
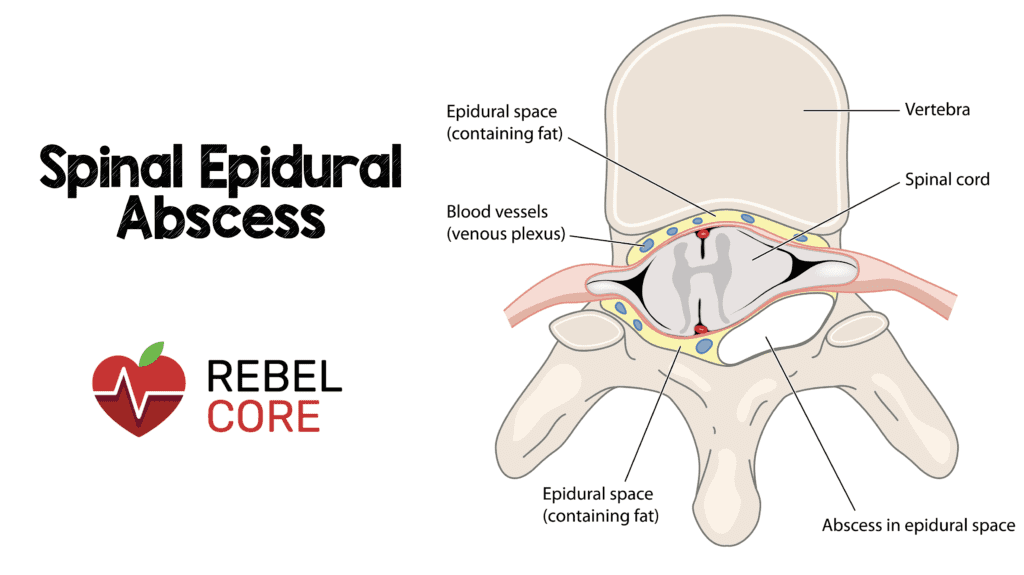
 Definition: Suppurative infection enclosed within the epidural space
Definition: Suppurative infection enclosed within the epidural space
Epidemiology
-
Incidence: 2-3 cases per 10,000 hospitalized patients (Sendi 2008).
- Rate is increasing given the rise in number of spinal procedures and anesthesia techniques
- Mortality is low at 5%, however, if untreated paralysis may occur
- Can occur at any age but most patients are between 50 and 70 years old.

Pathogenesis
-
Classified as either primary or secondary:
-
Primary: Hematogenous spread from a distant focus to the epidural space
- Usually from skin and soft tissue infections
- Often located in the posterior/dorsal aspect of the spinal canal due to the presence of infection prone adipose tissue.
-
Secondary: Direct inoculation from recent spinal procedure, trauma or contiguous spread from adjacent discitis or osteomyelitis
- Typically develops in the anterior/ventral epidural space
-
Primary: Hematogenous spread from a distant focus to the epidural space
- Organism: Most commonly Staph Aureus (MSSA and MRSA) with Coagulase-negative Staph and gram negative bacilli as the second and third most common, respectively
- Enlarging abscess may lead to spinal cord compromise via direct compression or interruption of blood supply
History and Physical
-
Risk Factors – The presence of certain comorbidities places patients at increased risk for developing disease. However, 20% of patients with SEA will have no predisposing factors. Risk factors include:
- Immunocompromised: DM, HIV, Malignancy, chronic steroids or immunosuppressant medication use
- Recent Soft Tissue Infection with Bacteremia (OR = 13.5) (Davis 2020)
- Spinal Abnormality: trauma, surgery, arthritis
- Substance Abuse: Alcoholism, IVDU
- Presence of an indwelling catheter
- Elderly
-
Spinal epidural abscess is known for its nonspecific presentation, and can be easily missed. Adding it to the differential is often the critical step in making the diagnosis.
-
Classic triad of fever, back pain and neurologic symptoms is only present in 15% of patients. (Darouiche 2006)
-
Back pain is the most common symptom (75% patients).
- Described as localized, severe and midline with tenderness to percussion.
- Fever is an inconsistent finding (50% of patients). Normothermia should not deter further workup.
