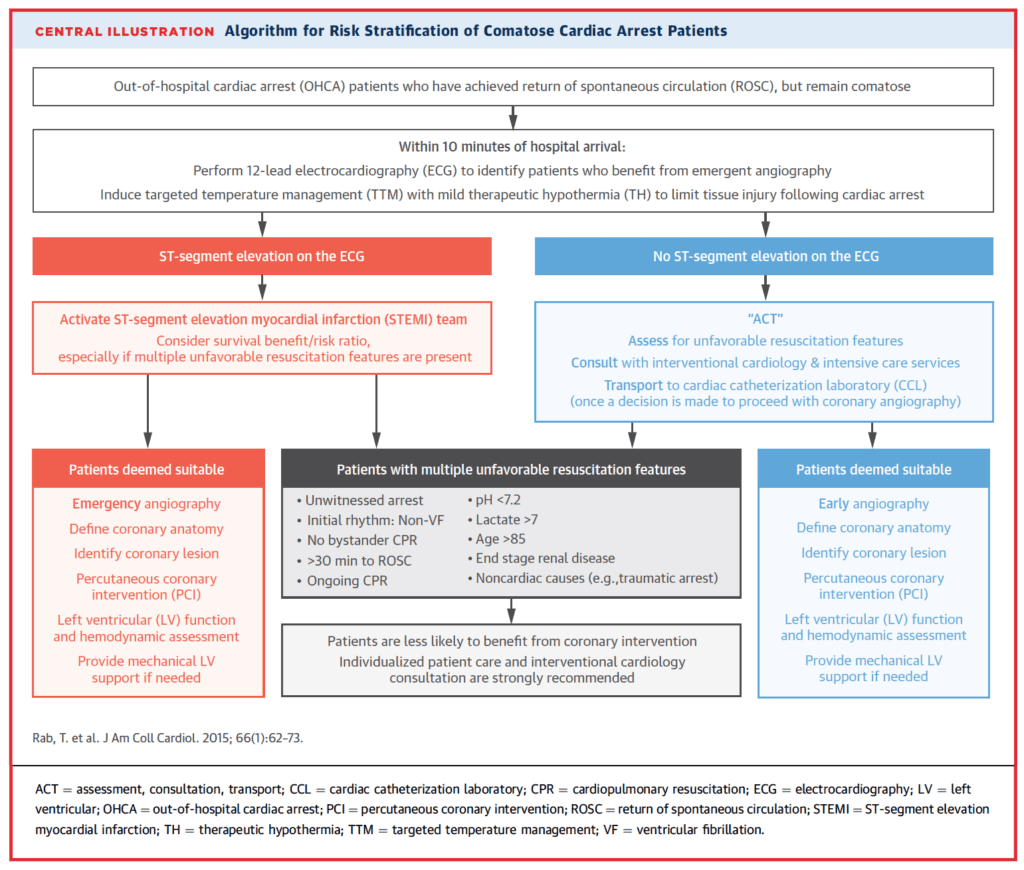
 Background: Post-ROSC care is a multifaceted endeavor that includes targeted temperature management (TTM), vital-organ support, and treatment of the underlying cause of arrest. One of the most common causes of cardiac arrest is acute coronary syndrome. Current European and American guidelines recommend immediate coronary angiography with PCI in patients who present with cardiac arrest due to STEMI. However, in patients with cardiac arrest who do not have STEMI, the role of immediate coronary angiography is still up for debate. The ACC/AHA published a statement in July of 2015 (Covered on REBEL EM) that proposed an algorithm to stratify cardiac arrest patients who are comatose on presentation for emergent coronary angiography and possible PCI.
Background: Post-ROSC care is a multifaceted endeavor that includes targeted temperature management (TTM), vital-organ support, and treatment of the underlying cause of arrest. One of the most common causes of cardiac arrest is acute coronary syndrome. Current European and American guidelines recommend immediate coronary angiography with PCI in patients who present with cardiac arrest due to STEMI. However, in patients with cardiac arrest who do not have STEMI, the role of immediate coronary angiography is still up for debate. The ACC/AHA published a statement in July of 2015 (Covered on REBEL EM) that proposed an algorithm to stratify cardiac arrest patients who are comatose on presentation for emergent coronary angiography and possible PCI.
