
 Background: In patients with ICH, antiplatelet therapy is withheld due to the perceived risk of hematoma expansion. Often, these medications are either not restarted or there is prolonged delays until they are restarted, but the risk of occlusive vascular events might be higher without resumption of antithrombotic therapy. A meta-analysis of observational studies found no difference in the risk of hemorrhagic events and a lower risk of occlusive vascular events associated with antiplatelet therapy resumption after any type of intracranial hemorrhage (ICH); however, randomized trials for antiplatelet efficacy in occlusive vascular disease have excluded patients with a history of intracerebral hemorrhage. Due to the paucity of evidence, no guidelines have strong recommendations about long-term anti-platelet therapy after ICH. The RESTART Trial [1] aimed to address the question of whether or not to start antiplatelet therapy following an intracerebral hemorrhagic stroke.
Background: In patients with ICH, antiplatelet therapy is withheld due to the perceived risk of hematoma expansion. Often, these medications are either not restarted or there is prolonged delays until they are restarted, but the risk of occlusive vascular events might be higher without resumption of antithrombotic therapy. A meta-analysis of observational studies found no difference in the risk of hemorrhagic events and a lower risk of occlusive vascular events associated with antiplatelet therapy resumption after any type of intracranial hemorrhage (ICH); however, randomized trials for antiplatelet efficacy in occlusive vascular disease have excluded patients with a history of intracerebral hemorrhage. Due to the paucity of evidence, no guidelines have strong recommendations about long-term anti-platelet therapy after ICH. The RESTART Trial [1] aimed to address the question of whether or not to start antiplatelet therapy following an intracerebral hemorrhagic stroke.
What they did: This was a prospective, randomized, open-label, blinded endpointstudy that took place in 122 hospitals within the United Kingdom. All patients underwent MRI either prior to randomization or as part of study protocol to confirm or refute eligibility. 537 patients who suffered an ICH while taking antithrombotic agents were randomly assigned to either antiplatelet therapy initiation or strict avoidance of same following hemorrhagic stroke. The antiplatelet medication options were one or more of the following: aspirin, dipyridamole, or clopidogrel. The medications were started within 24 hours of randomization. Recruitment occurred at a median of 76 days (IQR 29-146) following ICH event. Patients were permitted to start or stop antiplatelet therapy regardless of their treatment group if clinically indicated by events following randomization. They were followed for a median of 2 years (Range of 1 – 3 years), and adherence was measured by phone calls, questionnaires for the patients and their primary care physicians, and/or hospital charts.
Outcomes:
- Primary: Fatal or non-fatal radiographically or pathologically proven recurrent symptomatic intracerebral hemorrhage for up to 5 years
-
Secondary: Major vascular events, grouped as either occlusive or hemorrhagic events. The study analyzed multiple classifications for what was considered an occlusive or hemorrhagic event
- Major hemorrhagic events included recurrent symptomatic ICH, other forms of spontaneous or traumatic ICH, and symptomatic extracranial hemorrhage at any site requiring transfusion endoscopic intervention or surgery, or resulting in death within 30 days.
- Major occlusive events included ischemic stroke, myocardial infarction, mesenteric ischemia,peripheral arterial occlusion, DVT or PE, and carotid, coronary, or peripheral arterial revascularisation procedures.
Inclusion Criteria:
- ≥ 18 years of age
- ICH confirmed by imaging
- Taking anticoagulation or antiplatelet medications for the prevention of occlusive vascular disease at the time of the stroke
- Survived for 24 hours
Exclusion Criteria:
- Died within 24 hours following the onset of symptoms
- Those who continued taking antithrombotic medication following the stroke
- Preceding trauma
- Hemorrhagic transformation of an ischemic stroke
- Intracranial but not intracerebral hemorrhage
- Intracranial hemorrhage from a macrovascular cause such as cavernous malformation, venous thrombosis, or aneurysm
- Pregnant women, breastfeeding women, and those of childbearing age who were not taking contraceptives
Baseline Characteristics
- The patients were an average of 76 years of age, 68% were male, and 92% were white
- One half of patients were taking aspiring
- One quarter of patients were taking clopidogrel
- One fifth of patients were taking oral anticoagulation
- 62% had lobar ICH
- 88% had one or more previous occlusive vascular events (including ischemic heart disease, ischemic stroke, and TIA)
- Approximately three quarters of patients had a history of hypertension
- One quarter of patients had atrial fibrillation
Results:
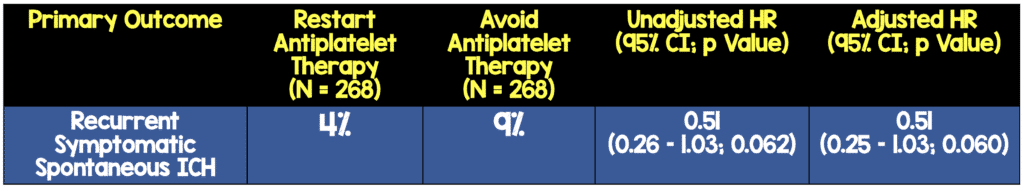
A lower rate of the primary outcome (recurrent symptomatic spontaneous intracerebral hemorrhage) was identified between groups; however, it did not reach pre-determined measures of statistical significance, and thus the null hypothesis could not be rejected. This non-significant reduction in the primary outcome was similar in unadjusted and adjusted models. There was no evidence of heterogeneity of the effects of antiplatelet therapy on the primary outcome in prespecified exploratory subgroup analyses.
