
 Background Information: Refractory ventricular fibrillation (RVF) is a complication of cardiac arrest defined as ventricular fibrillation (VF) that does not respond to three or more standard defibrillation attempts.1,2 Patients with RVF during their cardiac arrest have a mortality of up to 97%.3,4 Double external defibrillation (DED) involves the use of a second defibrillator providing an additional shock in a sequential or simultaneous manner. The left ventricle (LV), being the most posterior part of the heart and the furthest away from the anterolateral electrode pads, have led some to hypothesize that utilizing an anterior-posterior pad placement (ie. Changing the vector) is what accounts for DED’s success. Some theorize that the increase in amount of energy from two defibrillations as opposed to one is what’s needed to reach the LV. There are also theories suggesting that the sequential administration of the shocks, more effectively lowers the defibrillation threshold of the cardiac myocytes and thus leads to a more successful conversion of VF. In spite of these many theories, the intervention of DED has been studied for decades in the electrophysiology lab and widely discussed in the literature through case reports and meta-reviews. These case reports have shown success and a recent meta-review of 39 patients who received DED showed that 25% of them were discharged neurologically intact with Cerebral Performance Category (CPC) scores of 2 or less indicating normal recovery/mild disability or moderate disability but able to independently perform activities of daily living.5-10 While this literature is promising, DED is a highly variable intervention and there are still many unknown factors which continue to cause debate and controversy. The role of vector direction via pad placement, the role of a pulse interval in energy deliverance and the efficacy in method of delivering DED sequentially vs simultaneously continues to remain unclear. 6-11 The authors of this pilot RCT (DOSE VF) wished to answer some of these questions by first determining the feasibility and safety of performing a full RCT. In doing so, they used alternate defibrillation strategies such as vector changes and double external sequential defibrillation (DSED) in treating RVF.12
Background Information: Refractory ventricular fibrillation (RVF) is a complication of cardiac arrest defined as ventricular fibrillation (VF) that does not respond to three or more standard defibrillation attempts.1,2 Patients with RVF during their cardiac arrest have a mortality of up to 97%.3,4 Double external defibrillation (DED) involves the use of a second defibrillator providing an additional shock in a sequential or simultaneous manner. The left ventricle (LV), being the most posterior part of the heart and the furthest away from the anterolateral electrode pads, have led some to hypothesize that utilizing an anterior-posterior pad placement (ie. Changing the vector) is what accounts for DED’s success. Some theorize that the increase in amount of energy from two defibrillations as opposed to one is what’s needed to reach the LV. There are also theories suggesting that the sequential administration of the shocks, more effectively lowers the defibrillation threshold of the cardiac myocytes and thus leads to a more successful conversion of VF. In spite of these many theories, the intervention of DED has been studied for decades in the electrophysiology lab and widely discussed in the literature through case reports and meta-reviews. These case reports have shown success and a recent meta-review of 39 patients who received DED showed that 25% of them were discharged neurologically intact with Cerebral Performance Category (CPC) scores of 2 or less indicating normal recovery/mild disability or moderate disability but able to independently perform activities of daily living.5-10 While this literature is promising, DED is a highly variable intervention and there are still many unknown factors which continue to cause debate and controversy. The role of vector direction via pad placement, the role of a pulse interval in energy deliverance and the efficacy in method of delivering DED sequentially vs simultaneously continues to remain unclear. 6-11 The authors of this pilot RCT (DOSE VF) wished to answer some of these questions by first determining the feasibility and safety of performing a full RCT. In doing so, they used alternate defibrillation strategies such as vector changes and double external sequential defibrillation (DSED) in treating RVF.12
Paper: Cheskes S et al. Double Sequential External Defibrillation for Refractory Ventricular Fibrillation: The DOSE VF Pilot Randomized Controlled Trial. Resuscitation 2020. PMID: 32084567
Clinical Question: How feasible and safe is a full scale RCT of alternate defibrillation strategies in treating refractory ventricular fibrillation?
What They Did:
- Three-arm pilot RCT, with a randomized cluster crossing period, conducted across four paramedic services in Ontario, Canada from March 8th, 2018 to September 9th, 2019.
