http://en.evtm.org/Combat-tested abdominal/junctional tourniquet proven equivalent to REBOA
https://www.trauma-news.com/2019/08/combat-tested-abdominal-junctional-tourniquet-proven-equivalent-to-reboa/
Combat-tested abdominal/junctional tourniquet proven equivalent to REBOA
BY TRAUMA NEWS ON AUGUST 16, 2019 SOLUTIONSRecent wartime experience has demonstrated that tourniquets can save lives. Yet many common military and civilian injuries — particularly armpit and groin injuries and pelvic fractures — remain difficult to treat in the field. Patients with these injuries are at high risk for bleeding to death.
This article was developed by Trauma System News in cooperation with our advertiser, Compression Works.
Since 2012, special operations forces worldwide have been using an advanced tourniquet device to treat these difficult bleeding injuries — the Abdominal Aortic and Junctional Tourniquet™ (AAJT). Independent research has shown that the AAJT effectively occludes blood flow to the pelvis and the extremities.
“The AAJT is the only junctional tourniquet that has saved lives endangered by junctional hemorrhage in both the upper and the lower extremities,” said John Croushorn, MD, emergency medicine physician and co-inventor of the device.
“Even more important, it is the only such device that can also be applied to the abdomen,” he said. “As a result, it gives first responders a tool that lets them leverage the ‘REBOA effect’ to save patient lives.”
Recently, the inventors of the abdominal/junctional tourniquet introduced the AAJT-S (the S stands for stabilized). The updated design is not only more secure but faster and easier to apply.
Designed for battle environment
Dr. Croushorn deployed to Iraq in 2004 as a flight surgeon with the Mississippi National Guard. He later worked with U.S. Special Operations units, where he developed a particular interest in bleeding control — specifically, massive bleeding below the waist.
At the time, one of the newer ideas for controlling lower-body bleeding was to compress the aorta by pressing a knee into the mid-abdomen. After Dr. Croushorn transferred back to the U.S., he supervised a group of resident researchers who validated this technique in a swine model. He and a colleague soon began developing a device to replicate the knee effect.
“We received FDA approval for our device in early 2012,” Dr. Croushorn said. “And by the end of that year, the original AAJT was in the hands of both American and British special forces.”
How to use the AAJT-S
AAJT abdominal placement
Abdominal placement, demonstrated with original device (click to enlarge)
Field application is simple. To apply the AAJT-S to the mid-abdomen:
Buckle the device around the waist by passing the plastic ladder strap under the patient
Insert the ladder strap into the ratcheting buckle until the red mark on the ladder strap meets the red guide on the buckle
Position the main unit over the target area
Pull belt tight, taking all the slack out of the system
Tighten the ratchet until the device is tight around the patient
Inflate the device’s wedge-shaped bladder until the pressure indicator shows green (250 mmHg)
“As the wedge inflates, it pushes into the patient, cutting off blood flow through the descending aorta at or near the bifurcation,” Dr. Croushorn said. “You keep inflating the device until it reaches 250 mmHg, which is indicated by a green zone on the pressure gauge. We teach users to go for the green.”
The entire process takes about a minute. The updated design’s strap-and-ratchet mechanism makes application faster than ever. In addition, all controls are now in the front of the device, allowing for greater ease of use under challenging emergency conditions.
When applied to the abdomen, the AAJT-S can safely remain in place for 60 minutes. The AAJT-S also has FDA 510(k) approval for treating junctional hemorrhage at the groin or axilla. When applied to a junction, the device can remain in place for up to 4 hours.
“The original AAJT was first used by the British in 2013 to treat an Afghan soldier who was injured by an IED,” Dr. Croushorn said. “He lost both legs and had serious pelvic injuries and was frankly dying, but they put the device on him and he survived.”