- Neurologic symptoms (33% of patients) may indicate spinal cord compromise. These patients require rapid work-up and management. Once paralysis develops, it is often irreversible.
-
Back pain is the most common symptom (75% patients).
-
Classic triad of fever, back pain and neurologic symptoms is only present in 15% of patients. (Darouiche 2006)
-
4 Stages of Progression (Heusner 1948) – stepwise symptomatology of spinal epidural abscesses
- Pain: back pain at the spinal level affe3cted (however, lesions may be distant to location of pain)
- Radiculopathy: nerve root pain radiating from involved spinal region
- Weakness: motor weakness, sensory deficit, bladder and bowel dysfunction (retention or incontinence)
- Paralysis
-
Skip lesions – lesions present in noncontiguous vertebrae.
-
Increased risk if patient has 2 or 3 of the following symptoms (Ju 2015):
- Delay in presentation (symptoms for ≥7 days)
- Concomitant area of infection outside the spine and paraspinal region
- ESR >95 mm/h at presentation.
- If a patient displays symptoms not localized to a certain spinal level, consider imaging the entire spine.
-
Increased risk if patient has 2 or 3 of the following symptoms (Ju 2015):

Diagnosis
-
Labs – routine labs are unhelpful in diagnosis but are drawn to assist inpatient management
- CBC: Leukocytosis is present in 66% of cases (Davis 2004), however a normal WBC count is insufficient to rule out SEA.
-
ESR/CRP: sensitive, however very nonspecific.
- ESR normal values vary by age, and are frequently elevated in patients with neoplastic disease, regardless of the presence of infection.
- CRP normalizes quicker than ESR, and may be used in post-op patients or trended as an indicator of treatment success.
- Recently, a treatment guideline suggested incorporating ESR/CRP elevation in the decision to pursue imaging (Davis 2011). It is important to note that this treatment guideline was based on a small set (n =86) of patients. Currently, neither the presence nor the degree of elevation should be used to rule-in or rule-out SEA
-
Blood Cultures
- Provides assistance in tailoring antibiotic therapy
- Isolates have excellent correlation with the organism later found during surgical drainage
-
Imaging
-
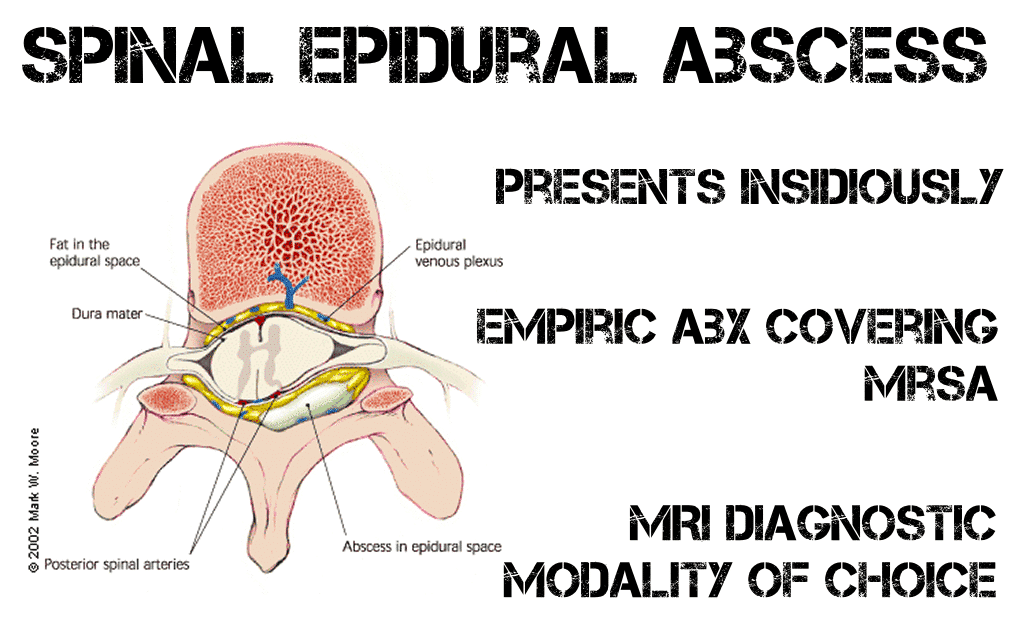
Gadolinium enhanced MRI: gold standard for diagnosis, over 90% sensitive (Darouiche 2006). MRI is able to detect an abscess in early disease, show the extent of inflammatory changes and identify thecal sac compression.