- One of the three following defibrillation strategies was assigned through computer-generated randomization to one of the four regional paramedic services and performed after three standard defibrillation attempts:
- Strategy 1: Continued standard defibrillation therapy with pads in the anterior-lateral configuration
- Strategy 2: Vector change (VC) defibrillation with pads transferred from the standard anterior-lateral to the anterior-posterior position
- Strategy 3: DSED with pads in the anterior-posterior position and an intentional delay to ensure rapid sequence delivery vs simultaneous defibrillation
- Prehospital care was provided by “advanced care” paramedics who perform full ACLS and are assisted by “primary care” paramedics who perform basic life support skills with the addition of a small number of medications and manual defibrillation
- Cluster crossing over meant that each of the paramedic services in the four regions was randomized to one of the three treatment approaches and then crossed over to an alternate defibrillation strategy after 6 months.
- Agencies were informed of their randomization assignment one month prior to allow time for appropriate preparations to start the trial or cross over to another defibrillation strategy.
Inclusion Criteria:
- Adult patients over the age of 18 years old
- Non-traumatic OHCA of presumed cardiac etiology
- Remaining in refractory VF after three standard defibrillation shocks
Exclusion Criteria:
- Traumatic cardiac arrest
- Pre-existing do not resuscitate orders
- Cardiac arrest secondary to drowning, hypothermia, hanging or suspected drug overdose
- Patients presenting in pulseless ventricular tachycardia
Outcomes:
Primary:
- To determine the feasibility and safety for a full scale RCT of alternative defibrillation strategies in RVF by looking at the following three key study logistics and their respective targets:
-
Recruitment
- Enroll an estimated minimum of 110 patients
-
Intervention delivery:
- Successful delivery of the allocated intervention in 80% of eligible patients
-
Protocol Adherence
- 80% of enrolled patients to receive an intervention shock of VC or DSED prior to the sixth shock
-
Recruitment
Secondary:
- Evaluate the effect of the three defibrillation strategies on the outcomes of VF termination and ROSC after 3 standard defibrillations
Results:
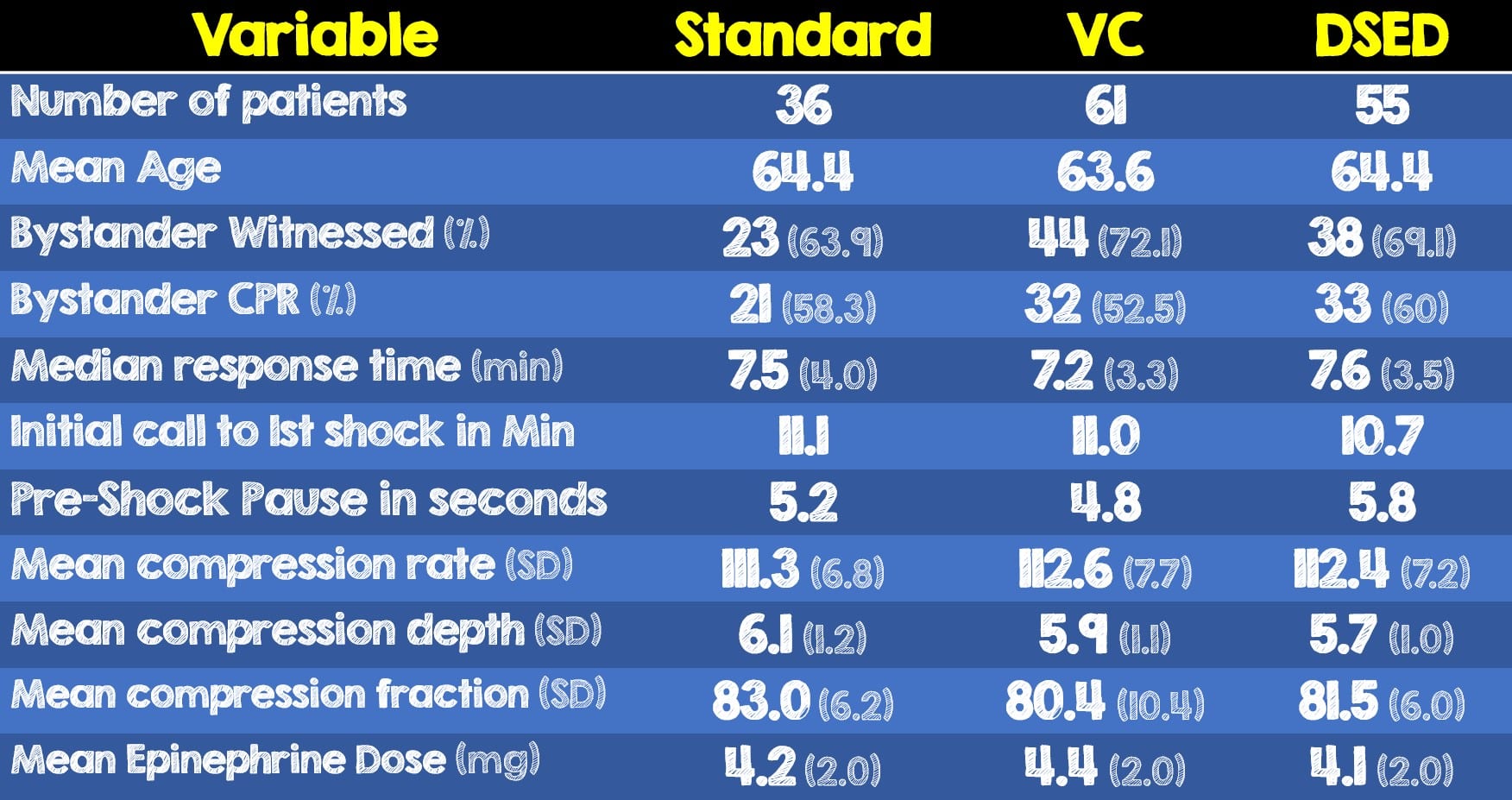
- Recruitment: 152 patients were enrolled at a rate of 12.6 per month with none excluded
- Intervention delivery: 5% of the patients received the defibrillation strategy they were randomized to (89.1% for VC, 83.6% for DSED and 100% for standard defibrillation).
