Background: Face masks can reduce transmission of respiratory viruses by both being a potential physical barrier and by reducing droplet transmission. Additionally, the presence of a mask reduces the users frequency of touching their face which may also reduce transmission. Despite strong, consistent public health messaging about the utility of wearing masks, their use continues to be debated. Both the CDC and WHO strongly recommend the use of masks as a means of source control, but the WHO acknowledges the lack of robust evidence in healthy persons.
Background: Face masks can reduce transmission of respiratory viruses by both being a potential physical barrier and by reducing droplet transmission. Additionally, the presence of a mask reduces the users frequency of touching their face which may also reduce transmission. Despite strong, consistent public health messaging about the utility of wearing masks, their use continues to be debated. Both the CDC and WHO strongly recommend the use of masks as a means of source control, but the WHO acknowledges the lack of robust evidence in healthy persons.
Paper: Bundgaard H et al. Effectiveness of Adding a Mask Recommendation to Other Public Health Measures to Prevent SARS-CoV-2 Infection in Danish Mask Wearers: A Randomized Clinical Trial. Annals of Internal Medicine 2020. [Link is HERE]
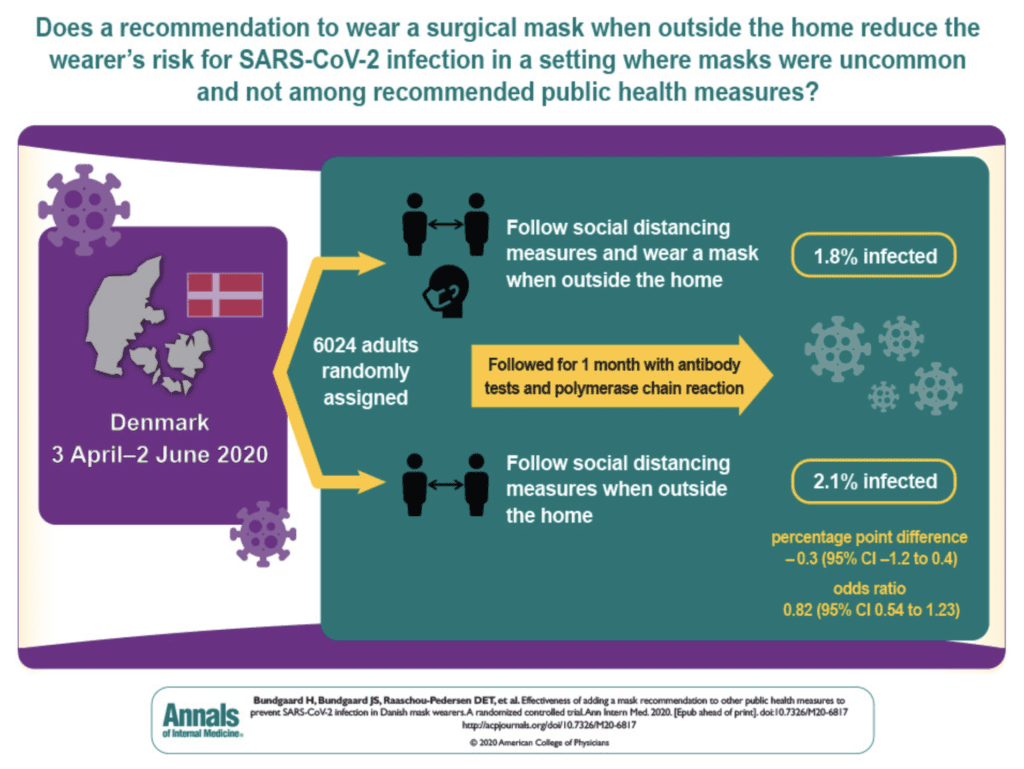
Clinical Question: Does a recommendation to wear a surgical mask outside the home reduce wearers’ risk for SARS-CoV-2 infection compared to not wearing a surgical mask?
