 Background: Rapid sequence intubation (RSI) is the most widely utilized approach for patients requiring emergency tracheal intubation. RSI typically requires the use of a induction agent followed by the use of a neuromuscular blocking agent (NMBA) to improve the overall intubation conditions and therefore improve first-attempt intubation success rate. Historically, succinylcholine has been the preferred NMBA, due to its fast onset (45 – 60 seconds) and fast offset (6 – 8 minutes of paralysis). Recent studies, however, show that rocuronium is an effective agent (similar timing of onset for ideal intubating conditions) as well. When used at a dose of 1.2mg/kg, rocuronium has a similar onset time to succinylcholine of about 1 minute. Additionally, succinylcholine has several contraindications (see bottom of the post) while rocuronium has no contraindications (except for hypersensitivity) which has increased the debate about the paralytic agent of choice for RSI.
Background: Rapid sequence intubation (RSI) is the most widely utilized approach for patients requiring emergency tracheal intubation. RSI typically requires the use of a induction agent followed by the use of a neuromuscular blocking agent (NMBA) to improve the overall intubation conditions and therefore improve first-attempt intubation success rate. Historically, succinylcholine has been the preferred NMBA, due to its fast onset (45 – 60 seconds) and fast offset (6 – 8 minutes of paralysis). Recent studies, however, show that rocuronium is an effective agent (similar timing of onset for ideal intubating conditions) as well. When used at a dose of 1.2mg/kg, rocuronium has a similar onset time to succinylcholine of about 1 minute. Additionally, succinylcholine has several contraindications (see bottom of the post) while rocuronium has no contraindications (except for hypersensitivity) which has increased the debate about the paralytic agent of choice for RSI.
What They Did:
- The Succinylcholine vs Rocuronium for Out-of-Hospital Emergency Intubation (CURASMUR) trial
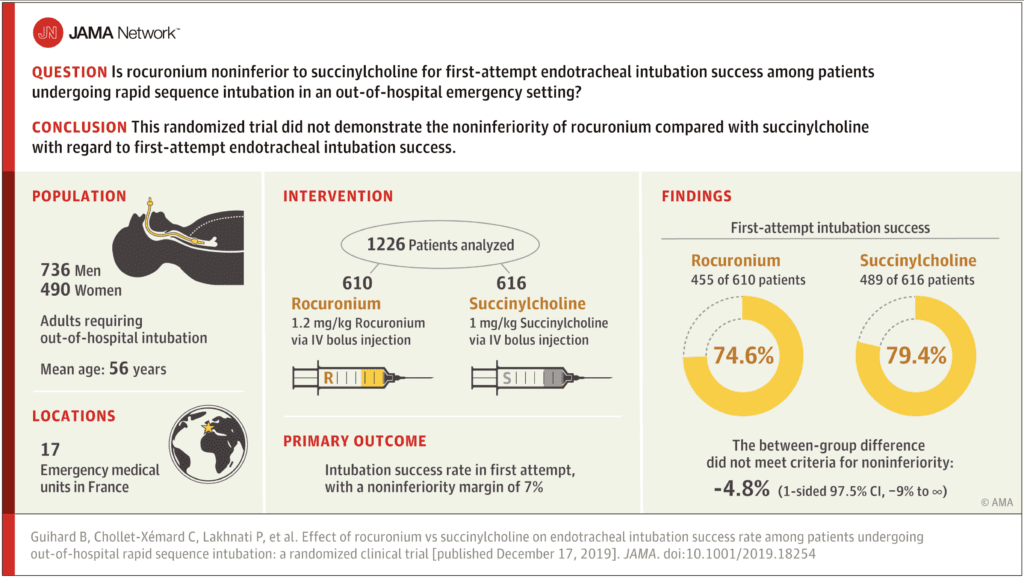
- Assess the non-inferiority of rocuronium to succinylcholine for tracheal intubation in the out-of-hospital setting
- Multicenter, single-blind, noninferiority randomized clinical trial comparing Rocuronium 1.2mg/kg IV vs Succinylcholine 1mg/kg IV for RSI
- 17 French out-of-hospital emergency medical units
Study Interventions:
- Sedation induction performed after preoxygenation
- Two induction agents recommended:
- Etomidate 0.3mg/kg IV
- Ketamine 2mg/kg IV
- Immediately followed by NMBA
- Succinylcholine 1mg/kg IV
- Rocuronium 1.2mg/kg IV
- Single-use Macintosh metallic laryngoscope blades (size 3 and 4) were used
- Interestingly standard intubation procedure did not include use of a stylet (considered an alternative airway procedure)
- Although standard interventions for this study, the following are not standard intubating practice in the US or Canada:
- Used Sellick’s maneuver as a standard
- Intubations done by physicians in the field
- If patient was a Can’t Intubate, Can’t Oxygenate (CICO) rocuronium was reversed with suggamedex
Outcomes:
- Primary: Intubation success rate on first attempt (Noninferiority margin of 7% was chosen)
-
Secondary:
- Cormack-Lehane grade of glottis visibility obtained by direct laryngoscopy (DL)
- Range 1 – 4; 1 indicates full view of glottis and 4 neither glottis nor epiglottis seen
- Overall difficulty of the intubation process
- Measured by the Intubation Difficulty Scale score – range of 0 to infinite; score > 5 indicates difficult intubation
