
 Background: Hypoxemia and hypoperfusion are important factors in outcomes after ROSC. While hypoxemia (SpO2 <90%) is clearly deleterious, it is unclear if hyperoxia is beneficial. Recent studies on patients requiring critical care have demonstrated that hyperoxia is harmful and instead we should be targeting normoxia (SpO2>93%). Similarly, while it is clear hypotension/hypoperfusion will result in worse outcomes, it is unknown whether we should be targeting higher blood pressures after ROSC. A higher MAP may offer advantages due to improved cerebral perfusion pressure, however data is lacking.
Background: Hypoxemia and hypoperfusion are important factors in outcomes after ROSC. While hypoxemia (SpO2 <90%) is clearly deleterious, it is unclear if hyperoxia is beneficial. Recent studies on patients requiring critical care have demonstrated that hyperoxia is harmful and instead we should be targeting normoxia (SpO2>93%). Similarly, while it is clear hypotension/hypoperfusion will result in worse outcomes, it is unknown whether we should be targeting higher blood pressures after ROSC. A higher MAP may offer advantages due to improved cerebral perfusion pressure, however data is lacking.
Paper 1: Schmidt HJ et al. Oxygen Targets in Comatose Survivors of Cardiac Arrest. NEJM 2022. PMID: 360027567[Access on Read by QxMD]
Paper 2: Kjaergaard J et al. Blood-Pressure Targets in Comatose Survivors of Cardiac Arrest. NEJM 2022. PMID: 36027564 [Access on Read by QxMD]
Clinical Question 1: What is the appropriate oxygen target for mechanical ventilation in comatose survivors of out-of-hospital cardiac arrest?
Clinical Question 2: What is the appropriate blood pressure target in comatose survivors of out-of-hospital cardiac arrest?
What They Did:
- Blood Pressure and Oxygenation Targets in Postresuscitation Care (BOX) Trial
-
Oxygen Target Phase of Trial (Paper 1)
- Investigator-initiated, open-label, randomized, superiority, 2×2 factorial design, clinical trial
- Trial took place in Denmark
- Comatose adults with OHCA randomized to:
- Restrictive O2: PaO2 9 to 10 kPa (68 to 75mmHg)
- Initial FiO2 set at 0.3
- Liberal O2 (PaO2 13 to 14kPa (98 to 105mmHg)
- Initial FiO2 set at 0.6
- FiO2 adjusted to assigned target but increased if peripheral ABG fell below 93% on pulse oximetry
- Restrictive O2: PaO2 9 to 10 kPa (68 to 75mmHg)
-
BP Target Phase of Trial (Paper 2)
- Investigator-initiated, double-blind, randomized, superiority, 2×2 factorial design, clinical trial
- Trial took place in Denmark
- Comatose adults with OHCA randomized to:
- Lower MAP: 63mmHg
- Higher MAP: 77mmHg
- All patients underwent temperature control at 36C with sedation and mechanical ventilation for at least 24hrs
- After maintenance period at 36C, core temperature was gradually raised to normothermia, and sedation weaned