- Protocol adherence:1% of patients received an intervention prior to the sixth defibrillation attempt.
- 77% of patients received an intervention shock at shock 4, the earliest time possible per study protocol
Critical Results:

- Compression qualities of rate and depth was similar across all three groups and compliant with the current AHA guidelines
- There were no reported cases of defibrillator malfunction, skin burns, difficulty with pad placement or concerns expressed by paramedics, families or emergency department staff about the trial.
Strengths:
- First pilot RCT assessing feasibility and impact of alternative strategies of VC and DSED compared to standard defibrillation therapy for refractory VF
- Patients were analyzed with an intention-to-treat analysis which is more like clinical practice as protocol violations can occur in real life
- Zero patients were excluded, lost to follow-up or discontinued intervention
- Attempted to provide insight into a widely debated topic of whether energy or vector play a role in the potential benefit of DSED
- Cluster randomization strategy chosen to maximize efficiency and allow comparison of two new treatments to standardized care in a single three-arm randomized trial.
- Utilized multiple paramedic services in both rural and urban communities in an attempt to accurately reflect these interventions in real practice
- Prior to trial launch, paramedics received standardized in-person training in the techniques of VC and DSED using a combination of one-hour didactic session plus two hours of video and simulated scenarios.
- In addition to the above training, a high level of oversight and paramedic feedback was implemented to ensure high compliance with study protocol.
- Prioritized timing of intervention shocks while maintaining high quality CPR
- The determination of six shocks as being the goal for protocol adherence was derived from prior work showing improved outcomes in earlier defibrillation.13
- Recognized minor modifications in this pilot study that may serve to strengthen the conduct of the main RCT
- The median response times in this study averaged 3.6 minutes which about half the 7-minute national EMS standard in the United States.14
Limitations:
- Enrollment in the standard defibrillation arm was lower than either intervention due to both cluster randomization and the largest enrolling site not being randomized to the standard care strategy during the pilot study
- Although both urban and rural settings were included in the study, the majority of patients were enrolled in the urban setting where a second defibrillator is more readily available.