- Intubation conditions, assessed by the Copenhagen score
- Poor, good, or excellent conditions)
- Percentage of patients intubated by alternative techniques
- Stylet, gum elastic bougie, ILMA, or cricothyrotomy)
- Intubation related complications in the first 15 minutes after intubation
- Cardiac arrest
- Hypotension = <90mmHg
- Hypoxemia = O2 sat <90%
- Physician-reported aspiration
- Severe arrhythmia = VT, VF, or allergic reaction
- Cormack-Lehane grade of glottis visibility obtained by direct laryngoscopy (DL)
Inclusion:
- Adult patients ≥18 years of age
- Requiring emergency tracheal intubation in the out-of-hospital setting
- Patients with all conditions (trauma, dyspnea, coma, overdoses, and shock)
Exclusion:
- Cardiac arrest
- Age <18 years
- Pregnancy
- Contraindication to rocuronium (i.e. known allergy)
- Contraindication to succinylcholine (i.e. personal or family history of known malignant hyperthermia, known allergy, congenital muscular dystrophy, myasthenia, specific hyperkalemia, recent open eye surgery, known congenital deficit in plasma pseudocholinesterases)
- Contraindication to sugammadex (selective paralytic binding agent for rocuronium reversal)
- Under guardianship
- No health insurance
Results:
- 1248 adult patients needing out-of-hospital tracheal intubation
- Majority of intubations were for coma due to neurological disease (≈50%) and coma due to self-poisoning (≈20%)
- Majority of intubations were done lying on a stretcher (≈50%) and lying on the ground (≈30%)
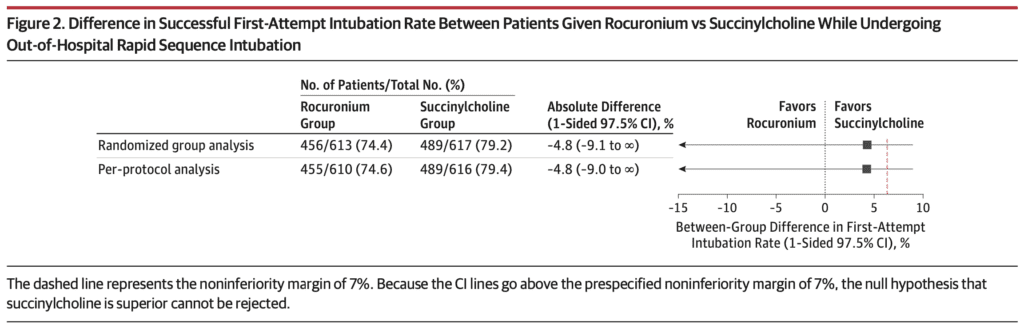
- 1st Pass Intubation Success Rate:
- Rocuronium: 455/610 (74.6%)
- Succinylcholine: 489/616 (79.4%)
- Between group difference of -4.8%
- 1-sided 97.5% CI = -9% to infinity
- Did not meet criteria for noninferiority
- No statistically significant between group difference for the Intubation Difficulty Scale score or the Copenhagen score
- No significant difference between the 2 groups in the use of alternative intubation techniques
- Intubation Related Complications Reported Within 15 Min After Intubation:
-
Overall
- Rocuronium: 111/610 (18.2%)
- Succinylcholine: 143/616 (23.2%)
- Hypoxemia:
- Rocuronium: 55/610 (9.0%)
- Succinylcholine: 61/616 (9.9%)
- Hypotension:
- Rocuronium: 39/610 (6.4%)
- Succinylcholine: 62/616 (10.1%)
-
Overall
Strengths:
- 1230/1248 patients (98.6%) completed the trial and 1226/1248 (98.2%) were included in the per-protocol analysis
- 1st randomized study comparing paralytic agents in emergency settings
- Consecutive out-of-hospital adult patients
- Limited exclusion criteria making the results of this study more generalizable
- Emergency situations: Not in the OR, not after fasting, and not after full evaluation therefore more like ED setting
Limitations:
- Study patients were blinded to intervention assignment, but the physicians conducting the intubation procedures were not blinded which could lead to bias
- Intubation protocols used in this study are much different than standard practices in many places in North America (No stylet, Use of Sellick’s maneuver, reversal of rocuronium in CICO, etc…)
- Patients were intubated without the use of a stylet or video laryngoscope which limits the generalization of the results to other out-of-hospital systems where these practices are widespread
- Successful first attempt orotracheal intubation assessed by the physician and confirmed by a capnography curve consistent over 3 respiratory cycles. This means results were physician self-reported without corroboration
- 1st pass success was not clearly defined (i.e. what counts as an attempt?)