REBEL Cast Episode 66: The COACT Trial – Coronary Angiography After Cardiac Arrest without STEMI
What They Did:
- Coronary Angiography after Cardiac Arrest (COACT)
- Investigator-initiated, randomized, open-label, multicenter trial that compared immediate coronary angiography vs delayed coronary angiography in patients successfully resuscitated after cardiac arrest and did not have STEMI on ECG
- Patients: Adults >18 years of age having OHCA, with an initial shockable rhythm (VF/VT), unconscious after ROSC, and without STEMI on ECG
- Intervention: Immediate angiography = angiography performed as soon as possible and initiated within 2 hours after randomization
- Comparison: Delayed angiography = Performed after neurologic recovery – in general after discharge from ICU
Outcomes:
- Primary: 90-day mortality
-
Secondary:
- Survival at 90 days with good cerebral performance or mild or moderate disability
- Myocardial injury
- Duration of mechanical ventilation
- Duration of catecholamine support
- Major bleeding
- Occurrence of acute kidney injury
- Need for renal-replacement therapy
- Time to target temperature
- Neurologic status at discharge from the ICU
Inclusion:
- Age >18 years
- OHCA with an initial shockable rhythm (i.e. VT/VF)
- Unconscious (GCS <8) after ROSC
Exclusion:
- STEMI on ECG in ED (Including new LBBB or isolated ST depression in V1 – V3)
- Hemodynamic instability unresponsive to medical therapy (Prolonged (>30min) of SBP <90mmHg at the time of screening)
- Obvious non-coronary cause of cardiac arrest
- Known severe renal dysfunction (GFR <30mL/min)
- Obvious or suspected pregnancy
- Suspected or confirmed acute ICH
- Suspected or confirmed acute stroke
- Known limitations in therapy or Do Not Resuscitate order
- Known pre-arrest Cerebral Performance Category 3 or 4
- >4hrs from ROSC to screening
- Refractory ventricular arrhythmia
- Known inability to complete 90d follow up
Results:
- 552 patients enrolled from 19 centers in the Netherlands
- 538 patients had data available for assessment
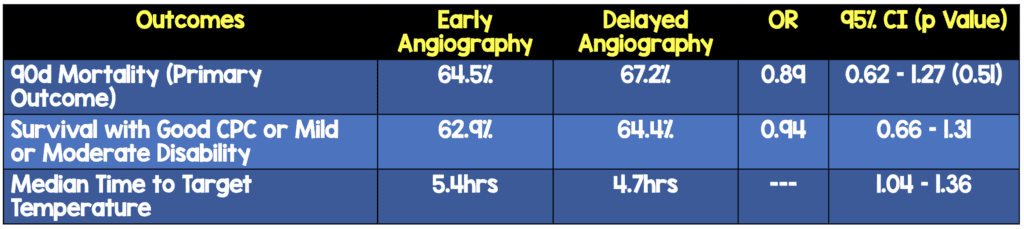
- No difference between other secondary outcomes
Strengths:
- Multicenter, randomized controlled trial
- Well done randomization with a web-based system
- Sponsors of trial had no role in the design or monitoring of the trial, site selection, enrollment of participants, collection, recording, storage, retention, or analysis of data
- Coronary angiography and PCI procedures were evaluated at an independent core laboratory by personnel who were unaware of the treatment assignments
- Independent data and safety monitoring committee of the trial was allowed to recommend an increase in the sample size on the basis of the results of an interim analysis of outcomes in the first 400 patients
- >90% of patients treated with targeted temperature management
Limitations:
- 90 day follow up was obtained by means of a telephone interview conducted at 90 days after randomization with the patient or a family member or were determined from information acquired from the patient’s general physician
- Non-blinded study where physicians knew the assigned group, and this may have influenced subsequent treatment