“REBOA effect” in one minute
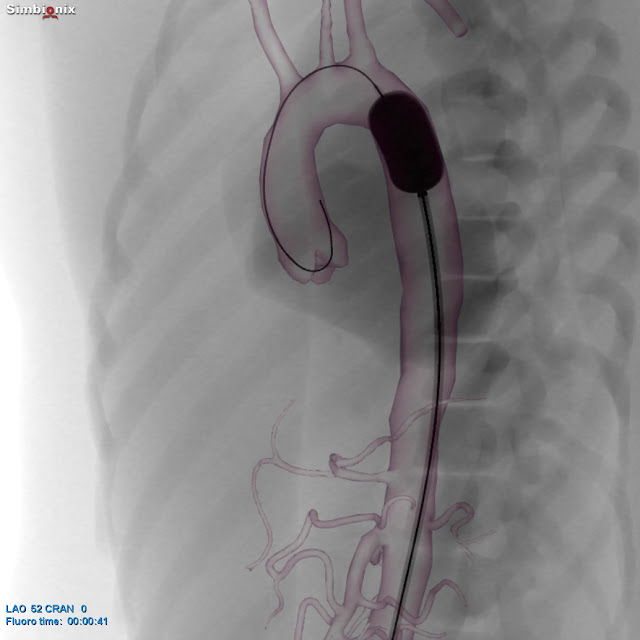
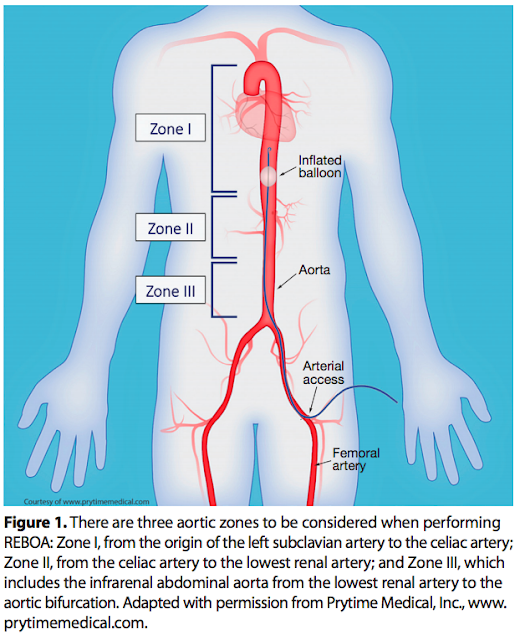
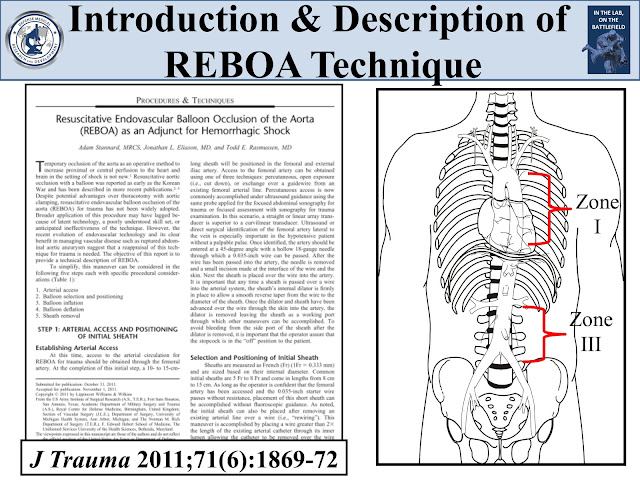
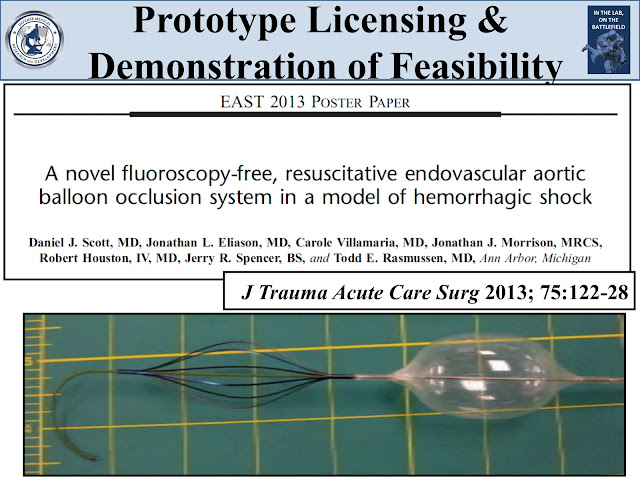
According to Dr. Croushorn, the AAJT-S mimics the effect of resuscitative endovascular balloon occlusion of the aorta (REBOA).
“REBOA stops massive bleeding and confines the blood volume to the heart, brain and kidneys, so it can be a life-saving intervention for severely bleeding patients,” he said. “Unfortunately, REBOA is limited right now to hospital use by a physician — and most patients who might benefit from it will bleed out before they even reach the hospital.”