- 1st pass success should not vary based on paralytic agent used unless patients were not paralyzed completely upon attempt.
- A more relevant primary endpoint would have been complications between agents
- Time between injection of paralytic agent and first tracheal intubation attempt were not recorded
- Pre-hospital setting is not the same environment, man/woman power, or number of potential adjuncts as seen in the ED setting
- Baseline differences between patients favored the succinylcholine group (i.e. rocuronium group was a sicker cohort)
- First pass success rate was significantly lower than ED 1st pass success rate making the results less generalizable to an ED setting
- Dosing of succinylcholine was on the lower side of what should be used in critically ill patients (i.e. Why not 1.5mg/kg IV?)
- Results are from a specific physican-staffed out-of-hospital emergency medical system and may not extrapolate to paramedical-based care systems
- Only early intubation-related complications during the out-of-hospital period were collected, and later hospital complications were not evaluated
- Sample size calculation was carried out from a hypothesis of a first-attempt intubation success rate of 75% with succinylcholine, but in this study was closer to 80%
- The noninferiority margin of 7% was selected based in part by expert opinion due to the paucity of high-level studies in this area
Discussion:
- Sample size calculation was based on successful 1st-attempt orotracheal intubation of 75% for patients. This is lower than what we traditionally see in ED studies.
- Agents used during the post-intubation period:
- Versed was the most common hypnotic used in ≈85% of patients, but the dose was higher in the succinylcholine group (median dose = 8mg vs 5mg).
- Sufentanyl was the most common analgesic used in ≈80% of patients, but again the dose was higher in the succinylcholine group (median dose = 20ug vs 15ug)
- The total doses of opioids and midazolam administered were greater in the succinylcholine group, which might have contributed to the higher frequency of hemodynamic complications in that group
- Although many of the complications were higher in the succinylcholine group, this was a post hoc exploratory outcome that requires more research
- One other point is that adverse events with succinylcholine were relatively rare in this study which means a study of this size won’t see many if any complications and therefore, succinylcholine could look potentially fine to us (Complications being low with succinylcholine may also be the case in real world practice, but something to keep in mind when evaluating this study)
- Biggest issue with this study is that the choice of paralytic shouldn’t influence the first pass success rate of intubation unless the dose is incorrect (i.e. to low) or the intubation attempt occurred too early
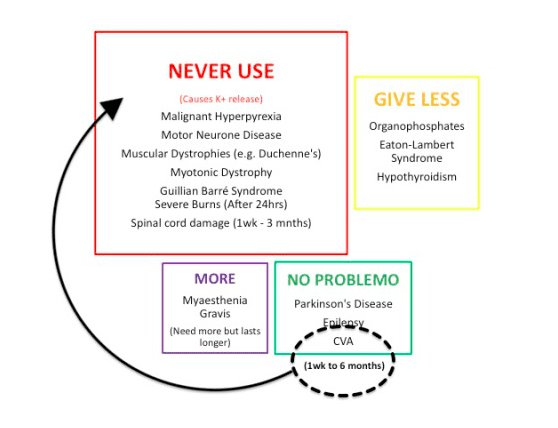
Contraindications for the use of Succinylcholine (From Sydney HEMS):
Author Conclusion: “Among patients undergoing endotracheal intubation in an out-of-hospital emergency setting, rocuronium, compared with succinylcholine, failed to demonstrate noninferiority with regard to first-attempt intubation success rate.”
Clinical Take Home Point: I am not sure why this is still a debate. If dosed appropriately, and the patient is paralyzed, the agent used should have no effect on the success rate of intubation. There are, however, several untoward effects of succinylcholine (i.e. hyperkalemia, shorter safe apnea time, etc) that push me toward using rocuronium.
References:
- Guihard Bertrand et al. Effect of Rocuronium vs Succinylcholine on Endotracheal Intubation Success Rate Among Patients Undergoing Out-of-Hospital Rapid Sequence Intubation: A Randomized Clinical Trial. JAMA 2019. [Epub Ahead of Print]
For More Thoughts on This Topic Checkout:
- PulmCrit: Rare Catastrophic Complications, Heparin, and Succinylcholine – Sometimes Excellent is the Enemy of Perfect.
- St. Emlyn’s: JC – Rocuronium or Suxamethonium for RSI
- 5Minute Airway: The CUSAMUR Trial – The Roc vs Sux Battle Continues
- EMNerd: The Case of the Adjacent Contradictions
- The Bottom Line: CURASMUR
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)
The post The CURASMUR Trial: Roc Rocks & Sux Sucks? appeared first on REBEL EM - Emergency Medicine Blog.