Prediction rule shows future promise to help risk stratify low-risk patients for SBI. The following variables in particular (if negative or low valued) were associated with a low risk for SBI.
-
- However further independent validation is still needed before it is reliably applied.
- Until further validation, clinicians need to remain cautious with this age group, particularly conservative in the <28 day olds in whom risks of SBI and severe viral infections are greatest.
References:
- Doran K, Fulde M. et al. Host–pathogen interactions in bacterial meningitis. Acta Neuropathol. 2016; 131: 185–209. PMID:26744349
- Recommended Child and Adolescent Immunization Schedule for ages 18 years or younger, United States, 2019. [CDC Website]
- Gomez B et al. Validation of the “Step-by-Step” Approach in the Management of Young Febrile Infants. Pediatrics 2016; 138(2). PMID: 27382134
- Kuppermann N, et al. A Clinical Prediction Rule to Identify Febrile Infants 60 Days and Younger at Low Risk for Serious Bacterial Infections. JAMA Pediatr. 2019 Feb 18. PMID: 30776077
For More on This Topic Checkout:
- CORE EM: PECARN – Febrile Neonate Decision Rule Derivation and Internal Validation
- DFTB: Fever in Under 60 Days of Age
- First10EM: The PECARN Febrile Infant Study
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post REBEL Cast Episode 64: A Clinical Prediction Rule for Febrile Infants ≤60 Days at Low Risk for Serious Bacterial Infections appeared first on REBEL EM - Emergency Medicine Blog.