What They Did:
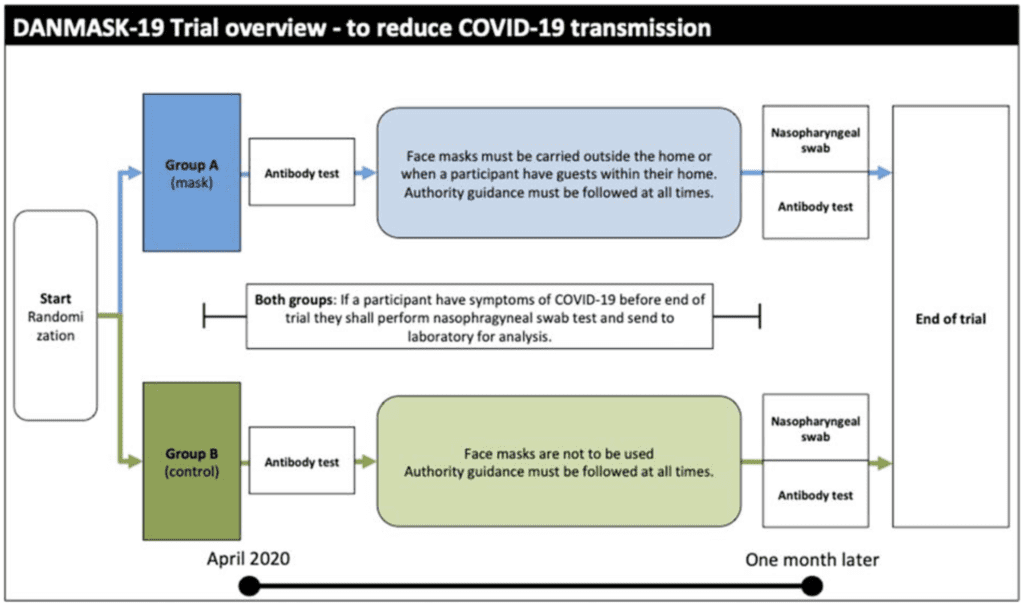
- Investigator initiated, nationwide, unblinded, randomized controlled trial performed in Denmark
- Danish Study to Assess Face Masks for Protection Against COVID-19 Infection (DANMASK-19)
- Recommended public health measures during the study interval included: quarantining persons with COVID-19 infection, physical distancing (including shops and public transportation), limiting the number of persons seen, frequent hand washing, limiting visitors to hospitals and nursing homes. Danish authorities did not recommend mask use for the general public at this time.
- Participants were instructed to change the mask if outside the home for more than 8 hours
- Encouragement to follow social distancing measures for COVID-19, plus either no mask recommendation or a recommendation to wear a mask when outside the home
Outcomes:
- Primary: SARS-CoV-2 infection in the mask wearer at 1 month by antibody testing, PCR, or hospital diagnosis
-
Secondary:
- PCR positivity for other respiratory viruses
Inclusion:
- Adults aged ≥18 years of age
- Spending more than 3 hours per day outside the home
- Did not have occupational mask use
Exclusion:
- Positive antibody test at baseline
- Wear face mask at work
Results:
- 3030 patients randomly assigned to wear masks and 2994 randomly assigned to no mask
- 4862 (80.7%) completed the study
- Participant reported having spent a median of 4.5 hours per day outside the home
- 46% of participants wore the mask as recommended
- 47% wore the mask predominantly as recommended
- 7% did not wear the mask as recommended
- Infection with SARS-CoV-2 (Intention-to-Treat)
- Mask: 42 participants (1.8%)
- No Mask: 53 participants (2.1%)
- Absolute Diff: -0.3%; 95% CI -1.2 to 0.4%; p = 0.38
- OR 0.82; 95% CI 0.54 to 1.23; p = 0.33
- Infection with SARS-CoV-2 (Per-Protocol)
- Mask: 40 participants (1.8%)
- No Mask: 53 participants (2.1%)
- Absolute Diff: -0.4%; 95% CI -1.2 to 0.5%; p = 0.40
- OR 0.84; 95% CI 0.55 to 1.26; p = 0.40
Strengths:
- Asks a clinically important question
- Baseline characteristics were fairly well balanced between groups
- Performed and intention-to-treat analysis and a per protocol analysis which is appropriate as the per protocol analysis excluded patients not wearing masks as instructed
Limitations:
- 52 participants in the mask group and 39 control participants reported COVID-19 in their household. This creates a bias favoring not wearing masks
- It is unclear how well other public health measures were being followed in this trial
- Self-administered tests and self-reported compliance means likely much lower numbers than what is reported
- Trial did not test the role of masks as source control of SARS-CoV-2 infection (i.e. masks preventing acquiring infection not spreading infection)
- Study not powered to see protective effect of masks for other viral infections
- Conjunctival routes of potential infection were not accounted for (i.e. eye protection)
- In patients who wore masks it is unclear if the masks were worn correctly
- Loss to follow-up was 19%
- Relied on patient-reported findings on home antibody tests
- Changed the primary outcome during the study from reduction in COVID-19 infection frequency
Discussion:
- Authors estimated an incidence of SARS-CoV-2 infection of at least 2% and made the assumption that wearing a mask halves risk for infection (i.e. down to 1%). A 50% relative reduction from one intervention is an audacious aspiration to say the least
- The authors simply studied the effect of a recommendation, not of mask wearing itself as evidenced by a <50% compliance rate by report (likely much lower). This study shows us that the public will not necessarily listen to recommendations alone
- The prevalence of disease as well as the density of a population will most likely make a huge impact on how well masks will work. A 2% prevalence of SARS-CoV2 is a low prevalence of disease, most likely making any intervention not helpful
- The results of this study are not surprising. Wearing masks by itself will not get us to 100% in the prevention of COVID-19 transmission. Ensuring other public health measures are also followed becomes additive. Therefore, we wouldn’t expect mask wearing alone to make a huge difference.