Outcomes:
-
Primary: Composite of death from any cause or hospital discharge with severe disability or coma (CPC 3 or 4) within 90d after randomization (whichever occurred 1st)
- Truly not a composite outcome, but rather a good neurologic outcome vs poor neurologic outcome
-
Secondary:
- Neuron-specific enolase levels at 48hrs
- Death from any cause
- Montreal Cognitive Assessment Score (Range 0 to 30; Higher scores indicate better cognitive ability)
- Modified Rankin Scale score (Range 0 to 6; higher scores indicating greater disability)
- CPC at 90d
Inclusion:
- Adult (Age ≥18 years) patients
- Admitted to the hospital
- After resuscitated cardiac arrest (of presumed cardiac cause)
- Unconscious (GCS ≤8)
- Sustained return of spontaneous circulation (20 minutes of circulation)
- Targeted temperature management indicated
Exclusion:
- Conscious patients
- Pregnancy
- OHCA presumed non-cardiac cause
- Cardiac arrest after arrival in hospital
- Known bleeding diathesis
- Suspected or confirmed acute ICH suspected
- Confirmed acute stroke
- Temperature on admission <30C
- Unwitnessed asystole
- Persistent cardiogenic shock
- Known limitations in therapy
- Known disease making 180d survival unlikely
- Known pre-arrest CPC 3 or 4
- >240min from ROSC to randomization
BOX Trial O2 Results:
- 802 patients enrolled in the trial
- 789 patients underwent randomization
- Median time form cardiac arrest to randomization was 146 min (Range 113 to 187min)
- Shockable rhythm: 85%
- Witnessed arrest: 85%
- Bystander CPR: 87%
- Time until ROSC: 21min
- Immediate coronary angiography: 91%
- PCI: 42%
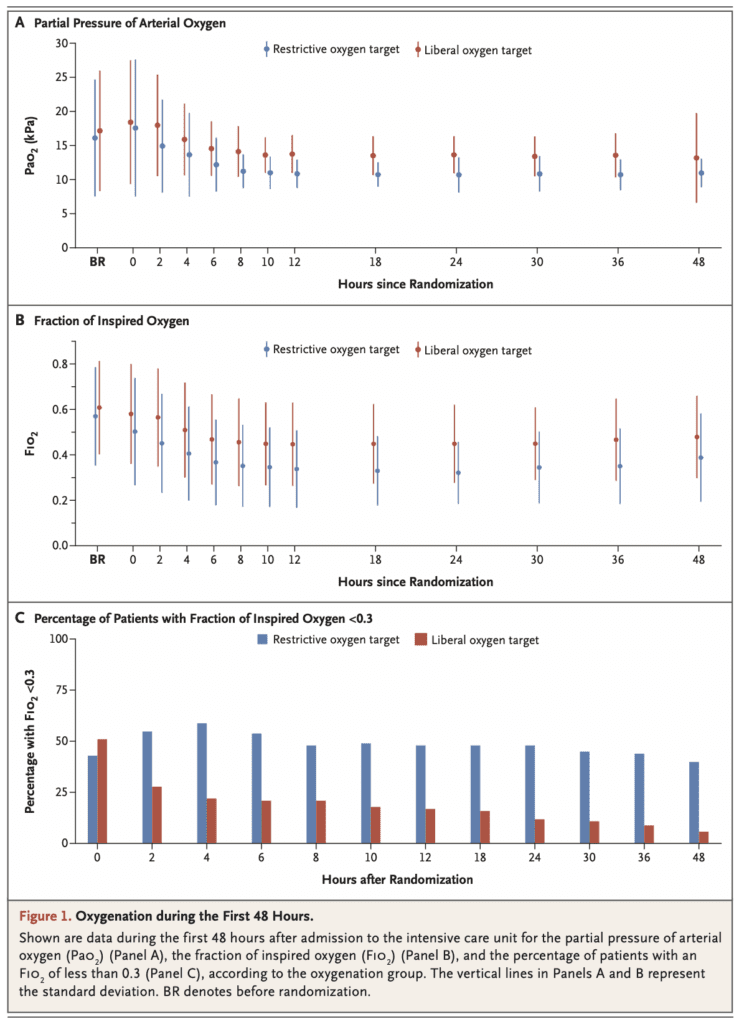
- Oxygen Intervention:
- On arrival to ICU patients in the two groups had similar values of PaO2 and FiO2 (See Figure Below)
- Separation of O2 levels between the two groups was established within 2 to 4 hours and remained through the first 48hrs (See Figure Below)
- Median duration of mechanical ventilation
- Restrictive O2: 57 hrs (Range 39 to 110)
- Liberal O2: 61 hrs (Range 40 to 111)
-
Composite outcome of death or hospital discharge with severe disability or coma within 90d (Primary Outcome):
- Restrictive O2: 32.0%
- Liberal O2: 33.9%
- HR 0.95; 95% CI 0.75 to 1.21; p = 0.69
- Results were consistent in all prespecified subgroups
- Death at 90d
- Restrictive O2: 28.7%
- Liberal O2: 31.1%
- HR 0.93; 95% CI 0.72 to 1.20
- Median CPC was 1 in both groups
- Median mRS score was 2 in the restrictive group and 1 in the liberal group
- Median Montreal Cognitive Assessment score was 27 in both groups
- Median neuron-specific enolase level at 48hrs was 17ug/L in the restrictive group and 18ug/L in the liberal group
- Incidence of adverse events was similar in the two groups
BOX Trial BP Results:
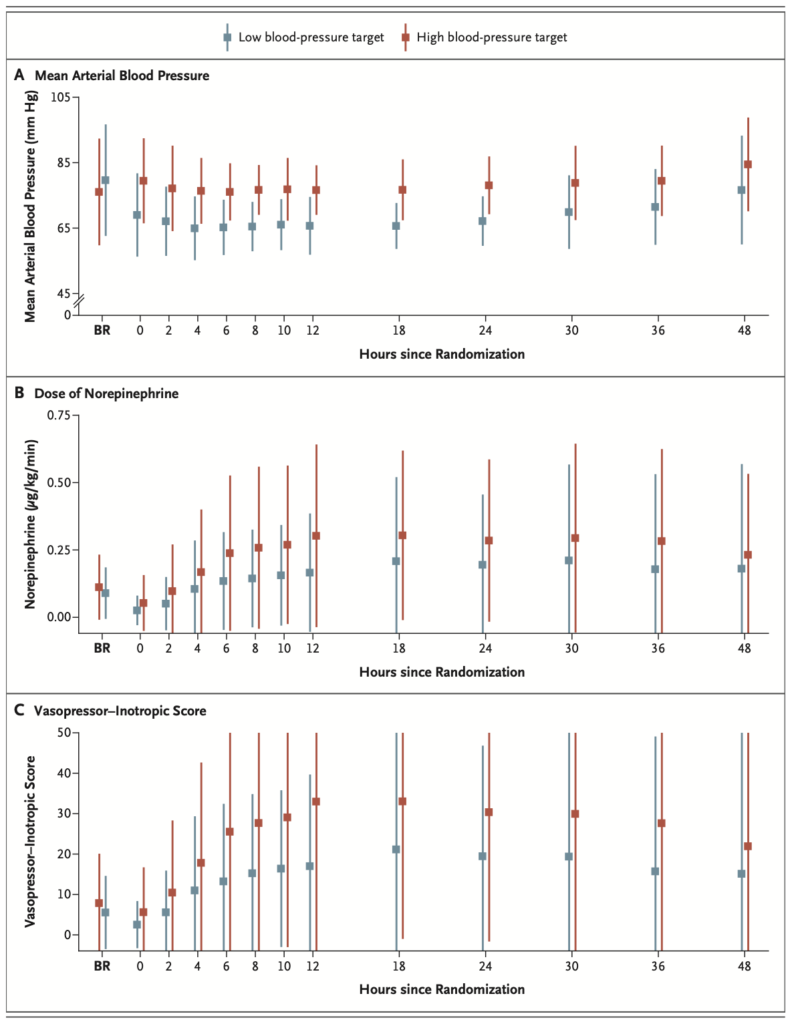