- The high degree of medical oversight and paramedic feedback may not be possible in all EMS services
- Use of two different models of defibrillators may negatively impact the internal validity of this pilot study
- All energy delivered by the Zoll defibrillators in the first three shocks were lower than the first shock delivered by the LifePak 15 which may serve as a confounding variable as a higher amount of energy delivered earlier may skew results
- Overall mortality and follow-up to determine patient centered outcomes such as neurologic function and return to activities of daily living was not assessed or considered.
- Exclusion of defibrillations performed by the fire department prior to EMS arrival accounted for 28% of enrolled cases and may have underestimated the potential benefit of VC and DSED intervention strategies.
- The EMS system in Ontario, Canada consists of two paramedics able to perform manual defibrillation. Within the United States, due to paramedic shortages, this dual-medic setup does not exist in many EMS systems.
Discussion:
- It’s important to remember that this is a pilot study. The main RCT is already underway with an estimated completion date of September 2022. They are planning to enroll 930 patients. More information can be found here: NCT04080986
- Several theories surround the efficacy of double external defibrillation. Differences in energy delivered, timing between shocks, time to first double defibrillation, and vectors are just some of the factors that play a role in DED success. This study is the first of its kind to factor in vector difference (by intentionally changing pad placement) on the success of DED in terminating VF.
- In addition to the incredibly fast response time, bystander CPR was performed over 50% of the time in all three groups. Furthermore, there was an 11-minute average time from initial call to first shock. These variables indicate a very well-coordinated and efficient EMS system that may have led to an increased survival and success rate when performing DSED. The external validity of this study may be impacted as not all cities, regions or EMS systems can replicate these factors.
- Prehospital intubation was more common with the vector change and DSED groups compared to standard defibrillation (57.4% vs 54.5% vs 38.9%, respectively). Although this doesn’t appear to have detracted from CPR quality in this study, this could affect CPR quality in other systems
- The most common causes of protocol violations were:
- VC Strategy: VF termination after the 4th standard shock while preparing to perform a VC defibrillation
- DSED Strategy: Inability to have a second defibrillator readily available
- The authors did not include or comment on their omission of another common and widely used pad placement arrangement. The anterior-anterior approach has both sets of pads on the front of the patient’s chest but NOT touching (Figure 1). This method is frequently used due to delays in performing DED and/or the inability to access the patient’s posterior chest (active compressions, body habitus, etc).
- Defibrillator models vary in the method they deliver their energy. Some use a Biphasic Truncated Exponential (BTE) or “High-Peak ” waveform (Figure 2) and others a Rectilinear waveform (Figure 3). Due to the impracticality of connecting an oscilloscope during an active cardiac arrest, studies to determine which of these is more efficacious in terminating VF are unable to be performed. Defibrillators using both waveforms were used in this study and thus may have been an unforeseen confounding variable in the DSED intervention strategy.
- Although the authors state that this study helps provide insight into whether energy plays a role in the benefit of DED there are many methodological flaws in this study that makes it difficult to accurately assess the role of energy.
- First, as previously mentioned, double external defibrillation may be performed sequentially or simultaneously depending on the pulse interval between the two shocks.11 The intentional delay utilized in this study’s protocol was purposefully done to ensure all DED attempts were sequential. Omitting an analysis of simultaneous defibrillation limits any kind of speculation that high energy had a role in terminating VF or obtaining ROSC
- Second, one paramedic region’s defibrillators delivered energy at 120, 150 and 200 J for the first three shocks, while a second paramedic region used their defibrillators to deliver 200, 300 and 360 J for the same first three shocks. It is unclear the effect of the variability in amount of energy delivered on the first three initial shocks and therefore are confounding variables.
- Finally, the rectilinear defibrillator model delivered a maximum amount of energy of 200 J, while the BTE defibrillator delivered a maximum of 360 J. The differences in these energy amounts is substantial and is unclear what kind of impact it may have had on the results.
- The variables of VF termination and return of ROSC are not patient centered outcomes. Although a pilot, this study made no mention of important and clinically relevant outcomes such as follow-up to hospital discharge, 30-day mortality, neurologic function, return to activities of daily living. It is unclear and unlikely if one or any of these factors will appear in the main RCT.