AAJT axilla placement
Axilla placement, demonstrated with original device (click to enlarge)
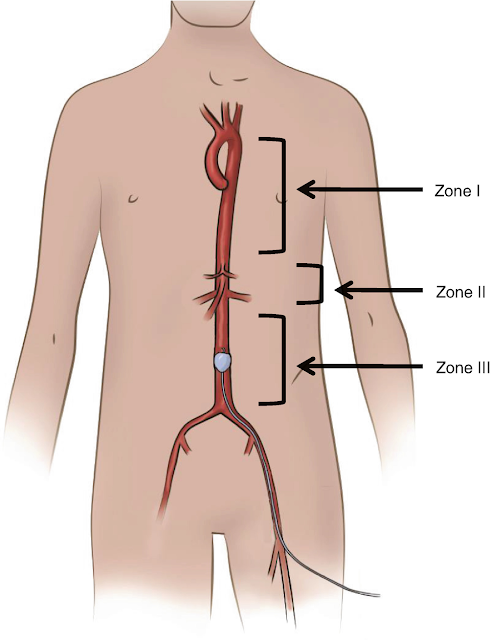
In August 2017 independent investigators from the U.S. Army Institute of Surgical Research and the Air Force’s 59th Medical Wing presented research showing that the abdominal/junctional tourniquet is equivalent to Zone 3 REBOA. (Journal of Surgical Research, Volume 226, June 2018)
“In addition, the Air Force group looked specifically at traumatic cardiac arrest,” Dr. Croushorn said. “They found that abdominal/junctional tourniquet application and blood transfusion led to 83% survival compared to 17% survival with blood and CPR alone.” (Military Medicine, Volume 182, September 2017)
“For years we taught medics that if a patient is in cardiac arrest from bleeding out, there is no reason to do CPR,” he said. “Now, with the AAJT-S, we can actually save most of these people, and that’s because of the REBOA effect of this device.”
Paramedics can use the AAJT-S to achieve the physiologic benefits of REBOA at the point of injury. The device can also be deployed in the ED as a “bridge therapy” while waiting for a trauma surgeon or emergency medicine physician to apply REBOA.
“The AAJT-S opens up the opportunity to achieve the benefits of REBOA much earlier,” Dr. Croushorn said. “We can’t put a trauma surgeon in every ambulance, but we can give medics the capability to do what trauma surgeons do.”
Effective intervention for pelvic fractures
While the AAJT-S was developed for a military setting, it could also help solve a major problem in civilian trauma — pelvic fracture bleeding.
The AAJT-S abdominal/junctional tourniquet
The redesigned AAJT-S abdominal/junctional tourniquet (click photo to enlarge)
“In the U.S., we have 115,000 pelvic fractures per year,” Dr. Croushorn said. “Paramedics are trained to recognize when the pelvis is broken, but they have no way to know whether a patient is bleeding from that fracture until their blood pressure starts to drop.”
In these situations, paramedics are little more than transport providers. “They can’t help these patients outside of applying a pelvic binder or simply tying a sheet around their hips,” he said. “That can reduce the bleeding volume but it does not stop the bleeding.”
For these patients, the AAJT-S is a potentially life-saving tool. Once a paramedic recognizes pelvic fracture, he or she can deploy the device at the mid-abdomen and quickly stop the blood flow to the pelvis.
“The AAJT-S lets you ‘turn off the faucet’ of pelvic bleeding,” Dr. Croushorn said. “It provides something that medics can do before they get to the hospital to prevent these patients from going into shock.”
Safety and ease of use
AAJT groin placement
Groin placement, demonstrated with original device (click to enlarge)
“Other junctional devices use point pressure, so they require very precise placement,” Dr. Croushorn said. “And, in fact, if the patient moves it is very easy to lose hemorrhage control.”
In contrast, the AAJT-S compresses a relatively large surface area. “Because of that, the user does not have to have specific knowledge of anatomy, so any first responder can place it,” he said. “That also means the device stays in place, even during hasty extractions.”
The recent design update includes a wider 3-inch belt that improves stability. In addition, the device is now built around a single platform of tough HDPE plastic, which distributes compression force more effectively.
Compared to other junctional devices, the wider compression area of the AAJT-S also lowers the risk of complications. “Other junctional hemorrhage tourniquets reach tissue pressures in the range of 700 to 800 mmHg, which increases the risk of tissue necrosis and nerve death,” Dr. Croushorn said.
The AAJT-S includes an automatic release valve that prevents the pressure from exceeding 300 mmHg. “It’s not much more pressure than you would experience with a blood pressure cuff in your doctor’s office,” Dr. Croushorn said.
(Read more: Complications of the Abdominal Aortic and Junctional Tourniquet: What the research says.)
A complement to Stop the Bleed
The Stop the Bleed campaign is spreading the use of conventional extremity tourniquets. However, these devices are ineffective in several challenging hemorrhage scenarios.
“That’s why I think the Abdominal Aortic and Junctional Tourniquet has an important role to play in this initiative,” Dr. Croushorn said. “The AAJT-S can provide early hemorrhage control for a high-risk subset of bleeding patients — individuals with dangerous bleeding at junctional sites and the pelvis.”
For more information on the AAJT-S, visit CompressionWorks.com. To order the AAJT-S for delivery in the United States, visit the Compression Works store page or North American Rescue. To order for delivery in Europe, visit exclusive EU distributor Fenton Pharmaceuticals. The AAJT-S will also be available from GSA Advantage this fall.
See it at the Military Health Symposium. The AAJT-S will be highlighted at the 2019 Military Health System Research Symposium taking place August 19-22 in Kissimmee, Florida. To see and use the device, visit North American Rescue at Booth #601.