Additionally, the rates of major occlusive events and major hemorrhagic events were not significantly different between the groups in any secondary analysis except for combined major vascular events using one of the classifications (non-fatal stroke, non-fatal myocardial infarction, or death from a vascular event) that did not include venous thrombotic events. However, there was no controlling for multiple comparisons.
Strengths:
- This is the first randomized trial on starting long-term antiplatelet therapy following an ICH.
- There was 100 percent follow-up by primary care physicians at all time points (6 months to 4 years). 79% done by mail, 16% by telephone, and 4% by both methods
- Adherence to treatment protocol started out high but decreased over time, from 99% at the time of discharge to 82% at 4 years.
- Staff following up patients and outcome event adjudicators were blinded to treatment allocation
- Used two internal assessor, consultant neurologists adjudicated every outcome event and were blinded to treatment allocation. This helps reduce misclassification of hemorrhagic and occlusive vascular events
- There was also one external assessor, consultant neurologist that randomly reviewed 25 of the outcome events. He/she agreed with the internal assessors for 24 (96%) of the outcome events
- Baseline characteristics of patients and use of antithrombotic agents was balanced between groups
- Blood pressure was controlled for both groups throughout follow up. Half of the patients had SBP below the recommended target of the UK national stroke guidelines
- Outcomes and methods were prespecified
Limitations:
- The study intended to recruit 720 participants, but only recruited 1-in-12 eligible patients. Instead, they extended the follow-up by 1 year in order to increase the number of person-years of follow-up and ICH numbers
- 26% of eligible patients were not recruited due to their physicians not agreeing to follow the protocol, which could have resulted in sampling bias.
- In this study, the participants were recruited at a median of 76 days following the ICH, with an IQR of 29-146. There is not enough data to analyze the effects of early intervention with antiplatelet medication.
- This study does not address other forms of intracranial hemorrhage including aneurysmal, traumatic, extra-axial, etc.
- As nearly all patients were treated with antiplatelet monotherapy, these data cannot be extrapolated to routine dual antiplatelet therapy regimens.
- Subgroup analyses of different antiplatelet medications, dosages, and timing are limited by study size.
- No placebo group (i.e. comparator was avoiding antiplatelet therapy)
- Antiplatelet regimens were mostly monotherapy, so the effects of dual antiplatelet therapy remain uncertain
- Adherence to the allocated treatment declined over time but was more than 80% even after 4 years of follow up
- Antiplatelet therapy helps prevent arterial thrombosis predeominantly. However venous thrombosis was included in the composite secondary outcome
Discussion:
- This trial will continue follow-up for 2 years, after which time the results will be published. Other similar trials are ongoing in Europe and will provide further information on this clinical question.
- 97% (522 pts) had ICH without an underlying structural or macrovascular cause identified)
- The risk of recurrent ICH in this study was at the lower end of ranges reported in other studies, but similar to the 0.61 – 1.20% annual rates observed with cilostazol or aspirin use in the PICASSO trial. [3]
- The risk of GIB was low in this study, possibly due to the prevalence of PPI use (4 pts or 1% in the antiplatelet group and 0 pts or 0% in the no antiplatelet group).
- There are currently two RCTs that are ongoing trying to answer the same clinical question:
- RESTART-Fr (NCT02966119, intended sample size of 280 patients)
- STATICH (NCT03186729, intended sample size of 250 patients)
Author’s Conclusions: “These results exclude all but a very modest increase in the risk of recurrent intracerebral haemorrhage with antiplatelet therapy for patients on antithrombotic therapy for the prevention of occlusive vascular disease when they developed intracerebral haemorrhage. The risk of recurrent intracerebral haemorrhage is probably too small to exceed the established benefits of antiplatelet therapy for secondary prevention.”
Clinical Take Home Point: The established benefits of antiplatelet therapy likely outweigh what may be a small or non-existent increased risk of recurrent bleeding following ICH; however, it is unclear when is the optimal time to restart therapy.
Guest Post By:

Cara M. Borelli, DO
UT Health Science Center at San Antonio
PGY-1 Resident
San Antonio, TX
References:
- RESTART Collaboration. Effects of Antiplatelet Therapy After Stroke due to Intracerebral Haemorrhage (RESTART): A Randomised, Open-Label Trial. Lancet 2019. PMID: 31128924
- Hemphill JC III et al. Guidelines for the Management of Spontaneous Intracerebral Hemorrhage. A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2015. PMID: 26022637
- Kim BJ et al. Prevention of Cardiovascular Events in Asian Patients With Ischaemic Stroke at High Risk of Cerebral Haemorrhage (PICASSO): A Multicentre, Randomised Controlled Trial. Lancet Neurol 2018. PMID: 29778364
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post RESTART: REstart or STop Antithrombotics Randomized Trial appeared first on REBEL EM - Emergency Medicine Blog.