- Lastly no damage or defibrillation malfunction was reported throughout this study and the authors justified using a sequential-only approach to DED due to a prior case report which reported damage to their defibrillators following dual defibrillation.15 There are many flaws with this cited case report that has led to a great deal of unfounded fear regarding damaging defibrillators.
- The defibrillators used by the electrophysiologists in the case report were both two different brands each having a BTE and rectilinear waveform as mentioned above
- While it has been performed before, DED is NOT indicated for ventricular tachycardia let alone synchronization. In fact, hitting the “sync button” is the WORST thing that could be done if trying to avoid defibrillator damage. There is a vulnerable period a defibrillator goes through after delivering a shock so it can perform an internal analysis. Another shock being delivered at a very specific time (ie. cardioversion) will revert back to the resistor of that first defibrillator when isn’t expecting that much energy in the first place (ie. Vulnerable period) and thus will overload its resistor. The defibrillator senses this, just like the authors mentioned in the case report, produces the message “Abnormal energy delivered”, and likely resulted in the malfunctioning of the device
- To conclude this damage was due to the use of two defibrillators for an arrhythmia that isn’t indicated for and not considering all of the confounding variables is premature.
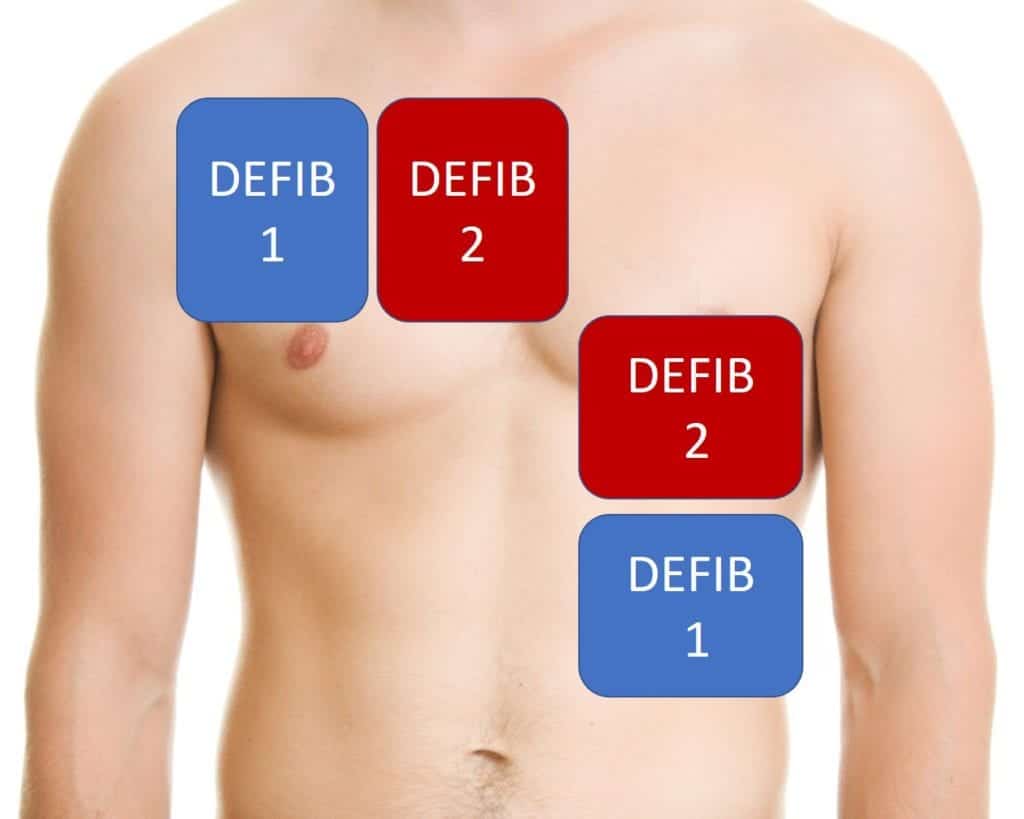
Figure 1: Anterior-Anterior pad placement for double external defibrillation where pads are NOT touching and there remains space for compressions
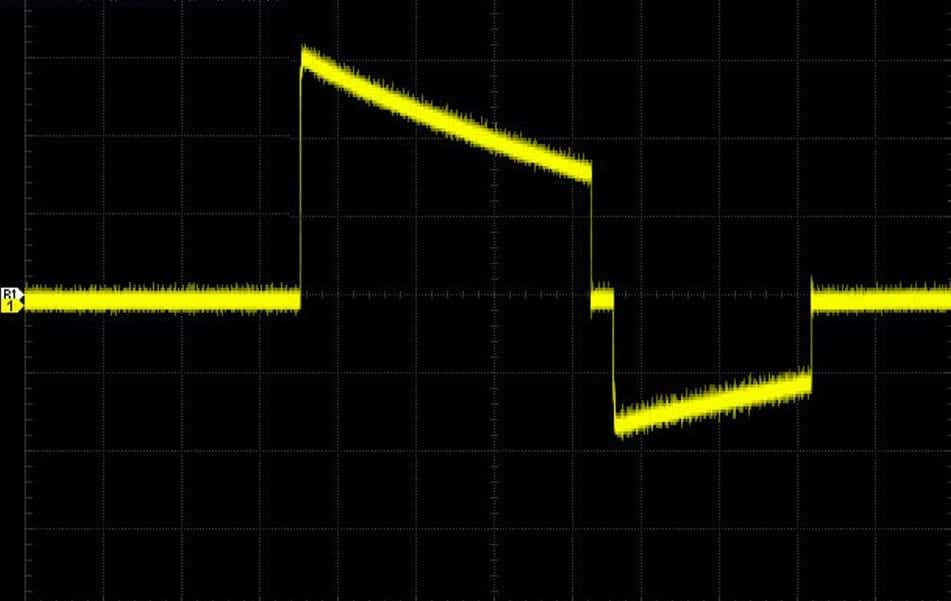
Figure 2: Oscilloscope depicting a Biphasic Truncated Exponential (BTE) or “High-Peak” defibrillator waveform
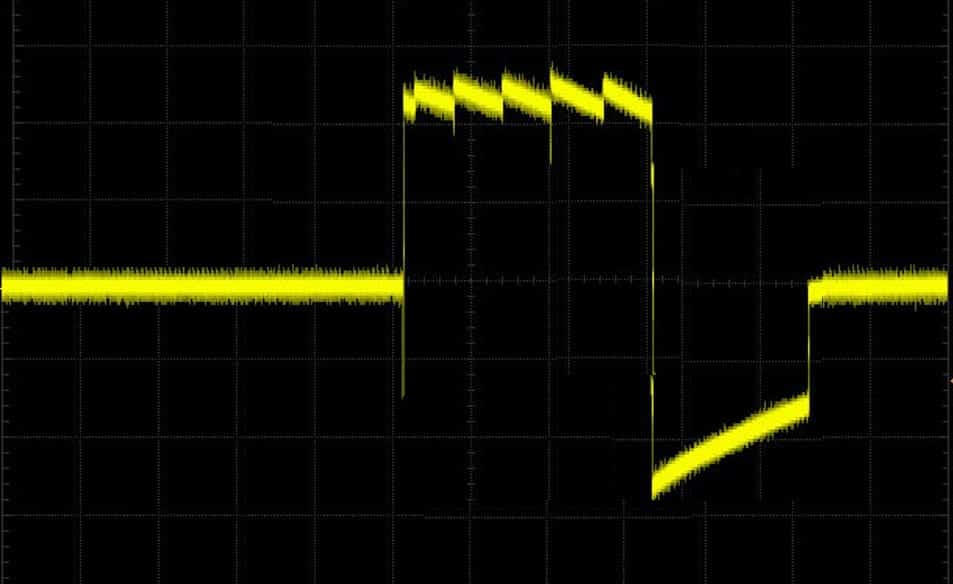
Figure 3: Oscilloscope depicting a rectilinear defibrillator waveform
Author’s Conclusions:
- Our findings suggest the DOSE-VF protocol is feasible and safe. Rates of VFT and ROSC were higher in the VC and DSED than standard defibrillation. The results of this pilot trial will allow us to inform a multicenter cluster RCT with crossover to determine if alternate defibrillation strategies for refractory VF may impact clinical outcomes.