- Blood Pressure Intervention
- Separation of blood pressure values was achieved with a mean difference of 10.7mmhg (95% CI 10.0 to 11.4)
- The norepinephrine dose and vasopressor-inotropic score was higher in the high-target group
-
Composite outcome of death or hospital discharge with severe disability or coma within 90d (Primary Outcome):
- Lower MAP: 32.0%
- Higher MAP: 34.0%
- HR 1.08; 95% CI 0.84 to 1.37; p = 0.56
- Results were consistent in the prespecified subgroups (including those with HTN)
- Death at 90d:
- Lower MAP: 29%
- Higher MAP: 31%
- HR 1.13; 95% CI 0.88 to 1.46
- Median CPC was 1 in both groups
- Median mRS was 1 in both groups
- Median Montreal Cognitive Assessment scores were 27 (Higher MAP) and 26 (Lower MAP)
- Median neuron-specific enolase level at 48 hours was similar between groups
- The percentage of patients with adverse events did not differ significantly between groups
Strengths Common to Both Trials:
- These studies ask a clinically meaningful set of questions with little current evidence to guide practice
- Performed prespecified subgroup analyses of the primary outcome to see if there was any subgroup where benefit or harm should be hypothesized
- No imputations for missing data were performed, meaning the results we get are believable and real
- Used an intention-to-treat analysis which mimics real life practice as opposed to per-protocol analysis which follows exactly what was studied
- Baseline characteristics between groups were well balanced in terms of medical history, OHCA features, and findings/procedures at hospital arrival and therefore not biasing the results to favor one intervention over the other
- Authors achieved separation between groups in the PaO2 achieved by 2 hours after randomization
Limitations Common to Both Trials:
- Due to pandemic restrictions the Montreal Cognitive Assessment score was done via telephone interview or review of hospital charts limiting the performance of this score
- Unclear if there was sequential enrollment of patients, which could introduce a selection bias
- Only enrolled patients with suspected cardiac cause of cardiac arrest. Therefore, results do not apply to patients with other etiologies of cardiac arrest
- Some patients had spontaneous PaO2 levels that exceeded the restrictive oxygenation target, even without additional O2 supplementation during mechanical ventilation. This could bias the results to show no difference between groups
- Separation between groups did not occur until 2 hours after randomization. It is unclear whether more aggressive attention to prehospital interventions would have changed results of the trial
- O2 portion of the trial was open-label which could bias choices regarding continued life-sustaining therapies which could affect outcomes