- (Image 2)
-
CT with IV contrast – indicated only when MRI is contraindicated
- Cannot readily distinguish early findings of infection from typical soft tissue, disk and osseous changes
-
Gadolinium enhanced MRI: gold standard for diagnosis, over 90% sensitive (Darouiche 2006). MRI is able to detect an abscess in early disease, show the extent of inflammatory changes and identify thecal sac compression.
Management
-
Empiric Antibiotics: directed against Staphylococcus and Gram Negative Bacilli.
- Vancomycin (30-60 mg/kg divided into two daily doses) PLUS
- 3rd Generation Cephalosporin: Cefotaxime (2 g IV every 6 hrs), Ceftriaxone (2 g IV every 12 hours) or Ceftazidime (2 g IV every 8 hours)
-
Operative drainage: Not all epidural abscesses are surgically drained. Decision is determined by:
-
Neurologic deficits
- Those with developing neurologic deficits are often drained given risk of rapid development to paralysis.
- Patients whom have already progressed to paralysis with low likelihood of improvement are often treated with antibiotics alone.
-
Presence of a drainable abscess versus a phlegmon on imaging
- A phlegmon is granulomatous-thickened tissue without a significant purlent collection. It is noted as a homogenously enhancing lesion on MRI.
- A liquid abscess is displayed as a central hypointense region with hyperintense peripheral enhancement.
- Location – given small amount of epidural space, and thus increased risk of developing neurologic sequelae, cervical or thoracic epidural abscesses are more likely to be surgically drained
-
Neurologic deficits
Take Home Points
- Spinal Epidural Abscess may present insidiously and patients often lack the classic triad of fever, back pain and neurologic symptoms
- Empiric Antibiotics should cover Staphylococcus (including MRSA) and Gram negative Bacilli
- All patients with clinical suspicion require rapid evaluation with MRI as the diagnostic study of choice
- Although not all patients will go to the operating room, surgical consult (Neurosurgery or Orthopedics) should be obtained immediately
Guest Post By: Latrice Triplett, MD
References
- Boody B, et al. Vertebral Osteomyelitis and Spinal Epidural Abscess: An Evidence-based Review. J Spinal Disord Tech. 2015 Jul;28(6):E316-27 PMID: 26079841
- Darouiche RO. Spinal epidural abscess. N Engl J Med. 2006; 355; 2012-2020 PMID: 17093252
- Davis DP, et al. The Clinical Presentation and Impact of Diagnostic Delays on Emergency Department Patients with Spinal Epidural Abscess. J Emerg Med. 2004 Apr;26(3):285-91. PMID: 15028325
- Davis DP, et al. Prospective Evaluation of a Clinical Decision Guideline to Diagnose Spinal Epidural Abscess in Patients who Present to the Emergency Department with Spine Pain. J Neurosurg Spine. 2011 Jun;14(6):765-70. PMID: 21417700
- Davis WT et al. High Risk Clinical Characteristics for Pyogenic Spinal Infection in Acute Neck or Back Pain: Prospective Cohort Study. AJEM 2020. PMID: 31128933
- Della-Guistina, D. Evaluation and Treatment of Acute Back Pain in the Emergency Department. Orthopedic Emergencies 2015 May; 33(2) 311-26. PMID: 25892724
- Heusner A, Nontuberculosis Spinal Epidural Infections. N Engl J Med. 1948 Dec; 239(23) 845-54. PMID: 18894306
- Ju K, et al. Predicting patients with concurrent noncontiguous spinal epidural abscess lesions. Spine J. 2015 Jan 1; 15(10):95-101. PMID: 24953159
- Sendi P, et al. Spinal epidural abscess in clinical practice. QM. 2008 Jan; 101(1)1-12. PMID: 17982180
- Winters ME, Kluetz P et al. Back Pain Emergencies. Med Clin North Am, 2006 May;90(3):505-23. PMID: 16473102
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post Spinal Epidural Abscess (SEA) appeared first on REBEL EM - Emergency Medicine Blog.