Our Conclusion:
- Although a pilot study, the findings of this RCT are promising regarding the role of VC and DSED on VF termination and achieving ROSC. Unfortunately, several methodological flaws still leave many questions unanswered regarding DED. More importantly the impact DED has on patient centered outcomes (ie. mortality, survival to discharge, return to functional activities of daily living, etc) is not addressed and is unclear if it will be in the main RCT. The authors have successfully displayed that a double defibrillation RCT is safe and feasible, however they should consider limiting the number of confounding variables and adding a follow-up component to identify DED’s role in patient centered outcomes.
Clinical Bottom Line:
- Emergency physicians should continue to consider the use of a second defibrillator when treating refractory ventricular fibrillation. It isn’t clear from this study if increased ROSC will translate into improve neurologically intact survival. In settings where a second defibrillator is not available or not feasible, changing pad placement from anterolateral to anteroposterior when performing defibrillation may help improve VF termination and achievement of ROSC.
For More on This Topic Checkout:
- REBEL EM: Dual Sequential Defibrillation (DSD)
- REBEL EM: Beyond ACLS: Dual Simultaneous External Defibrillation
- EmCrit: Dual External Defibrillation: Close but Not Touching
- First10EM: Double Sequential Defibrillation (The DOSE VF Trial)
References:
- Eifling M, et al. The evaluation and management of electrical storm. Tex Heart Inst J 2011; PMID: 21494516
- Sakai T, et al. Incidence and outcomes of out-of hospital cardiac arrest with shock-resistant ventricular fibrillation: data from a large population-based cohort. Resuscitation. 2010; PMID: 20653086
- Windecker S, et al. Percutaneous left ventricular assist devices for treatment of patients with cardiogenic shock. Curr Opin Crit Care 2007; PMID: 17762230
- Herlitz J, et al, Rhythm changes during resuscitation from ventricular fibrillation in relation to delay until defibrillation, number of shocks delivered and survival. Resuscitation 1997; PMID: 9051819
- Sena R, et al. Refractory Ventricular Fibrillation Successfully Cardioverted With Dual Sequential Defibrillation. J Emerg Med. 2016; PMID: 27369859
- Bell C, et al. Make it two: A case report of dual sequential external defibrillation. CJEM. 2017; PMID: 28587703
- Boehm K. et al. First Report of Survival in Refractory Ventricular Fibrillation After Dual-Axis Defibrillation and Esmolol Administration. Western Journal of Emergency Medicine. 2016; PMID: 27833686
- El Tawil C, et al. Double sequential defibrillation for refractory ventricular fibrillation. Am J Emerg Med. 2017; PMID: 28978402
- Leacock B, Double Simultaneous Defibrillators for Refractory Ventricular Fibrillation. J Emerg Med. 2014; PMID: 24462025
- Hajjar K et al. Dual defibrillation in patients with refractory ventricular fibrillation. Am J Emerg Med 2018. PMID: 29730094
- Hamilton R, Ramzy M. et al.Dual defibrillation is highly variable: an analysis of pulse interval delivered in dual defibrillation. Prehospital Emergency Care. 2019 PMID 31116612
- S. Cheskes, et al. Double sequential external defibrillation for refractory ventricular fibrillation: The DOSE VF pilot randomized controlled trial. Resuscitation 2020; PMID: 32084567
- Cheskes S, et al. The impact of double sequential external defibrillation on termination of refractory ventricular fibrillation during out-of-hospital cardiac arrest. Resuscitation 2019. PMID: 31059670
- Mell, H. et al. Emergency medical response times in rural, suburban and urban areas JAMA Surgery 2017. PMID 28724118
- Gerstein NS, et al. External defibrillator damage associated with attempted synchronized dual- dose cardioversion. Ann Emerg Med 2018 PMID: 28559035
Post Peer Reviewed By: Salim R. Rezaie, MD (Twitter: @srrezaie)
The post The DOSE VF Pilot RCT: Double Sequential External Defibrillation for Refractory Ventricular Fibrillation appeared first on REBEL EM - Emergency Medicine Blog.