Discussion:
- Authors were looking for a 10% difference in the primary composite outcome. They would need 732 patients to provide an 80% power, or 846 patients would provide a 90% power. The assumption was a mortality of 28% (This was assumed based on department 6month mortality of 33%)
- The authors did achieve a separation between groups regarding the PaO2 values, but this separation did not start until 2 hours after ICU admission. Despite achieving separation and maintaining it for 48hrs there was no significant between group difference in the primary outcome
- The authors also did achieve a separation between groups regarding the mean arterial pressure values, with a separation of 10.7mmHg. This is however lower than what they were trying to achieve (14mmHg). In addition, there was an observed difference between the groups regarding doses of norepinephrine and vasopressor
- An interesting point about these two papers was the BP portion of the trial was double-blinded whereas the O2 portion of the trial was open-label (unblinded).
Author Conclusion for Paper1: “Targeting of a restrictive or liberal oxygenation strategy in comatose patients after resuscitation for cardiac arrest resulted in similar incidence of death or severe disability or coma.”
Author Conclusion for Paper2: “Targeting a mean arterial blood pressure of 77mmHg or 63mmHg in patients who had been resuscitated from cardiac arrest did not result in significantly different percentages of patients dying or having severe disability or coma.”
Clinical Take Home Point: In comatose adult patients, with presumed cardiac etiology of their cardiac arrest, with ROSC…
- There appears to be no difference between a restrictive vs liberal oxygenation target regarding the incidence of death or severe disability or coma at 90 days.
- I will continue to titrate FiO2 to maintain a PaO2 range of 68 to 105mmHg (based on this trial) or an SpO2 of 90 to 95% (my bedside practice) in the post arrest setting.
- There appears to be no difference between targeting a lower mean arterial pressure (63mmHg) vs a higher mean arterial pressure (77mmHg) regarding the incidence of death or severe disability or coma at 90 days.
- I will continue to target a mean arterial pressure of ≥65mmHg in the post arrest setting.
References:
- Schmidt HJ et al. Oxygen Targets in Comatose Survivors of Cardiac Arrest. NEJM 2022. PMID: 360027567[Access on Read by QxMD]
- Kjaergaard J et al. Blood-Pressure Targets in Comatose Survivors of Cardiac Arrest. NEJM 2022. PMID: 36027564 [Access on Read by QxMD]
For More Thoughts on This Topic Checkout:
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)
The post The BOX Trial: BP & O2 Targets in Comatose Survivors of Cardiac Arrest appeared first on REBEL EM - Emergency Medicine Blog.