- Acute unstable coronary lesions were found in less than 20% of the total trial cohort and coronary interventions were performed in <40% of patients
- Power calculation – 85% power to detect a 40% difference. That is a huge difference even for an intervention like cardiac catheterization
- Mortality is a nice hard endpoint, but survival with good neurological outcome would have been a bettr primary outcome
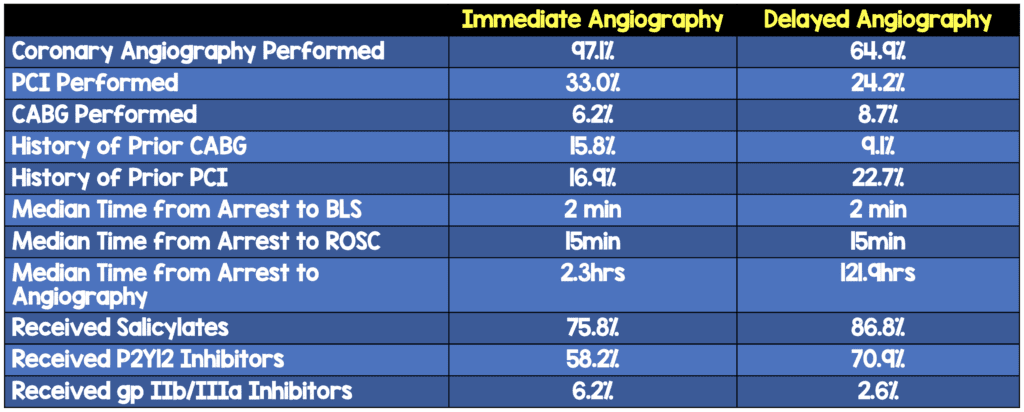
- There are some baseline differences between the two groups though hard to tell if those differences favored one group or the other
Discussion:
- Some Baseline Differences Worth Noting:
- Potential reasons why this trial did not find any survival benefit compared to previous studies:
- Previous studies were observational which may result in selection bias of patients with better prognosis
- The majority of patients included in this trial had stable coronary artery disease, but only a small percentage of them (5%) had thrombotic occlusions. PCI is only effective in patients with thrombotic occlusions
- Majority of non-survivors died from neurologic complications and not cardiac complications
Author Conclusion: “Among patients who had been successfully resuscitated after out-of-hospital cardiac arrest and had no signs of STEMI, a strategy of immediate angiography was not found to be better than a strategy of delayed angiography with respect to overall survival at 90 days.”
Clinical Take Home Point: We agree with the authors conclusions that immediate vs delayed angiography does not affect 90 day mortality in patients with cardiac arrest without STEMI. It is important to note that the majority of patients who had cardiac arrest in this study did not have unstable coronary lesions as the cause of their cardiac arrest (which is the probable reality of this group of patients) therefore the majority of patients who had angiography did not even require PCI. This study is the best evidence we have to date that shows not all cardiac arrests , even those with shockable rhythms need a heart catheterization. So the bottom line for us is:
- Cardiac Arrest + STEMI on ECG = Cath Lab
- Cardiac Arrest + No STEMI on ECG = Dependent on patient factors + conversation with interventional cardiologist (It may be reasonable to not cath immediately and wait 24 – 48hrs before doing a heart cath, if at all)
References:
- Lemkes JS et al. Coronary Angiography after Cardiac Arrest Without ST-Segment Elevation. NEJM 2019. [EPub Ahead of Print]
For More Thoughts on This Topic Checkout:
- EM Lit of Note: Shocked – To the Cath Lab?
- EMCrit: EMCrit Podcast 243 – The COACT Trial on Early vs. Delayed Cath after Cardiac Arrest without STEMI
- The Bottom Line: COACT – Coronary Angiography After cardiac Arrest Without ST-Segment Elevation
- Taming the SRU: Is the Cath Lab the Place to be after V fib VTac Cardiac Arrest?
Support the Show by Paying & Claiming 0.5hrs of CME/CEH by Clicking on the Logo Below
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)
The post REBEL Cast Episode 66: The COACT Trial – Coronary Angiography After Cardiac Arrest without STEMI appeared first on REBEL EM - Emergency Medicine Blog.