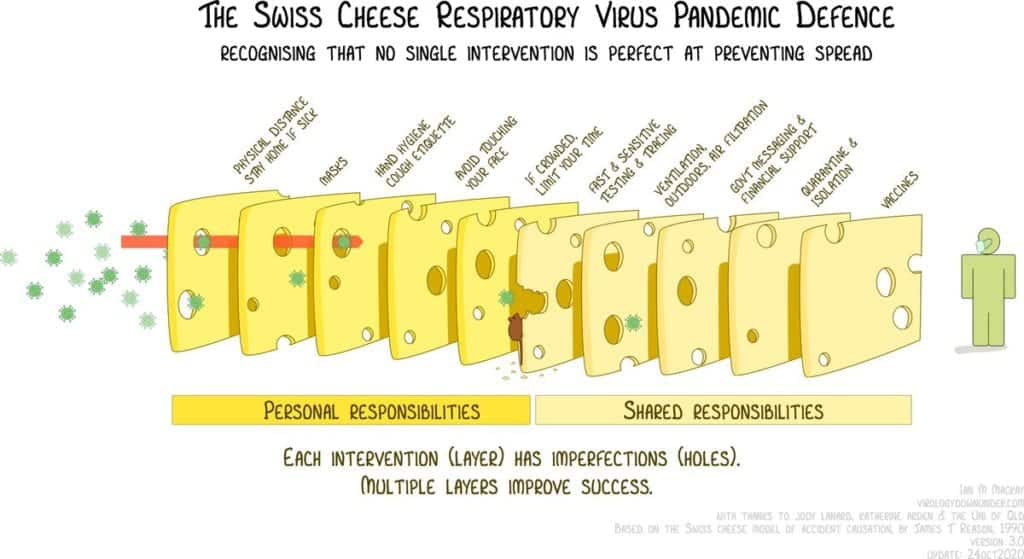
Image from Twitter [Link is HERE]
- Nasopharyngeal swabs were performed by participants at home. How likely is a person to shove a q-tip as far back as it needs to go to get a good sample? We already know what the issues are with the sensitivity of SARS-CoV2 testing (i.e. it is not 100%)
- In the discussion the authors state, “The most important limitation is that the findings are inconclusive, with CIs compatible with a 46% decrease to a 23% increase in infection.”
-
So why did wearing masks not reduce acquiring COVID-19 in this study?
- As stated above, physical distancing, limiting social gatherings, and hand washing are all additive to masks and it may be that if all these things are followed (which they are not) masks may not have as much impact but still add something
- The prevalence of disease was so low that you wouldn’t expect to see much of a difference (Cases of COVID-19 in this trial are far lower than what we are currently seeing in the US)
- The trial really examined the effects of recommending mask use, not the effect of actually wearing a mask
- This trial studied the role of masks as source control of SARS-CoV-2 infection (i.e. masks preventing acquiring infection not spreading infection) which is not the purpose of these masks
- Finally, many have been upset by the publication of this trial, however it is important to publish both positive and negative trials to get closer to the truth of medical practice. The more important point is going through the nuance of the study, instead of just the headlines, which are this is a negative trial. This is actually a negative trial with lots of methodological issues and confounders limiting its results
Author Conclusion: “The recommendation to wear surgical masks to supplement other public health measures did not reduce the SARS-CoV-2 infection rate among wearers by more than 50% in a community with modest infection rates, some degree of social distancing, and uncommon general mask use. The data were compatible with lesser degrees of self-protection.”
Clinical Take Home Point: This trial does not answer the question of “do masks reduce transmission of SARS-CoV-2 infection.” While this is what the researchers sought to study, what they actually studied is the compliance rate with a recommendation to wear masks which was low in this cohort. In a population that predominantly does not wear masks, this trial does not give us information on masks effects with more widespread mask wearing in the community. Additionally, with no clarity on how other public health measures were upheld and whether masks were worn correctly, there are too many confounders that limit the results of this trial. Until better evidence is available, wearing a mask is simple, has minimal harm, and should be recommended at this time.
References:
- Bundgaard H et al. Effectiveness of Adding a Mask Recommendation to Other Public Health Measures to Prevent SARS-CoV-2 Infection in Danish Mask Wearers: A Randomized Clinical Trial. Annals of Internal Medicine 2020. [Link is HERE]
For More Thoughts on This Topic Checkout:
- EM Lit of Note: The Futility of Mask Wearing?
- PulmCrit: Why the DAMASK Trial is a Futile Diversion – The Limitations of RCTs
- The SGEM: SGEM #309 – That’s All Joe Asks of You – Wear a Mask
- The Bottom Line: DANMASK-19
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)
The post The DANMASK-19 Trial: Masks Not Effective to Prevent COVID-19? Not So Fast!!! appeared first on REBEL EM - Emergency Medicine Blog.